A blueprint for pursuing therapeutic interventions and early phase clinical trials in clonal haematopoiesis
Tamanna Haque and Aditi Shastri contributed equally to this study.
Summary
The age-associated mutational state of clonal haematopoiesis (CH) is linked to multiple adverse health outcomes. As higher risk CH can lead to progressive neoplastic or vascular disease, there is interest in developing clinical trials to mitigate risk associated with CH. Given the high prevalence of CH, data from clinical trials could have broad public health implications for screening and therapy. Thoughtful consideration is needed to design trials that are both clinically relevant and avoid overmedicalization. Here, we summarize clinical studies of CH to date and provide suggestions and guidance on how to approach designing CH-focused therapeutic clinical trials. These recommendations are derived from discussions among clinical researchers and scientists emanating from the Inaugural Meeting on Somatic Mutations and Predisease in October 2021.
BACKGROUND: BUILDING A CASE FOR THERAPEUTIC INTERVENTION
Definitions
Clonal haematopoiesis (CH) is a somatic mutational event arising from an error in genomic replication within a small number of clonal haematopoietic stem cells.1 While CH is present in nearly all adults at small variant allele frequencies (VAF),2 CH of indeterminate potential (CHIP) refers to a growth of clones to a clinically meaningful size, usually considered ≥2% VAF.2, 3 CHIP occurs recurrently in a relatively small number of genes which are also commonly mutated in myeloid malignancies.1, 2, 4-6 CHIP is more commonly detected with increasing age (>10% over age 70), male sex and a history of tobacco smoking.1, 4, 5, 7 CHIP is associated with an increased risk of developing a haematological malignancy (~0.5% per year) and an increased all-cause mortality, mostly from adverse cardiovascular events.5, 8 Beyond cardiovascular disease, higher rates of CH have been implicated in other medical conditions, including chronic inflammatory diseases.9 The most commonly mutated genes in CH are DNMT3A, TET2 and ASXL1 (DTA), all of which alter epigenetic patterns and chromatin conformation, influencing transcriptional profiles.1, 4, 5, 7
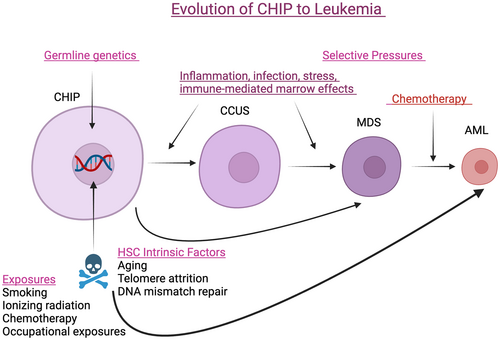
While the risk of transformation of CHIP to an overt malignancy remains small in the general population, several studies have explored predictors of a higher risk. In one study, nearly 75% of acute myeloid leukaemia (AML) patients who had sequencing performed on pre-AML blood samples had somatic mutations detectable before AML diagnosis in putative driver genes.10 Having a greater number of mutations at a younger age, higher VAF and CHIP-specific mutations including U2AF1, SRSF2, SF3B1 or TP53 were associated with an increased risk of progression to AML.10 Similarly, the presence of CH mutations in a Women's Health Initiative study found that higher VAF (>10%), mutations in IDH1, IDH2, TP53, DNMT3A, TET2 or spliceosome factor genes increased the probability of developing AML.11
Clonal cytopenia(s) of undetermined significance (CCUS) is a term used to describe CH in conjunction with clinically relevant blood cytopenias.3, 12 While CCUS is heterogeneous, it is associated with decreased overall survival (OS) and course similar to that of patients with lower risk myelodysplastic syndromes (MDS, expanded as myelodysplastic neoplasms in the 2022 World Health Organization classification).3, 13 CCUS progression risk appears higher with non-DNMT3A/TET2 mutations such as spliceosome mutations, high VAF and the presence of multiple mutations.14, 15 While CCUS usually connotes an increased risk over CH alone, some individuals with CCUS (e.g. DTA single mutants with low VAF and mild cytopenias) have a low risk of transforming into an overt myeloid malignancy (Figure 1). Determining which individuals with CH are at risk for disease progression is critical. Early intervention in this subset is most desirable if disease progression a be prevented, as progression to MDS and AML is often incurable with currently available treatment.16
Risk stratification: Not all CH mutations have the same leukaemogenic potential
People are discovered to have CHIP when genetic sequencing is performed on blood in individuals without known blood disorders, either as part of testing for non-myeloid cancer (e.g. cell-free DNA), during testing for germline predispositions to breast cancer and other neoplasms, or during cardiovascular risk evaluation including polygenic risk score assessment.17-19 CHIP can be discovered by clinicians who are unfamiliar with counselling, which has led to the development of many CHIP-focused clinics at large referral centres. Early reports described the logistics, goals and challenges of such a clinic as well as the benefits of prospective evaluation and counselling from specialists.20, 21 There is currently no clear recommended screening or monitoring criteria.
