Venetoclax induces profound and sustained responses in patients with relapsed/refractory light-chain amyloidosis
Systemic light-chain (AL) amyloidosis has a poor prognosis, especially when progressive heart failure occurs. AL treatment has improved and the combination of bortezomib, dexamethasone, and cyclophosphamide had become a widely used treatment regimen, conferring a high response rate and prolonged survival, which could be improved with daratumumab adjunction.1 However therapeutic options are limited in relapsed/refractory (R/R) patients, especially those who progressed after treatment with daratumumab.2
AL amyloidosis is characterized by a frequent t(11;14) translocation, detected in up to 50% of AL patient.3 In myeloma cells, this translocation is also associated with higher BCL2 and lower MCL-1/BAX expression, conferring in vitro sensitivity to BCL2 inhibition with venetoclax.4 These results were subsequently confirmed in a clinical trial on patients with R/R myeloma in which venetoclax showed promising activity, especially in patients harbouring the t(11;14) translocation.5
Given the high rate of t(11;14) in AL amyloidosis, venetoclax could be an attractive treatment option for R/R AL amyloidosis. However, only few cases and a cohort of 12 patients have recently6 been reported, including a limited number of patients with cardiac involvement.
We report here the results of a single-centre retrospective study on consecutive R/R AL amyloidosis patients treated off-label with venetoclax in a French academic referral centre between February 2017 and January 2020.
The diagnosis of AL amyloidosis and evaluation of organ involvement were established locally according to consensus criteria.7 Cardiac stage was determined using the European Modified Mayo Clinic Stage. The standard and updated criteria for cardiac and haematological response evaluation were used.8 Three patients had associated multiple myeloma (two patients had bone lesions, and one patient had anaemia, renal failure and 56% plasma cells in the bone marrow aspirate). Venetoclax was given daily, alone or in association with dexamethasone, with or without bortezomib. Treatment was administered until progression or toxicity. Patients received prophylaxis based on cotrimoxazole, valaciclovir, and penicillin V. Within the limitations of a retrospective study, tolerability and toxicity data were also collected. Toxicity grading followed Common Terminology Criteria for Adverse Events version 5.0. Data were recorded electronically according to the French CNIL (Commission National de l’ Informatique et des Libertés; authorization number # 1846564 v0, March, 25th 2015).
Ten patients with R/R AL amyloidosis were treated with venetoclax. Their clinical characteristics are shown in Table I. The median age was 71 years (40–84). The median number of organs affected was 2 (1–4). Nine (90%) patients had cardiac disease: two patients with stage I, two with stage IIIA, and six with stage IIIB. Six patients had renal involvement and three multiple myeloma. Translocation t(11;14) was detected in seven patients, absent in two, and undetermined in one. The median value for the difference between involved and uninvolved light chains (dFLC) was 90 mg/dl (21–998).
| Characteristics | Median (range)/n (%) |
|---|---|
| Age (years) | 71 (40-84) |
| Male | 5 (50%) |
| Time from diagnosis (months) | 34·5 (7–125) |
| Organ involvement | |
| Cardiac | 9 (90%) |
| Renal | 6 (60%) |
| Liver | 2 (20%) |
| Gastrointestinal | 1 (10%) |
| Peripheral nerve | 2 (20%) |
| Autonomic nerve | 1 (10%) |
| Pulmonary | 0 (0%) |
| Soft tissue | 1 (10%) |
| No. of organs involved | |
| 1 | 3 (30%) |
| 2 | 5 (50%) |
| ≥3 | 2 (20%) |
| Mayo stage | |
| I | 2 (20%) |
| II | 0 (0%) |
| IIIa | 2 (20%) |
| IIIb | 6 (60%) |
| Left ventricular ejection fraction (%) | 54 (30–65%) |
| Serum creatinine (µmol/l) | 124 (48–242) |
| GFR (based on MDRD ml/min/1·73 m2) | 42 (23–125) |
| GFR < 50 ml/min/1·73 m2 | 7 (70%) |
| APL (UI/l, N < 150) | 109 (54–248) |
| Serum albumine (g/l) | 32·5 (10–38) |
| ECOG-PS | 2 (1-2) |
| Involved light chains lambda | 6 (60%) |
| dFLC (mg/l) | 90 (21–998) |
| dFLC > 180 mg/l | 3 (30%) |
| Multiple myeloma associated | 3 (30%) |
| Cytogenetic | |
| Failure | 1 (10%) |
| Presence of t(11;14) | 7 (70%) |
| Number of prior treatment | |
| 1 | 0 (0%) |
| 2 | 3 (30%) |
| ≥3 | 7 (70%) |
| Previous treatment lines | |
| Bortezomib | 10 (100%) |
|
Whose CyBorD |
6 (60%) |
|
IMiDs |
7 (70%) |
| Daratumumab | 10 (100%) |
| Best haematologic response of Daratumumab | |
|
CR |
0 (0%) |
|
VGPR |
1 (10%) |
|
PR |
5 (50%) |
|
SD |
3 (30%) |
|
PD |
1 (10%) |
| Reasons for initiating venetoclax therapy | |
| Refractory disease | 4 (40%) |
| Relapse | 4 (40%) |
| Non-optimal haematologic response | 2 (20%) |
| Treatment-related toxicity | 0 (0%) |
| Scheme of treatment | |
| VEN-Bor-Dex | 7 (70%) |
| VEN-Dex | 2 (20%) |
| only VEN | 1 (10%) |
| Daily dose of VEN | |
| 100 mg | 1 (10%) |
| 200 mg | 4 (40%) |
| 400 mg | 5 (50%) |
| No. of cycles of VEN | 6·5 (1–21) |
- GFR, glomerular filtration rate; MDRD, modification of diet in renal disease; APL, Alcaline Phosphatase; ECOG-PS, Eastern Cooperative Oncology Group-Performance Status; dFLC, difference between involved and uninvolved serum free light chains; CyBorD, cyclophosphamide–bortezomib–dexamethasone; IMiDs, immunomodulatory drugs; CR, complete response; VGPR, very good partial response; PR, partial response; SD, stable disease; PD, progressive disease; VEN, venetoclax; Bor, bortezomib; Dex, dexamethasone.
