Outcome of a patient with refractory Hodgkin lymphoma on pembrolizumab, infected with SARS-CoV-2
A 22-year-old female presented at the Emergency Department on the 14 March 2020 with a three-day history of cough, pyrexia, sore throat, chills and rigors. Dyspnoea, myalgia and anosmia did not feature at presentation.
The patient had a history of early-stage unfavourable-risk, classical Hodgkin lymphoma (HL) for which she was diagnosed in May 2017. She underwent two cycles of adriamycin/bleomycin/vinblastine/dacarbazine (ABVD) with escalation to bleomycin/etoposide/adriamycin/cyclophosphamide/vincristine/procarbazine/prednisolone (escBEACOPP) for four cycles due to a suboptimal response on interval positron emission tomography (PET) scan. An end of treatment PET scan showed residual mass in the mediastinum which was negative for lymphoma when biopsied. An interval PET in February 2018 demonstrated progressive disease and salvage therapy was commenced with three cycles of ifosfamide/carboplatin/etoposide (ICE). A repeat PET scan demonstrated chemo-refractory disease and she subsequently received three cycles of brentuximab vedotin with a suboptimal response. She received 30 Gray of involved field radiotherapy in January 2019 with complete metabolic response. Unfortunately, the patient developed histologically confirmed disease recurrence in June 2019.
The patient was commenced on six-weekly pembrolizumab 400 mg in July 2019. PET post third cycle showed a mixed response to treatment. The patient was due for cycle 7 of therapy 11 days into inpatient stay on 23 March 2020.
The patient had no recent travel or sick contacts. The patient worked in a local beauty salon doing nail art and lived in her family home with her mother and two brothers who were all well.
On presentation vitals showed low-grade pyrexia; temperature 37.9°C, heart rate 65, respiratory rate 18, blood pressure 120/84, SpO2 96% on room air. Examination was unremarkable.
The patient was lymphopenic 0·27 (×109/l), had raised C-reactive protein (CRP) 42 mg/l, and raised lactate dehydrogenase (LDH) 282 U/l (previously within normal range in January 2020). Liver blood test and renal function, haemoglobin, neutrophil count and d-dimer parameters were within normal range. Platelets dropped transiently while an inpatient. A portable X-ray chest scan was initially clear.
Broad spectrum antibiotics, piperacillin–tazobactam and doxycycline, were starte4d on day 1 of admission to treat community-acquired pneumonia pending a SARS-CoV-2 swab result. Once COVID-19 was confirmed, lopinavir and ritonavir (LPV/r) were commenced on day 2.
Within the first six days of stay the patient was pyrexial and had rising O2 requirements. Shortness of breath coincided with bi-basal crackles on auscultation of lung fields and evolving infiltrates in the lower zones bilaterally on chest X-rays (Fig 1). Supplementary oxygen requirements increased from 0% on day 1 to a fraction of inspired oxygen (FiO2) of 40% on day 6. The intensive care service was consulted but intubation was not required at this time. Therapy was not altered throughout this period until day 7 (Day 6 of LPV/r) with the development of new diarrhoea. Antibiotics and LPV/r were stopped. At that time the patient was switched to hydroxychloroquine (HCQ) and azithromycin. The patient remained febrile until day 13 of symptoms (day 10 of admission and day 2 of HCQ/azithromycin). Corticosteroids were decided against. A drop in CRP levels, improvement in oxygenation, and resolution of symptoms appeared to coincide with commencement of HCQ and azithromycin (Fig 2).

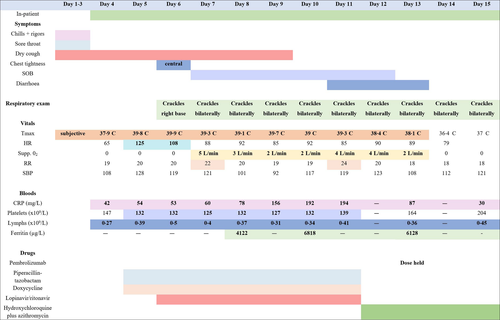
The patient was well, apyrexial and had no supplemental O2 requirements at time of discharge on day 16 of symptoms (day 13 of admission).
Discussion
Reports of outcomes for patients living with malignancy who are infected with SARS-CoV-2 are limited but appear to be worse than for the standard population. In a prospective cohort study of 1 590 Chinese patients diagnosed with COVID-19, 1% were found to have a history of cancer.1 These patients, especially the majority who had lung cancer, had a higher risk of severe events, a composite end-point of admission to intensive care unit, intubation and death, compared to the reminder of the cohort (39% vs. 8%, P = 0·0003).
Furthermore a report from a single centre in Wuhan indicated that people living with cancer were more likely to acquire COVID-19 infection than the general population [heart rate (HR) 2·31, 95% confidence interval (CI) 1·89–3·02] potentially due to the frequency of interactions with a healthcare setting.2
Our patient developed symptoms consistent with pneumonitis, a known complication in up to 2·5% of those receiving PD-1 inhibitors.3 At the time of presentation levels of community transmission of COVID-19 were low in the Republic of Ireland with 90 cases and an incidence of 1·9 per 100,000 population. Despite this a decision was made to test for SARS-CoV-2 as the primary differential.
Pembrolizumab is an immune checkpoint inhibitor targeting programmed cell death 1 (PD-1) ligand, used in melanoma, non-small cell lung cancer, urothelial cancer, and refractory HL. Predisposition to serious infection is not a feature of the monoclonal antibody, in fact the adverse appears to be true even relative to other immune checkpoint inhibitors.4 Patients receiving pembrolizumab have been shown to have increased levels of seroconversion with influenza vaccination compared to standard population.5 It is unknown to what extent pembrolizumab can potentiate immunological response in those with COVID-19. Bersanelli et al. hypothesise the potential dangers of administering PD-1 inhibitors in this context, the potential for dual pathology for lung injury, cytokine release syndrome caused by PD-1 inhibitors, overactivation of T cells, and mononuclear predominance in acute respiratory distress syndrome-associated COVID-19 may lead to a synergistic pro-inflammatory state.6
We report a positive outcome in a patient with refractory HL albeit with prolonged fevers and symptomatology and raised inflammatory markers in the context of HL and approaching her seventh cycle of pembrolizumab. Our patient was pyrexial for 13 days, longer than the median of 10 (95% CI 8–12 days) reported elsewhere.7 Factors in this patient's disease course may be underlying malignancy, significant exposure to cytotoxic chemotherapy, waning levels of pembrolizumab with dissipation of immune activation, a change of viral-directed therapy from LPV/r to HCQ and azithromycin or the natural progression of a new infectious disease. We highlight that this report is limited, being a single case. The patient had a number of factors associated with favourable outcome in COVID-19, younger age, female sex, and no other significant comorbidities like diabetes mellitus, obesity, or cardiovascular disease.
We would also like to highlight potential dilemma of an acute respiratory presentation in the current climate in patients taking PD-1 inhibitors. Pembrolizumab-induced pneumonitis, although a rare complication, carries a high mortality. While prompt administration of corticosteroids is necessary in the case of pembrolizumab-induced pneumonitis, this strategy may result in worse outcomes in patients affected by COVID-19.8 A careful risk versus benefit assessment using a multidisciplinary approach is advised in these cases.
Funding information
The authors received no funding for the preparation of this manuscript.
Conflicts of interest
The authors declare to have no conflicts of interest to declare regarding the present work.
Consent
Patient consent was obtained for submission.
Author contributions
All authors contributed to the writing of this article.