In an effort to define risk factors associated with CHIP that predispose towards the development of myeloid neoplasia (MN), Weeks et al. analysed sequenced exomes of healthy U.K. Biobank (UKBB) participants and developed the CH risk score (CHRS).22 Important determinants of risk were single DNMT3A mutations, high-risk mutations, two or more mutations, a VAF of ≥20%, age ≥65 years, having CCUS versus CHIP and abnormal red blood cell indices including mean corpuscular volume and red cell distribution width.22 CHRS correlated not just with progression to MN but also with OS and risk of ischaemic cardiovascular disease.22 Similarly, the MN prediction system utilized annotated genetic data from the UKBB to outline time-dependent risk of transformation to specific haematological malignancies including MDS, myeloproliferative neoplasms and AML.23 The clonal cytopenia risk score was developed by performing multivariate analysis on multicentre CCUS patient data and uses three variables (thrombocytopenia, presence of splicing factor mutations and ≥2 mutations) to calculate a score that predicts CCUS progression risk to an overt MN.24 While large population databases were used to describe incidence of CHIP and clinical associations, recognition of CHIP in real-world clinical practice more often occurs in patients who have reason for genetic testing, thus accounting for an increased rate of CCUS and non-MN. Nonetheless, CHRS is still useful in the prediction of progression of CHIP to MN,25 and other prognostic systems will be validated in this context as well to help identify higher risk individuals who might benefit from participation in CH intervention trials.
Attempts to develop guidelines for the management of individuals with CH, such as determining who might be at higher risk for malignant progression, are underway.21 Accumulating real-world clinical outcomes data for people with CH is refining risk evaluation, and therapeutic intervention may be indicated in select subpopulations at higher risk for an adverse event. There is currently a lack of consensus on therapeutic intervention for CHIP, including clarity on which subpopulations to treat, the investigational interventions, the goals and objectives in early intervention and validated end-points to measure that potential benefit.
PRINCIPLES OF DESIGN FOR INTERVENTIONAL CLINICAL TRIALS FOR CHIP
The major impetus for pursuing therapeutic intervention in CHIP and CCUS is to prevent progression to an overt malignancy or to reduce the risk and severity of potential adverse non-haematological outcomes, particularly cardiovascular disease. Since most individuals with CHIP will not progress to an MN within their lifetime, it is critical that interventions pursued in prospective trials are risk-informed, age appropriate and pose minimal toxicity. Given the increasing number of mechanistic studies, population health-based approaches and multivariate risk prediction tools, the following sections will highlight key considerations in designing clinical trials for secondary or tertiary prevention in individuals with CHIP/CCUS.