The median number of previous lines was 3 (2–4) and all patients had been treated previously with bortezomib and daratumumab. The best haematological response with daratumumab was as follows: a very good partial response (VGPR) for one patient, a partial response (PR) for five, stable disease (SD) for three and progressive disease (PD) for one patient.
The reasons for initiating venetoclax therapy were refractory disease for four patients (40%), relapse for four (40%), and non-optimal haematological response for two (20%).
Seven patients received a combination of venetoclax, bortezomib, and dexamethasone, as previously reported for multiple myeloma treatment.9 Two patients received a combination of venetoclax and dexamethasone, and one received venetoclax as a single agent. Patients received a median of 6 (1–21) cycles. Five patients received 400 mg per day, four 200 mg per day, and one 100 mg per day. The median duration of treatment was 189 days (31–1028). At the time of the analysis, four patients were still on treatment and six had stopped (three because of PD and three because of side effects).
The overall haematological response rate was 66·6% for the nine patients assessable for haematological response. Three patients achieved a complete response (CR), two a VGPR, and one a PR. Two patient had SD and one PD (Fig 1 and Table SI). Among the seven patients harbouring the t(11;14) translocation, four showed at least a VGPR, while only one of the three patients without t(11;14) experienced a response (VGPR).
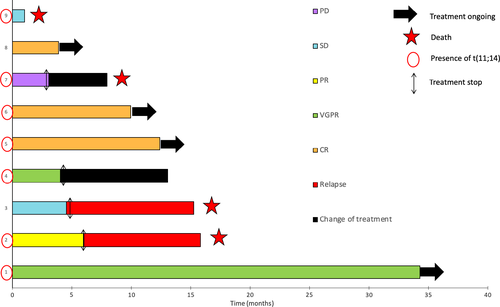
The median time to reach the best haematological response was 43 days (21–78). Four of the six patients with a haematological response were still on treatment and the median duration of the response was 241 days. The median follow-up was 270·5 days (31–1 028) and 50% of patients were still alive at the time of this report. The median overall survival was 10·5 months (Fig S1).
Among the nine patients with cardiac involvement, seven were evaluable for cardiac response. Four patients (57·2%) had a cardiac response, one (14·2%) had SD, and two (28·6%) showed progression of the cardiac dysfunction. Among the six patients with renal involvement, five were evaluable for renal response. One (20%) had a renal response, three (60%) had SD, and one (20%) showed renal progression (Table SI).
In terms of safety, grade 1–2 diarrhoea was the most common adverse event (n = 4). Four patients (40%) experienced infectious events, including pneumonia (n = 2), influenza (n = 1), and a urinary tract infection (n = 1). One patient (10%) showed haematological toxicity, with anaemia and grade 3 thrombocytopenia. Three patients discontinued venetoclax due to side effects (grade 3 asthenia, influenza infection, and acute respiratory distress; Table SII). None of the patients experienced tumour lysis syndrome. Adverse events were in line with what we observed with daratumumab in this population,10 reflecting more the fragility of these patients than the treatment toxicity.
Five patients (50%) died: three from cardiac complications of amyloidosis, one from infectious complications, and one from an undetermined cause.
In conclusion, we report a series of heavily pre-treated R/R cardiac AL amyloidosis patients, most of them with a severe cardiac involvement, treated with venetoclax. This treatment administrated as a single agent or in association with bortezomib and/or dexamethasone resulted in a sustained haematological and cardiac response with acceptable toxicities. These results support the prospective evaluation of venetoclax in AL amyloidosis.
Conflict of interest
FL reports personal fees from Miltenyi and travel grants from Celgene and Jansen. CH reports personal fees from Celgene during the conduct of the study and personal fees from Roche, Amgen, Janssen, Gilead, Novartis, and Takeda outside the submitted work. SO has received honoraria from Pfizer.
Author contributions
HP, KB, JD, SO, AG, AL, AM, LR, RG, CG, TD, FLB and FL treated patients and collected data. EP perfomed the pathological review. ABF and VMF performed laboratory tests. HP and FL wrote the manuscript. All the authors read and approved the manuscript.




