In vitro effect of hyoscine-N-butyl bromide and diclofenac sodium in human tuba uterina
Funding information: The authors declared that this study has received no financial support.
Abstract
Introduction
To investigate the in vitro effect of diclofenac on tubal smooth muscle as an alternative to hyoscine-N-butyl bromide, which is used for premedication before hysterosalpingography (HSG).
Material and Methods
Fallopian tubes were retrieved from seven healthy women after bilateral tubal ligation and in vitro contractility and histological studies were conducted using tissue bath and immunohistochemistry.
Results
Diclofenac sodium and hyoscine-N-butyl bromide did not significantly change the basal mean tension; however, they decreased the contractions induced by potassium chloride (KCl). The relaxant effect of diclofenac sodium and hyoscine-N-butyl bromide was not statistically significantly different. The presence of cyclooxygenase (COX)-2 enzyme in the fallopian tube was demonstrated by immunohistochemical studies.
Conclusions
The in vitro relaxant effect of diclofenac sodium on the fallopian tube is similar to hyoscine-N-butyl bromide. Diclofenac may have the potential to be used as an alternative to hyoscine-N-butyl bromide in premedication in HSG.
1 INTRODUCTION
Female infertility is one of the common gynaecological problems. About 30% of women infertility is due to fallopian tube (tuba uterina) abnormalities.1 Hysterosalpingography (HSG), saline infusion sonograph and laparoscopy with chromopertubation are the methods used in the evaluation of tubal patency.2, 3 HSG is the standard technique for evaluating tubal patency, as it is simple, inexpensive and non-operative.4 Proximal tubal occlusion exhibits about 39% high false positive rate at HSG, most likely due to spasms.5 Hyoscine-N-butyl bromide, an anticholinergic agent, is commonly used as an antispasmodic in genitourinary spasms. The administration of hyoscine-N-butyl bromide prior to HSG can lower the false positive rates of tubal occlusion.6 Also, premedication with hyoscine-N-butyl bromide decreases the pain scores due to its spasmolytic effect. For these reasons, it is commonly prescribed before the HSG procedure.7
Prostaglandins are one of the intrinsic systems that control tubal function.8 Cyclooxygenase (COX)-1, COX-2 and prostaglandin synthase are expressed by human oviductal cells.9 Prostaglandin (PG)I2 and PGE2 are major products of PG biosynthesis in the human fallopian tube.10 Additionally, the receptors for PGE1, PGE2, PGI2 and PGF2α are present in the human fallopian tube.10, 11 Diclofenac inhibits PG synthesis by inhibiting COX-1 and COX-2 enzymes and shows analgesic, anti-inflammatory and antipyretic properties. The relaxant effect of diclofenac on isolated human ureteral smooth muscle,12 mouse airway smooth muscle13 and rat uterine smooth muscle14 has been demonstrated in previous studies. However, the in vitro effect of diclofenac on the smooth muscle of human tuba uterina is unknown.
Diclofenac may reduce tubal contractions by inhibiting PG synthesis and may decrease the rate of false positive tubal occlusion before the HSG procedure. Moreover, it may also contribute to reducing the pain associated with tubal occlusion due to its analgesic effect. In this study, we aimed to investigate the in vitro (histological and pharmacological methods) effect of diclofenac on tubal smooth muscle as an alternative to hyoscine-N-butyl bromide, which is used for premedication before HSG in the diagnosis of proximal tubal occlusions.
2 MATERIAL AND METHODS
2.1 Study subjects
Our study was carried out in accordance with the principles of the Declaration of Helsinki, with the approval of the Izmir Katip Celebi University Faculty of Medicine, the local ethical organization. The study was conducted in accordance with the Basic & Clinical Pharmacology & Toxicology policy for experimental and clinical studies.15 Seven healthy women with a mean age of 36 years (28–40 years) who underwent bilateral tubal ligation for sterilization were included in the study. All tissues were collected during the late follicular phase of the menstrual cycle. Patients with pelvic inflammatory disease (PID), tuboovarian abscess and primary and secondary infertility were not included in the study. None of the women participating in the study had a history of IUD use, except for one (she had been using a copper IUD for 5 years). Except for one of the women, none of them was a smoker. None of the women used drugs. During surgery, the fallopian tubes were excised. Biopsies were obtained from the ampullary part of the fallopian tubes. The biopsies were divided, and one piece was fixed for immunohistochemistry. The other piece was used for functional studies in an in vitro tissue bath. Immunohistochemistry was also performed on the same tissues after functional studies.