Detecting CHIP
While common in the general population in large cohort studies, most people with CH in clinical practice today are managed within academic research centres by oncologists, geneticists, haematologists and cardiologists within established CHIP clinics. The assays that detect CH, generally error-corrected sequencing or c-DNA testing, will differ based on institution, with varying depth, quality and reproducibility of results. Assays may have varying numbers of genes detected, potentially missing clinically relevant or understudied mutations. Confirmatory germline testing may not be routinely performed at all centres. Whole genome sequencing and whole exome sequencing used in research assays are not available in clinical practice. The variation of testing modalities brings to forefront the need to consider standardized clinical testing approaches to do large-scale prospective studies feasible and generalizable.26 As technology improves, historical data will need to be re-analysed, and partnering with multiple institutions, federal authorities and/or industry may be needed for far reaching harmonization of detection within samples. In addition, large-scale testing and novel approaches to conduct gene testing more efficiently may lower costs, making testing accessible to a broader population in both clinical practice as well as in practical collaborative research opportunities.27
Patient selection
Defining the intended treatment population is a particularly important in clinical trials in which participants are healthy individuals. Criteria for selecting individuals with CH to be considered for clinical intervention should be predefined to ensure safety and interpretability between studies. Selection criteria should first and foremost be risk-informed, selecting populations with high-risk genomic features, clinically relevant cytopenias or high cardiovascular risk profiles. Examples of a selected CH population may be by a specific high-risk feature, such as a specific mutation (such as TP53); by number of mutations (more than 2); or by a high VAF (such as >10%).10, 11 Other features that may be of interest may be those with CH and predisposing cardiovascular risk factors, or CH and those undergoing intensive chemotherapy.14 Future studies may also choose specific populations, such as an older population, or those with a specific comorbidity such as autoimmune disease that is associated with higher rates of CH.28-38 Efforts to homogenize eligibility criteria across different planned clinical studies will help validate the future implementation of therapeutic interventions. In other haematological malignancy precursor conditions such as smouldering myeloma, the lack of uniform entry criteria had been recognized as a barrier to implementation of potentially effective interventions.39-41
Risk of progression to an adverse outcome may also affect population choice. Using a standardized approach for assessing risk, especially in a community/population setting, may be helpful in making clinical decisions for eligibility. An attractive stepwise approach may be choosing the highest risk patients for initial studies, such as individuals with CHIP who already have cardiovascular disease as tertiary prevention, prior to treating lower risk CHIP patients as secondary prevention, as the tolerance for adverse events in such a setting is lower. However, criteria should also be dependent on the goal/intent of the intervention. For example, enrolling extremely high-risk individuals for prevention studies may work against the intervention if the intent is prevention and the disease process is too advanced to halt. Risk stratification for therapy will change as more prospective cohorts are analysed.
Identification of patients as potential clinical trial candidates is essential to ensure robust accrual. Patients with CCUS are often referred to haematologists; however, individuals with asymptomatic CHIP may be identified by medical oncologists, geneticists, primary care physicians, cardiologists or others that are not necessarily seen in a setting where trial enrolment is feasible. While many centres have developed CHIP clinics, some referred patients have competing risks including solid tumours more urgently requiring therapy and these patients may not be appropriate candidates for an interventional secondary or tertiary prevention study. A high incidence of CHIP (~25%) in patients evaluated in the cardiac catheterization lab suggests that this population might be appropriate for more systematic screening, and potential enrolment into interventional protocols.19, 36, 42 Older adults, a group inherently enriched for CH, can be insufficiently included in clinical trials despite explicit Federal Drug Administration (FDA) guidance regarding their inclusion.43 It also important to consider how the exclusion criteria may affect enrolment (e.g. excluding those with solid tumours from participating in a CHIP study).
CH may have different epidemiology across populations, and representation of diverse groups is important in interventional studies. The largest data sources defining the spectrum of mutations and epidemiology of CHIP are from European populations (e.g. UKBB) or from US-based cohorts with a majority of persons of European descent. In these cohorts and others, CHIP has been observed to have differential prevalence in different populations.5, 8, 26, 44 In particular, Hispanic individuals have been identified as having lower rates of CHIP than European individuals.45 The basis for these differential prevalence is incompletely understood and likely has both genetic and environmental contributors. Several studies have identified germline genetic variants that are enriched in different populations as conferring differential risk of CHIP.46 For example, the JAK2 46/1 risk haplotype that is associated with an increased risk of JAK2-mutated CHIP (and MPN) is more common in Northern European ancestry individuals than other populations.46 A germline variant in a distal enhancer of TET2 that increases the risk of CHIP is more common in African Americans.44 Although each of these individual germline variants confers a very small increased or decreased risk of CHIP, it is possible that, in aggregate, they contribute to differential population risk and warrant further study.
