Akt inhibitor MK2206 selectively targets CLL B-cell receptor induced cytokines, mobilizes lymphocytes and synergizes with bendamustine to induce CLL apoptosis
Accumulating evidence supports the critical role of B-cell receptor (BCR) activation in chronic lymphocytic leukaemia (CLL) pathogenesis (Herishanu et al, 2011). Recent preclinical and clinical studies indicate BCR signal inhibitors, specifically the Bruton tyrosine kinase (BTK) inhibitor Ibrutinib and phosphatidylinositide 3-kinase (PI3K) δ inhibitor CAL101, have impressive preclinical and clinical efficacy in CLL (Herman et al, 2010; Byrd et al, 2013). Akt is downstream of the signalling cascade following BCR ligation. Preclinical studies performed using co-culture of CLL B-cells with marrow stromal cells highlight the importance of PI3K/Akt signalling in the activation of both cell types during their interactions that support survival of CLL B-cells (Edelmann et al, 2008; Ding et al, 2010). MK2206 is a highly selective oral allosteric Akt inhibitor found to have minimal side effects in a phase 1 trial of patients with refractory solid tumours (Yap et al, 2011). The present study determined the maximum tolerated dose (MTD) of MK2206 as a single-agent and its ability to target Akt in tumour cells. Here we explore the in vitro efficacy of MK2206 on CLL B-cell survival, its potential synergy with bendamustine, and its impact on BCR ligation events including cytokine release both in vitro and in vivo. Materials and methods are detailed in Appendix S1.
We initially tested the effect of the Akt inhibitor, MK2206, on CLL B-cell survival. Dose and time-dependent apoptosis was induced by Akt inhibition with MK2206 (Fig 1A, n = 37, Appendix S1). Unlike CLL cells, normal peripheral blood mononuclear cells did not undergo apoptosis after exposure to MK2206. Basal phosphorylation of AktS473 was detected at variable levels amongst tested CLL samples (n = 7) but was completely abolished by MK2206 treatment at the 1 μmol/l dose (Fig 1B). MK2206 also resulted in cleavage of the poly (ADP-ribose) polymerase (PARP) protein and significantly decreased the activation of Akt target p70S6K. However, expression of the p85 subunit of PI3K, which is upstream of Akt, was not affected. Next we tested whether established prognostic factors would be associated with differential CLL apoptosis levels induced by MK2206. No significant differences in MK2206-induced cell death were found based on the presence or absence of IGHV mutation, del (17p13), positivity of ZAP70 and CD38 (Fig 1C–F). These results indicated that MK2206 is able to induce apoptosis in CLL B-cells independent of adverse prognostic factors.
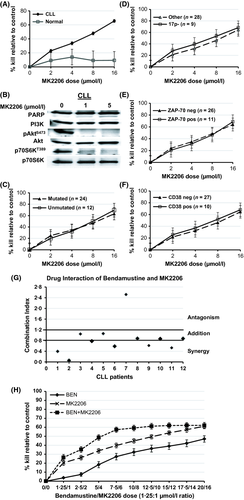
To assess whether MK2206 could enhance the drug sensitivity of CLL cells to the established agent (bendamustine) in relapsed disease (Fischer et al, 2011), we next explored the impact of MK2206 in combination with bendamustine on CLL apoptosis. An additive or synergistic affect was observed when MK2206 was added to bendamustine in 11 of the 12 CLL samples tested (Fig 1G and 1H).
Given the prognostic significance of BCR-induced cytokines (Sivina et al, 2011), we subsequently tested if Akt inhibition with MK2206 could abrogate BCR-mediated cytokine secretion and signal activation. BCR ligation with anti-IgM significantly increased production of selective immune cytokines (CCL3, CCL4, CCL2, IL-2Rα, IL-1Rα and IL-8) among the 30 cytokines tested (Fig 2A-B, n = 7). CCL3 and CCL4 upregulation are consistent with the previous report (Burger et al, 2009). The increase of CCL2, IL-2Rα, IL-1Rα and IL-8 following BCR ligation of CLL has not been previously reported. Pre-treatment with MK2206 abrogated the increase of CCL3, CCL4, CCL2 and IL-2Rα (Fig 2A), but not IL-1Rα and IL-8 (Fig 2B). Variable degrees of pAktS473, pGSK3βS9, p44/42ErkT202/Y204 and p70S6KT389 activation were also observed at 30 min after BCR stimulation (Fig 2C). MK2206 pretreatment reduced or abolished the activation of pAktS473, pGSK3βS9 and p70S6KT389 induced by anti-IgM and reduced the activation of p44/42ErkT202/Y204 to a variable degree. Collectively, these in vitro results indicate that MK2206 selectively abolishes BCR induced CCL3, CCL4, CCL2 and IL-2Rα production, probably via abrogating Akt and Erk signals. Other BCR-induced cytokines, such as IL-8 and IL-1Rα however were not affected by MK2206, suggesting these cytokines are induced by BCR-initiated signals other than those mediated by Akt or Erk phosphorylation.
