Multiple intracranial hemorrhages in a postmenopausal female
Xinhua Lu and Xinya Xu contributed equally to this work.
BOX 1. Virtual glass slide
Access at https://isn-slidearchive.org/?col=ISN&fol=Archive&file=BPA-24-11-CIR-339-A.svs and https://isn-slidearchive.org/?col=ISN&fol=Archive&file=BPA-24-11-CIR-339-B.svs
1 CLINICAL HISTORY AND IMAGING
A 53-year-old postmenopausal female presented to the neurology clinic with acute onset of right arm weakness for 1 week. Neurologic examination was notable for 4/5 strength in the right upper extremity. Computed tomography revealed multiple hematomas with mass effect in the left frontal lobe and basal ganglia (Figure 1A; Box 1). Magnetic resonance imaging with gadolinium showed multiple heterogeneously enhancing lesions associated with surrounding edema, mass effect, and midline shift (Figure 1B). Given the absence of an overt primary source for the hemorrhagic mass with elevated intracranial pressure and neurologic deficits, surgical excision of the left frontal lobe lesion was performed. Intraoperatively, the mass showed evidence of prior hemorrhage and was noted to encase a relatively large vessel. Postoperative CT imaging showed gross total resection of the frontal lesion and found a new lesion adjacent to the left lateral ventricle (Figure 1A inset). Of notice in the past medical history, the patient had undergone hysterectomy 3 years earlier. After a final diagnosis was reached, adjuvant treatment was performed with stereotactic radiosurgery (SRS) and chemotherapy. At 10 months of follow-up, the patient's symptoms have resolved.

2 FINDINGS
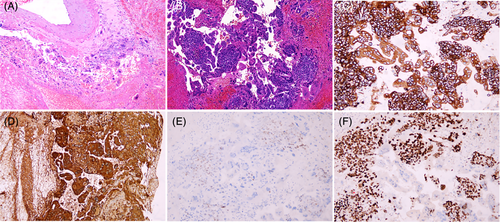
Hematoxylin–eosin stain showed that several pieces of tissue mingled together with a lot of blood. There was no normal brain parenchyma found. Small clusters of atypical cells made up of uninucleate and multinucleated cells were embedded in the hemorrhagic material. These were big cells with clumped chromatin, noticeable nucleoli, uneven nuclear outlines and nuclear-cytoplasmic ratios, and a modest proportion of amphophilic cytoplasm. Eosinophilic hyaline globules were seen in a large number of the cells. Mitoses were present (Figure 2A,B). Moreover, we saw atypical cells infiltrating relatively large vessels (Figure 2A) and some small vessels. Looking carefully into the previous history of hysterectomy, we found the diagnosis of complete hydatidiform mole, which led us to consider the possibility of metastatic gestational trophoblastic neoplasia (GTN). The atypical cells were strongly and diffusely positive for CK7 (Figure 2C) and β-HCG (Figure 2D), slightly immunopositive for SALL-4 (Figure 2E) on immunohistochemical examination. Ki-67 displayed a high proliferative index (approximately 60%, Figure 2F).
3 FINAL DIAGNOSIS
Metastatic gestational choriocarcinoma following complete hydatidiform mole.
4 DISCUSSION
Multiple intracranial hemorrhages can be due to a variety of causes, including hypertension, cerebral amyloid angiopathy (CAA), primary or secondary CNS vasculitis, hematologic disorders, anticoagulant use, sinus thrombosis, and brain tumors, most frequently metastatic. In this patient, normotensive, young for CAA, and overall only apparently without a significant past medical history, multiple hemorrhagic lesions on MRI led to the suspicion of brain metastases. Once discovered, the previous diagnosis of complete hydatidiform mole prompted immediate consideration of metastatic gestational trophoblastic neoplasia (GTN) following complete hydatidiform mole.
Gestational trophoblastic disease (GTD) is a group of interrelated diseases, characterized by cellular proliferations in the placental villous trophoblast, including hydatidiform moles (complete and partial) and GTN (invasive mole, choriocarcinoma, placental site trophoblastic tumor, epithelioid trophoblastic tumor, and mixed trophoblastic tumor). Choriocarcinoma is the most malignant GTN and can occur during any type of pregnancy, including abortion, term or preterm gestation, tubal pregnancy, or hydatidiform moles. It is estimated that 2%–3% of complete moles and 0.5% of partial moles progress to choriocarcinoma [1]. Choriocarcinoma can metastasize early due to hematogenic spread of trophoblastic tissue. Symptoms are typically associated with bleeding from the metastatic center. Lung metastases are prevalent (80% of cases), while only in 3% to 21.4% of cases will choriocarcinoma metastasize to the brain, with greater morbidity and mortality due to intraparenchymal bleeding [2] Brain metastases often present with multiple hemorrhagic space-occupying lesions, associated with infiltration of the vascular wall, causing bleeding inside the tumor mass or formation of fusiform cerebral aneurysms that may burst, resulting in intracerebral or subarachnoid hemorrhage.
In our patient, CT and MRI imaging showed multiple intracranial hemorrhagic masses. Histopathological examination showed syncytiotrophoblast and cytotrophoblast cells surrounded by areas of necrosis and hemorrhage typical of choriocarcinoma. With a combination of multinucleated cells and somewhat amphophilic cytoplasm, the cells have an odd nuclear cytomorphology. The atypical cells showed vascular wall infiltration, likely the cause of multiple hemorrhages. Immunohistochemical staining for β-HCG confirmed the origin of the tumor cell.
This case is unique in terms of both treatment techniques and prognosis. For choriocarcinoma with cerebral metastases, there are currently no guidelines on treatment techniques for these individuals [3]. In our case, the patient subsequently received craniotomy, SRS, and chemotherapy. At 10 months of follow-up, the patient's symptoms have resolved, and the β-hCG level decreased from 31,289 to 0.25 mIU per milliliter (reference value, <2.9).
AUTHOR CONTRIBUTIONS
Xinhua Lu drafted the manuscript. Xinya Xu and Xiaopeng Zhang reviewed and edited the draft. All the authors approved the final version of the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.