It is critical to keep in mind that most CH is incidental, may never need treatment and, in some situations, may provide clonal fitness and protection from certain diseases. Progressive haematopoietic oligoclonality is inescapable with ageing and mutations in such epigenetic modifiers as DNMT3A and TET2 may be necessary to maintain adequate haematopoietic output in the setting of ageing-associated stem cell attrition.47 CH has been associated with the decreased rates of Alzheimer's dementia, particularly at higher CH VAF burden, and may be related to a more efficient microglial replacement.47, 48 CHIP does not seem to have a meaningful impact in key areas intuitively thought to be associated with increased risk. For example, there was no difference in the rates of CH among patients with sickle cell anaemia compared to age-matched controls, including in those treated with hydroxyurea.49 In the context of allogeneic haematopoietic cell transplant, donor CH was associated with improved outcomes in the recipient in one study50 and, in another, had no net effect on outcomes51; while recipient CH had no effect on long-term transplant outcomes,52 and inferior progression-free survival in another.53 It is possible that heterogeneity of studies or populations lead to these discrepant findings, but currently the impact of CH on allogeneic stem cell transplant is unclear.54 There is an increase in TET2-mutant CHIP in solid-organ transplant recipients not due to an increased risk of receiving a transplant in the first place.55 While this may be partly explained by a clear correlation between certain types of immunosuppression and emergence of TET2-mutant CHIP, there is also evidence from a preclinical mouse model of cardiac transplant that TET2-null haematopoietic cells promote allograft tolerance, although no such association has been described in the limited number of clinical cohort studies completed to date.56 These studies suggest there exists subsets of CH that are better left alone, particularly when not associated with any cytopenias (Table 1).57-60
| Lower risk CHIP/CCUS | Higher risk CHIP/CCUS | |
|---|---|---|
| Selected study objectives |
|
|
| Selected study interventions |
|
|
- Abbreviations: CCUS, clonal cytopenia(s) of undetermined significance; CHIP, clonal haematopoiesis of indeterminate potential.
- a To date, there is no clear consensus on defining features for lower risk and higher risk CHIP/CCUS.
Selecting the right therapeutic end-points
In pursuing interventions for a predisease state, it is important to highlight the expected outcomes, the timeframe and clinical significance the intervention would have on subject outcomes, which can be challenging. While OS is a critical end-point, this is likely to be difficult to measure in CH trials given the low risk of a death event during the first years of follow-up, and competing risks in an elderly population that would be enriched for persons with CH. Relevant alternative clinical end-points measurable within a shorter timeframe include progression to MN, improvement of clinically significant cytopenias and major adverse cardiac events (MACE) (Table 2). Measuring time to progression to MN would not describe the severity of MN as OS would; for example, low-risk MDS and TP53-mutated MN have strikingly different clinical courses.
| End-point | Study duration | Indications | Limitations |
|---|---|---|---|
| Overall survival | Decades | Establishes clear clinical benefit |
|
| MN-free survival | Years | Establishes clear clinical benefit |
|
| Time to MACE or incidence of other associated chronic disease | Years | Would establish clear clinical benefit |
|
| Haematologic improvement | Weeks to months | Establishes clear clinical benefit as long as clinical symptoms and transfusion independence is established |
|
| Reduction in clone burden (measured by VAF) | Months to years | Possible surrogate end-point to MN development and haematologic improvement respectively |
|
| Reduction in inflammatory biomarkers | Weeks to months | Potential surrogate end-point for cardiovascular and other chronic inflammatory disease development |
|
| Quality of life scores | Months to years |
Establishes clinical benefit Incorporates PROs |
|
- Abbreviations: CCUS, clonal cytopenia(s) of undetermined significance; CHIP, clonal haematopoiesis of indeterminate potential; MACE, major adverse cardiovascular event; MDS, myelodysplastic neoplasm; MN, myeloid neoplasia; PRO, patient-reported outcomes; VAF, variant allele frequency.