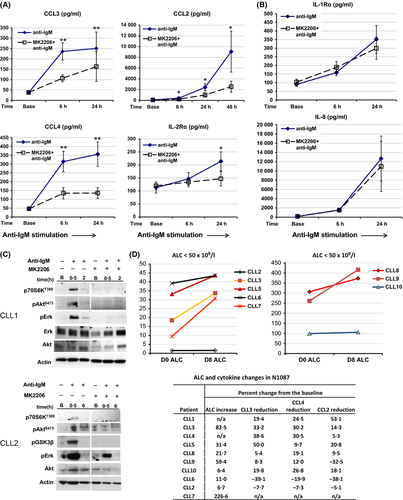
These preclinical studies support trials of MK2206 in combination with bendamustine for CLL patients. To that end, we initiated a phase 1/2 trial of MK2206 in combination with bendamustine and rituximab for patients with relapsed CLL (N1087) in 2011. N1087 is currently open for accrual with 10 patients enrolled to date. To evaluate the single agent effect of MK2206, this trial involves a 1-week run-in of MK2206 monotherapy prior to initiating bendamustine and rituximab (Appendix S1). Similar to the finding of lymphocyte mobilization from other BCR targeting therapies, all patients evaluated (n = 8) had increases of their absolute lymphocyte count (ALC) after a single dose of MK2206 monotherapy (Fig 2D, mean increase of eight patients: 56%). The increase in ALC after the first dose of MK2206 was modest in three of these patients (6·3%, 6·7% and 11·0% increase respectively), and more dramatic in the remaining five patients (mean increase of 84·3%; Fig 2D).
To explore the clinical relevance of our in vitro results showing that MK2206 abrogates BCR-mediated CCL2/3/4 secretion, we investigated the effect of a single-dose MK2206 on the plasma levels of these cytokines in trial patients after 1 week. The majority of the tested nine patients had a decrease in CCL3 [mean ± standard error of the mean (n = 7): 25% ± 6% reduction], CCL4 [(n = 7), 22% ± 3% reduction] and CCL2 level [(n = 6), 20% ± 7% reduction] after a single-dose MK2206 (Fig 2D). In contrast, two patients were found to have small increases of these three cytokines after the single-dose of MK2206. Notably these two patients also experienced the smallest increase in ALC. Although our sample size is too small to draw a definitive conclusion, these findings corroborate our in vitro results and suggest that the reduction of the BCR-stimulated CCL2/3/4 secretion is associated with lymphocyte mobilization.
Collectively, our in vitro and in vivo findings indicate that MK2206 induces apoptosis of CLL B-cells and is able to block the signal activation and cytokine up-regulation induced by BCR ligation. Single agent MK2206 is capable of mobilizing leukaemic B-cells and decreases CCL3, CCL4 and CCL2 production in vivo. We believe that this data strongly encourages further clinical testing of MK2206 either alone or in combination with traditional chemotherapeutic drugs in CLL.
Acknowledgements
This work was supported by funding from NCI grant K23CA160345 (WD), NCI grant CA95241 (NEK) and Cephalon (TDS). Dr. Shanafelt is a Clinical Scholar of the Leukemia and Lymphoma Society.
Authorship contributions
WD designed research and performed the experiments, analysed and interpreted the results, and wrote the paper. TDS and NEK designed research, interpreted the results, and wrote the paper. CEL, CS and TRS performed the experiments and interpreted the results. CE designed research, provided scientific input, review, and discussion. SK provided reagent and provided review and input. JFL, TGC, DAB, MC recruited patients, provided input and discussion.
Disclosure of conflicts of interest
TDS has received research support from Celgene, Hospira, Cephalon, Genentech, Glaxo-Smith-Kline and Polyphenon E International. SK has consulting relations with Merck, Celgene, Millennium, Novartis, Sanofi and Onyx (all uncompensated). CE was on the advisory board of Merck over 1 year ago. NEK has received research support from Celgene.




