Inflammatory mediators in sickle cell anaemia highlight the difference between steady state and crisis in paediatric patients
Sickle cell anaemia (SCA) is a chronic inflammatory disease with a complex mechanism of pathogenesis. The rheological phenomenon of SCA has been directly associated with the activation of sickle red blood cells, reticulocytes, leucocytes, platelets and endothelial cells, with the expression of several molecules secondarily expressed in this inflammatory environment and on the surface of these cells (Ware et al, 2017).
Although inflammatory mediators have been studied among SCA patients, the immunological and inflammatory mechanisms associated with the disease pathogenesis, endothelial activation and dysfunction, and repair mechanisms, as well as their roles as biomarkers of the crisis and steady states, remain unclear.
Considering the complex network of mechanisms involved in SCA pathogenesis, we investigated systemic levels of cytokines, including tumour necrosis factor-alpha (TNF-α); interleukin (IL) 1β, IL6, IL8, IL10, and IL12; and transforming growth factor beta (TGF-β). We also investigated inflammatory mediators, such as prostaglandin E2 (PGE2), leukotriene B4 (LTB4) and the vascular remodelling modulators matrix metalloproteinase-9 (MMP9) and its inhibitor, tissue inhibitor of metalloproteinase 1 (TIMP1), and free haem levels. To test the hypothesis that systemic levels of these molecules can be associated with steady and crisis states in SCA patients, we investigated the haematological and biochemical markers of oxidative stress, haemolysis and inflammation to identify biomarkers of prognosis, establishing risk factors for each phase of the disease.
We evaluated haematological, biochemical and immunological parameters in 101 stable SCA patients, 23 SCA patients in vaso-occlusive crisis (crisis state) and 146 healthy control individuals.
The human subject research board of the Instituto Gonçalo Moniz- Fundação Oswaldo Cruz (IGM-FIOCRUZ) and the Hospital da Criança das Obras Sociais Irmã Dulce (HCOSID) approved this study, with protocol number 0016.0.225.000-09. Each child's guardian signed the consent form, and the study followed the Brazilian standards for the development of research on humans. The present work is in accordance with the Helsinki Declaration of 1975 and its revision. More information is available in Data S1.
All analyses were performed using the EPI Info™ 6.04 (CDC, Atlanta, Georgia, USA) and Graphpad Prism 5.01 (GraphPad Software Inc., San Diego, CA, USA) software, considering P values <0·05 significant. Baseline values of selected variables are expressed as means. The Kolmogorov–Smirnov test was used to determine quantitative variable distribution. The Mann–Whitney test and independent t-test were used to compare two numerical variables according to distribution. Additionally, the receiver operator characteristics (ROC) curve and C-statistics analyses were performed to estimate the predicted disease severity for acute and chronic events using data from each candidate SCA biomarker.
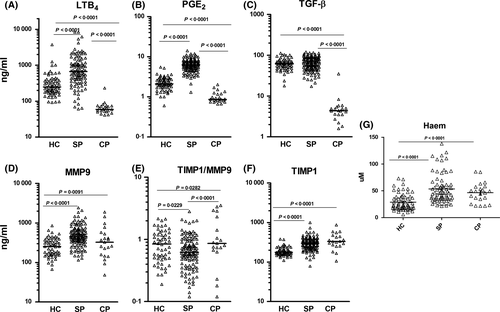
Characteristics of the SCA patient groups and the healthy control group are described in Tables S1 and S2. As expected, the crisis state SCA patients had the lowest haematological and chemical marker concentrations. Our results show that LTB4, PGE2 and TGF-β were increased in steady state SCA patients. In addition, higher concentrations of haem, TIMP1, and MMP9 were increased in both patient groups (steady and crisis state) (Fig 1A–G).