There is a precedent of measuring MACE in the CH setting. In the CANTOS study of secondary prevention of cardiovascular events and death in patients who previously had a myocardial infarction and had elevated levels of C-reactive protein (CRP), the use of canakinumab was associated with a mild reduction of cardiovascular outcomes and death in all patients and greater than a 60% reduction in the subgroup of patients with TET2-mutated CHIP.61 Canakinumab therapy was associated with a lower incidence of non-myeloid malignancies; the reduction was greatest in individuals with TET2 mutations.62, 63 CHIP was associated with signatures of inflammation and infection defence, which were exacerbated by concomitant anaemia and ameliorated by canakinumab therapy.63 For patients with CCUS, improvement in cytopenias, changes in patient-reported outcomes and reduction in infections and transfusion needs are likely to be important.
Surrogate end-points in CHIP such as reduction in VAF, improvement in inflammatory markers (e.g. CRP, erythrocyte sedimentation rate, interleukin-6 [IL-6], IL-8) or other relevant biomarkers (e.g. those relevant to specific genotypes, such as increases in GDF15 in a TP53 mutant population or 2-hydroxyglutarate levels in those with IDH1/IDH2 mutations) may be easier to observe in a shorter time but are not yet clinically validated, so the clinical relevance of these end-points is unknown. The balance between a clinically meaningful outcome with a feasible measurable outcome will be a fundamental challenge in designing therapeutic trials in this setting.
Outcomes in long-term interventional studies may be difficult to attribute to a single intervention, especially if the duration of intervention is limited. In large studies of diabetes prevention in high-risk individuals, both lifestyle interventions and metformin were efficacious interventions for long-term diabetes prevention; however, neither group had a reduction in cardiovascular events after more than 20 years of follow-up.64 Therefore, changes in clinical practice based on surrogate end-points or interim analyses should be used with caution until clear evidence is available. Examples include altering decisions about allogeneic Hematopoietic stem cell transplant based on donor or recipient CH status or modifying standard chemotherapy or radiotherapy regimens for non-myeloid cancer patients due to incidentally detected CH.
Outcomes in non-interventional studies in CHIP
The majority of CH in the general population will be considered lower risk and may not be the prime focus of therapeutic interventional clinical trials. Low-risk CH may include those with a normal CBC, as well as a single mutation in DNMT3A or TET2 with low VAF, which are less likely to transform to an advanced MN. This group of people would be excellent candidates for clinical studies in previvorship, natural history studies, understanding risks or extrinsic factors that may predispose to clonal evolution and assessing quality of life and OS (Table 1). As these are important outcomes that cannot be captured in retrospective studies, a focus on innovative measures such as telehealth platforms and surveys may be utilized, as well as working with data managers to collect data uniformly.
Study design considerations
As a condition that is prevalent in the general population, with nuances in diverse and varied populations that remain understudied, efforts to design CHIP clinical trials that will lead to high enrolment and reduce barriers are very important. Efforts to include participants within various clinical practice settings beyond academic centres should be considered, including community practices, inner city and rural populations. Telehealth visits have been increasingly incorporated into clinical practice since the COVID-19 era, and novel clinical trial designs have included telehealth clinical trial design including which may increase access, including the IDH1 targeting CCUS study (NCT05030441). International collaborations as part of larger studies and cooperative groups may also increase enrolment.
