Folliculocentric hyperkeratotic lichen sclerosus in a 7-year-old child successfully treated with narrowband ultraviolet B phototherapy
Abstract
Click here for the corresponding questions to this CME article.
Lichen sclerosus (LS) is an inflammatory skin disorder, which was first described by Hallopeau in 1887 as an atrophic variant of lichen planus.1 The aetiopathogenesis of LS is not clear, but it is strongly associated with other autoimmune disorders.2 Clinically, LS is characterized by white opalescent macules, usually anogenitally, which may coalesce and lead to atrophy.3 Primarily prepubertal, perimenopausal and postmenopausal women are affected; the female : male ratio is 10 : 1 for genital disease,1 whereas extragenital disease affects men and women equally. Approximately 15% of LS cases are seen in childhood.2
A 7-year-old girl presented with a 2-year history of white, asymptomatic lesions on her trunk and limbs (Fig. 1).

On physical examination, widespread, folliculocentric, hyperkeratotic and hypopigmented papular lesions were seen on the patient's trunk, arms and legs. She was otherwise well, and the differential diagnoses considered included LS, anetoderma, vitiligo and mycosis fungoides (MF).
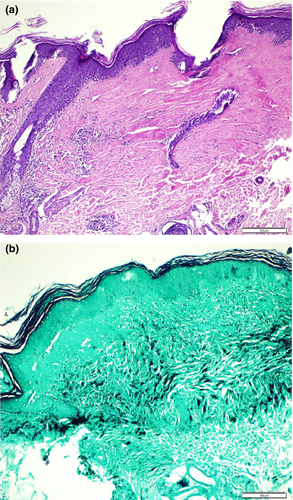
Histological examination of a 4-mm punch biopsy demonstrated hyperkeratosis, focal parakerosis, mild acanthosis, basal vacuolar degeneration and elastic fibre loss in the papillary dermis (Fig. 2a,b).
Based on the clinical and histopathological findings, a diagnosis of folliculocentric LS was made, and narrowband ultraviolet B phototherapy was initiated. After 20 sessions, the lesions regressed (Fig. 1b), and no recurrence was detected 6 months post-treatment.
Extragenital LS occurs in 6% of children with LS, occurring predominantly on the neck, arms and upper trunk, and to a lesser extent on the scalp, face, palms and soles. It may start at any age, but is rare in childhood.2
Classically, extragenital LS is characterized by polygonal, blue/grey/white, slightly elevated papules with comedo-like follicular plugging, which coalesce into plaques and become increasingly atrophic over time. Bullous, erythematous, pigmented, keratotic or folliculocentric forms of extragenital LS have also been reported in the literature.2, 4-6
The folliculocentric hyperkeratotic variant of LS is very rare, and is characterized clinically by shiny, hypopigmented macules with follicular scale (Fig. 1).6 This type of LS is differentiated from classic extragenital LS mainly by its clinical morphological appearance. In line with the previous case reports in the literature, we did not see distinct follicular involvement in the histology. The differential diagnosis of this folliculocentric hyperkeratotic rash includes MF, anetoderma, psoriasis, parapsoriasis, pityriasis lichenoides chronica, pityriasis rubra pilaris and lichen spinulosus. The absence of the typical atrophy, both clinically and histopathologically, and the presence of generalized involvement may lead to difficulty in distinguishing this variant from classic LS. Histological findings of this variant are similar to those of classic extragenital LS.2, 5 All forms of LS typically show elastic fibre loss in the papillary dermis but this is more prominent in later stages. Psoriasiform, lichenoid or vasculitic-like findings may also be present. In our patient, epidermal atrophy was not marked, but rete ridge flattening, dermal lichenoid infiltration and elastic fibre loss were consistent with the diagnosis of LS.
Topical therapeutic options in LS include topical corticosteroids, retinoids, calcineurin inhibitors and sex hormones. Topical or systemic retinoids and photodynamic therapy are other treatment options. In cases of generalized or recalcitrant disease, possible options include pulsed corticosteroids and methotrexate in combination, phototherapy with narrowband UVB, PUVA or UVA1, and pulsed dye laser.2 We opted for narrowband UVB phototherapy because of the patient's age and the distribution of the lesions.
In conclusion, we present this case to highlight this rare folliculocentric variant in the paediatric population and demonstrate the effectiveness of phototherapy.
References
CPD questions
Learning objective
To gain knowledge of the characteristics and treatment of lichen sclerosus.
Question 1
Which of the following statements about lichen sclerosus (LS) is correct?
- (a) LS has a predilection for the acral region, and results in parchment-like atrophic skin.
- (b) LS is an inflammatory disorder, predominantly affecting the face, limbs and acral areas.
- (c) LS predominantly affects the paediatric population.
- (d) Extragenital LS can present with keratotic, pigmented, bullous or folliculocentric lesions.
- (e) LS primarily affects young adult males.
Question 2
What treatment options have been reported as unsuitable for generalized lichen sclerosus (LS)?
- (a) Phototherapy.
- (b) Systemic retinoids.
- (c) Systemic corticosteroids.
- (d) Methotrexate.
- (e) Ablative lasers.
Instructions for answering questions
This learning activity is freely available online at http://www.wileyhealthlearning.com/ced
- Read the article in print or online, paying particular attention to the learning points and any author conflict of interest disclosures
- Reflect on the article
- Register or login online at http://www.wileyhealthlearning.com/ced and answer the CPD questions
- Complete the required evaluation component of the activity
Once the test is passed, you will receive a certificate and the learning activity can be added to your RCP CPD diary as a self-certified entry.
This activity will be available for CPD credit for 2 years following its publication date. At that time, it will be reviewed and potentially updated and extended for an additional period.