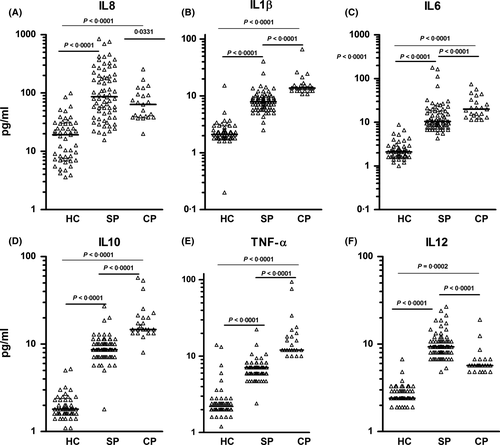
The inflammatory cytokines IL1β, IL6, IL10 and TNF-α were increased in SCA patients in crisis state, and IL12 and IL8 were increased in both crisis and steady state SCA patients (Fig 2A–G).
The ROC curve showed a predictive power and demonstrates that LTB4, TGF-β and PGE2 serve as markers of steady state SCA, whereas TNF-α, IL1β and IL10 serve as markers of crisis state SCA (Figure S1).
Inflammation is a complex mechanism modulated by several cell types as well as many different molecules. In this context, the inflammatory response in SCA is driven by a considerable amount of stimuli, such as monocytes, neutrophils, platelets, irreversibly sickled erythrocytes, cytokines, lipid mediators and even haem released during haemolysis (Taylor et al, 2008; Lanaro et al, 2009; Monteiro et al, 2011; Zhang et al, 2016). We found increased levels of LTB4, PGE2 and TGF-β among steady state patients. These molecules have been previously associated with neutrophil chemotaxis and vascular endothelial cells activation, and were also correlated with leucocyte counts (Setty & Stuart, 2002; Monteiro et al, 2011; Torres et al, 2016). Cytokines are molecules responsible for the signalling mechanisms during immune response and we identified higher IL1β, IL6, IL10 and TNF-α levels in crisis state SCA. These cytokines are produced during acute inflammatory conditions, such as the crisis state, and were associated with vascular dysfunction and leucocytosis. It is believed that neutrophils, followed by monocytes and endothelial cells, may serve as a source of these mediators (Brittain & Parise, 2007; Lanaro et al, 2009). The levels of free haem, IL12, IL8, TIMP1 and MMP9 remained elevated on both states. SCA patients exhibit a chronic haemolytic feature and systemic free haem levels and reactive oxygen species are released during haemoglobin (Hb) catabolism following intravascular haemolysis (Taylor et al, 2008). Both IL8 and free haem were associated with acute chest syndrome in SCA (Adisa et al, 2013).
Systemic levels of MMPs and TIMPs, as well as their ratio, have been associated with normal and pathological events, including tissue remodelling, metastasis, angiogenesis, multiple sclerosis, obesity, metabolic syndrome and atherosclerosis (Belo et al, 2009). Our data suggest continuous production in both SCA groups, which may represent active matrix remodelling and maintenance of tissue destruction and degradation in these patients.
The ROC curve analysis allowed us to identify markers associated with steady state and crisis state SCA patients. The markers had high sensitivity, specificity and accuracy, showing high predictive values for these biomarkers in the follow-up of SCA patients.
Our data highlight the molecular differences in the chronic inflammatory response exhibited by both states of the disease. LTB4, PGE2 and TGF-β may be useful predictors of steady state SCA while IL1β, IL6 and TNF-α may be useful predictors of crisis state SCA. The high levels of free haem, MMP9 and TIMP1 in both SCA states suggest a possible role of free haem in the chronic haemolysis and vasculopathy.
Acknowledgements
We thank the physician and laboratory technicians who provided technical support and assistance with the sickle cell patients and with routine laboratory tests.
Authorship
MOSC was involved in the study design, collected the samples, performed the experiments at IGM/FIOCRUZ and at College of Pharmaceutical Sciences (UFBA), performed statistical analyses and wrote the paper. TAS, BAVC, NFL, JHOR and CGB helped with the sample collection and performed the enzyme immunoassays. CCG, CVBF, LMF, RPS provided technical support, discussed the results and co-wrote the paper. LCR, IML and VML assist the patients enrolled in the study. MBN, VMB and MSG were involved in the design and coordination of the study, provided academic support, co-wrote and critically revised the manuscript. All authors read and approved the final manuscript.