THERAPEUTIC STRATEGIES IN CH
Targeting inflammation
Inflammatory pathways are an appealing target in CH, due to preclinical models and other evidence pointing to a reciprocal relationship between clonal expansion in CH and upregulation of a variety of inflammatory signalling cascades, including NLRP3 inflammasome and its downstream cytokines (e.g. interleukin-1β [IL1 β], interleukin 18). For example, the increase in atherosclerosis seen in the TET2 knockout murine models was mediated by IL1 β.8, 65 High doses of vitamin C modified TET2 function in murine models, leading to a prospective study of vitamin C in CCUS (NCT03418038), which showed no responses at 20 weeks (Table 3).66, 67 The CANTOS study described previously has motivated a prospective trial in CCUS with canakinumab (NCT05641831).61 NLRP3 inflammasome mediators are now being tested in the clinic for MDS and could be explored for CH/CCUS if safety patterns permit (NCT06097663). In addition, luspatercept treatment in the front-line COMMANDS MDS study showed downregulation of IL-1, IL-1R, IFNα, IL-6 pro-inflammatory pathways suggesting a modulation of inflammatory bone marrow microenvironment along with a reduction in NT-proBNP and may be attractive target in patients with CCUS.68 As the inflammatory mediators and clinical consequences of CH are genotype-specific, such as the link between DNMT3A-mutated CH and osteoporosis, studies should aim to collect data encompassing a variety of CH driver mutation and end-organ consequences.32
| Study identifier | Title | Intervention | Select outcome measures |
|---|---|---|---|
| NCT03418038 | Ascorbic acid and combination chemotherapy for the treatment of relapsed or refractory lymphoma or CCUS | Ascorbic acid (Vitamin C) |
Primary: ORR, haematologic response rate Secondary: OS, PFS, transfusion dependency, percent eligible for transplant |
| NCT05102370 | A Study of enasidenib in people with CCUS | Enasidenib | Primary: Best response (assessed up to 18 months) |
| NCT04741945 | Repurposing Metformin as a Leukaemia-preventive drug in CCUS and LR-MDS | Metformin |
Primary: Change in VAF Secondary: Safety, changes in weight and other bodily composition |
| NCT05030441 | Ivosidenib for patients with CCUS and Mutations in IDH1 | Ivosidenib |
Primary: Improvement of haematologic parameters Secondary: change in VAF, DFS |
| NCT05641831 | Canakinumab for the prevention of progression to cancer in patients with CCUS, IMPACT study | Canakinumab versus placebo |
Primary: Time to overt malignancy (assessed up to 6 years) Secondary: Haematologic ORR, changes in VAF, OS, cardiovascular events, infection events, PROs |
| NCT06063486 | Curcumin to improve inflammation and symptoms in patients with CCUS, low-risk myelodysplastic syndromes, and myeloproliferative neoplasms | Curcumin, placebo |
Primary: Inflammatory cytokine levels and symptoms Secondary: Changes in VAF, methylation patterns, peripheral blood counts, safety |
| NCT05483010 | Statins in patients with CCUS and myelodysplastic syndromes | Atorvastatin or rosuvastatin |
Primary: Change in VAF Secondary: EFS at 15 months |
| NCT06097663 | A study to investigate the efficacy, safety, and tolerability of DFV890 and MAS825 for inflammatory marker reduction in adult participants with coronary heart disease with CHIP | DFV890, MAS825 |
Primary: Serum levels of IL-6 and IL-18 Secondary: Plasma concentrations of DFV890, MAS825 |
- Abbreviations: CCUS, clonal cytopenia(s) of undetermined significance; CHIP, clonal haematopoiesis of indeterminate potential; DFS, disease-free survival; EFS, event free survival; MACE, major adverse cardiovascular event; MDS, myelodysplastic neoplasms (syndrome); MN, myeloid neoplasia; ORR, overall response rate; OS, overall survival; PFS, progression-free survival; PRO, patient-reported outcomes; VAF, variant allele frequency.
- a No studies are currently assessing interventions in CH without cytopenias.
Addressing select mutations
Another therapeutic strategy is earlier intervention with small-molecule inhibitors or other agents already approved for the treatment of MDS or AML, such as IDH1 and IDH2 inhibitors, low-dose/short course DNA methyltransferase inhibitors (hypomethylating agents), lenalidomide, luspatercept, imetelstat or haematopoietic growth factors in at-risk individuals. This approach does have appeal, as specific CH mutations such as IDH1 and IDH2 mutations, for example, are associated with an increased risk of disease progression, and the safety profile of IDH inhibitors is well established; however, IDH mutations are uncommon in CH. Since these treatments are associated with treatment-related toxicity (e.g. cytopenias with hypomethylating agents, differentiation syndrome with IDH inhibitors), justification of treatment needs to be supported by longer term safety data and/or a clear definition of risk. If targeted interventions show clear promise in long-term prevention of morbidity and mortality in particularly adverse populations, novel approaches such as autologous gene editing or other techniques to prevent disease can be considered in the future, based on success in diseases such as the haemoglobinopathies.69 The duration of therapy with targeted agents is also an important consideration particularly if disease occurrence can take many years, potentially exposing individuals to drug toxicities versus waiting for disease to occur and then treating with targeted agents. Delay of progression to MN becomes an important criterion in such cases.
Nutritional targets
The role of dietary interventions and naturally occurring compounds in reducing clonal expansion in CH is attractive given the low tolerance for toxicity and the strong precedent of effective non-pharmacologic intervention in a variety of similar precursor states. Diet has been shown to influence stem cell fitness in several preclinical studies, and observational cohort data indicate that individuals with less healthy eating habits have a greater prevalence of CHIP.70 An ongoing randomized placebo controlled study of a plant-based dietary intervention in patients with precursor myeloma states is ongoing, and a similar dietary intervention in the CH population, to assess changes in clonal trajectory, is attractive.70
Repurposing drugs
Novel therapies that may affect oxidative phosphorylation or metabolomics or epigenetics may shed new light in prevention of progression in a predisease state. Repurposing drugs approved drugs such as HMG Co-A reductase inhibitors, particularly when targeting associated cardiovascular and other chronic disease of ageing may also play a role and warrant further investigation. There is preclinical evidence to support studying mTOR inhibition by rapamycin in DNMT3A- and ASXL1-mutated CH.71, 72 Statins and metformin are already in clinical investigation in CCUS (Table 4).
| Therapeutic strategy | Examples |
|---|---|
| Address modifiable risk factors | Smoking cessation, nutrition |
| Naturally occurring active biological compounds | High dose vitamin C, curcumin |
| Repurposing cardio-metabolic agents | Metformin, statins |
| Anti-inflammatory/anti-cytokine agents | Canakinumab, NLRP3 inhibitors |
| Selective mutational targeting | IDH1 inhibitor, IDH2 inhibitor |
| Metronomic therapy of FDA-approved agents for MDS or AML | Luspatercept, imetelstat, hypomethylating agents |
- Abbreviations: AML, acute myeloid leukaemia; CCUS, clonal cytopenia(s) of undetermined significance; CHIP, clonal haematopoiesis of indeterminate potential; FDA, Federal Drug Administration; IDH, isocitrate dehydrogenase; MDS, myelodysplastic neoplasm; NLRP3, NLR family pyrin domain containing 3.
Targeting the fitness landscape
There may be a role for considering interventions specifically for populations that may be at higher risk for MN progression, such as people with pre-existing or therapy-related CH within DNA damage response genes (e.g. TP53 or PPM1D), who will undergo additional chemotherapy or radiation for a non-haematological indication. It is well established that select genotoxic and immunomodulatory drugs can promote the expansion of pre-existing TP53- and PPM1D-mutated haematopoietic clones; thus, it is crucial to exercise caution when considering the study of modulating treatment decisions for the primary malignancy.73-75 Thoughtful interventions that will likely not compromise the success of eradicating the existing disease (e.g. another cancer) will need to be considered in these novel trial designs.
LESSONS LEARNED FROM EARLY CLINICAL TRIAL DEVELOPMENT: A CALL FOR UNITY
Most CCUS studies are still in active enrolment, and several themes have been noted by investigators in the designing and implementation of these studies. Early involvement in regulatory discussions with the FDA as well as discussions with industry partners to gauge interest in implementing these studies may help in the design and quicker implementation of studies. Further refinement of risk stratification models is needed to define the highest at-risk populations that are most suited to benefit. Innovative trial designs that optimize enrolment are needed. Defining new CCUS-specific outcomes can be beneficial for future trials, as low-risk MDS outcomes may not be applicable in every study.76 Long-term follow-up along with thoughtful correlative studies may help define the populations that will most benefit.
Designing and treating CHIP and CCUS in interventional trials is a new approach that moves from ‘treatment’ to ‘secondary/tertiary prevention’ studies. Such studies are less common in cancer, which requires adaptations in trial design. While early prospective results validate retrospective population database studies, data from many more patients is needed.19, 26, 77 Collaborative meetings for investigators, researchers, drug developers/trial sponsors and regulators to discuss new approaches and observations in CH and CCUS will allow modification of studies as new data emerge. We envision an annual pre-disease congress as an opportunity to discuss clinical approaches to CH and CCUS by integrating key discoveries from and linking scientists and clinical investigators (https://genetic-hematologic-malignancies-us-2023.md-education.com/). Clinical practice algorithms and guidelines may help standardize approaches in this quickly changing clinical space.
CONCLUSION
The opportunity to therapeutically intervene to prevent progression to an overt malignancy and reduce cardiovascular and other non-haematologic outcomes is highly appealing. It will be important to design therapies to minimize risk and clearly define outcomes, and to carefully select the highest risk population for interventions. Collaborative meetings and multicentre interventional clinical trials and biorepositories are needed to facilitate this goal. International groups and consortia will need to work together to develop harmonized guidelines on CH trial design. Partnership with federal regulatory authorities will propel haematologic malignancies into a new era of pre-disease intervention. We acknowledge the limited experience in this evolving field to firmly recommend clinical guidelines. We anticipate that goalposts will change as our understanding of the natural history and clinical outcomes in people with CH improves.
AUTHOR CONTRIBUTIONS
All authors contributed to the review. TH, AS, DPS and MRS conceived the idea of the review and wrote the initial draft. All authors provided critical suggestions and refined the final draft of the review.
CONFLICT OF INTEREST STATEMENT
TH has served on advisory boards for Servier Pharmaceuticals, Morphosys and Bristol Myers Squibb. AS has received research funding from Kymera Therapeutics, advisory board fees from Gilead Sciences, Rigel Pharmaceuticals and Kymera Therapeutics, consultancy fees from Janssen Pharmaceuticals and honoraria from NACE & PeerView. PD has received research funding from Kura Oncology, Janssen Pharmaceuticals, BMS and has received consultancy fees for Servier Pharmaceuticals, BMS, Abbvie/Genentech. DH has received research funding from Break Through Cancer, funding for AML-CHIP TeamLab. UMB received grants/research support from Abbvie, Incyte, Jazz, Pfizer; served on an advisory board for Abbvie, Genentech, Agios, Novartis, Blueprint, Astellas, Takeda, Kura, Servier; and received honorarium from RUNX1 foundation. YFM has received honoraria/consulting fees from BMS, Kura Oncology, BluePrint Medicines, Geron, OncLive and MD Education, VJHemOnc and Medscape Live. YFM participated in advisory boards and received honoraria from Sierra Oncology, Stemline Therapeutics, Blueprint Medicines, Morphosys, Taiho Oncology, SOBI, Rigel Pharmaceuticals, Geron, Cogent Biosciences and Novartis. YFM received travel reimbursement from Blueprint Medicines, MD Education and Morphosys. None of these relationships were related to this work. YA served on scientific advisory boards or consults for: Astellas, Bristol Myers Squibb, Geron, KiTE, Pfizer, Rigel and Servier. YA received institutional trial support from AbbVie, ALX Oncology, Biomea, Biosight, Curis and Novartis. KLB received research funding and served on a medical advisory board of Servier. MSP served on advisory boards for CT1 and Astra Zeneca and received research funding from Stem Line, Kura Oncology, Polaris, Epigenetix, Solutherapeutics. AKV has received research funding from Prelude, BMS, GSK, Incyte, Medpacto, Curis and Eli Lilly and is a scientific advisor for Stelexis, Novartis, Acceleron and Celgene and received honoraria from Stelexis and Janssen and held equity in Stelexis and Throws Exception. SJ reported consultancies at Novartis, Roche Genentech, Astrazeneca; speaking fees from GSK and Merck; scientific advisory board membership and equity at Bitterroot Bio and at TenSixteen Bio, all unrelated to the present work. AGB is a scientific advisor and has received personal fees and equity in TenSixteen Bio. DPS is currently employed at Ajax Therapeutics. MRS has consulted and served on advisory boards for and/or received travel expenses from BMS, CTI, Forma, Geron, GSK, Rigel, Taiho and Treadwell; is an equity holder in and served on advisory committees for Empath Biosciences, Karyopharm and Ryvu; and received research funding from ALX Oncology, Astex, Incyte and Takeda. ZK, ZX, AK, AS, AS, JBH, DAS have no disclosures to report.