The fallopian tubes used for the in vitro contractility experiments were immediately placed in Krebs–Henseleit solution (composition in mmol/L: potassium chloride 4.7, sodium chloride 118, magnesium sulphate heptahydrate 1.2, calcium chloride dihydrate 1.2, sodium dihydrogen phosphate 1.2, sodium bicarbonate 25 and glucose monohydrate 11), and functional studies were conducted within 2–3 h after surgery.
2.2 Experimental protocols of functional studies
Longitudinal tissue strips (7 × 1 × 1 mm) were prepared and placed into a 10 ml tissue bath chamber filled with pre-aerated (95% O2 and 5% CO2) Krebs–Henseleit solution at 37°C and rested for 15 min before the initial tension set. In the functional studies of the fallopian tube, 1 g tension was uploaded to the tied strips by an isometric force-displacement transducer (FDT-05, MAY, Turkey). For functional studies, there were two separate groups in which we investigated the effects of diclofenac sodium and hyoscine-N-butyl bromide: the diclofenac group and the hyoscine group. Fallopian tubes were allowed to equilibrate for 30 min and washed every 15 min. After equilibrium, for the evaluation of the effects of drugs on basal mean tension, diclofenac sodium (10−6–3 × 10−4 M) and hyoscine-N-butyl bromide (10−6–3 × 10−4 M) were added separately to the tissue bath in a cumulative manner. After a 30 min washout and resting period, for the evaluation of the relaxation effect, diclofenac sodium (10−6–3 × 10−4 M) and hyoscine-N-butyl bromide (10−6 3 × 10−4 M) were added separately to the tissue bath in a cumulative manner after pre-contracted with 80 mM KCl. Isometric tensions were recorded with an amplifier system (MP36 Biopac Systems Inc., Santa Barbara, CA, USA) to a computer using the Biopac computer program.
In each experimental protocol, diclofenac sodium and hyoscine-N-butyl bromide were applied in two different baths. First, the effects of hyoscine-N-butyl bromide and diclofenac sodium on basal mean tension were investigated separately. After the washout period, the effects of diclofenac sodium and hyoscine-N-butyl bromide on the contracted tissue after pre-contraction with KCl were investigated.
Hyoscine-N-butyl bromide was purchased from Spazmol® ampoule (manufactured by DEVA® Pharmaceutical Company), and diclofenac sodium was purchased from Sigma Aldrich® (D6899). Diclofenac sodium was initially dissolved in methanol, and distilled water was used for further dilution.
2.3 Histopathology and immunohistochemistry of tuba uterina
For histopathological and immunohistochemical studies there were three groups: control group, hyoscine applied group and diclofenac applied group (for each group n = 6). All samples were processed for embedding in paraffin using routine protocol. Sections 5 μm thick were cut on a rotary microtome (Leica RM2245) and stained with haematoxylin and eosin (H&E) for histopathological examinations. Additional sections were used for immunohistochemical staining. Tissue samples were stored at 60°C overnight and then were deparaffinized by xylene for 30 min. After dehydration of the sections with ethanol, they were washed with distilled water. The tissues were then treated with 2% trypsin at 37°C for 15 min and incubated in 3% hydrogen peroxide solution for 15 min to inhibit endogenous peroxidase activity. Then, sections were incubated with anti COX-2 (sc-23983 Santa Cruz Biotechnology) primer antibody in a 1/100 dilution for 18 h at +4°C. They were then given an additional three five washes in phosphate-buffered saline (PBS), followed by incubation with biotinylated IgG and administration of streptavidin peroxidase (Histostain Plus kit cat no: 85-9043, Invitrogen). After washing the secondary antibody with PBS three times for 5 min, the sections were stained with diaminobenzidine (DAB-plus substrate kit, Invitrogen) to detect the immunoreactivity and then stained with Mayer's haematoxylin (72804E, Microm, Walldorf, Germany) for counterstaining. They were covered with mounting medium (Clear Mount, Mounting Medium Ref: 008110 Invitrogen, USA) and observed with light microscopy (Olympus BX-43, Tokyo, Japan). Two randomly selected areas were scored, and in sections where all the staining appeared intense, one random field was chosen. At least 100 cells were scored per X40 field for each tissue in all the groups. All sections were scored in a semi-quantitative fashion, by considering both the intensity and percentage of cell staining. Intensities were classified as 0 (negative staining), 1 (mild staining), 2 (moderate staining) and 3 (intense staining).
2.4 Statistical analysis
The effect of diclofenac sodium and hyoscine-N-butyl bromide on basal contractions was expressed as % of basal mean tension. The relaxant effect of diclofenac sodium and hyoscine-N-butyl bromide on tissues contracted with KCl was expressed as % of KCl contraction.
Emax represents the maximum relaxation response. The data were expressed as a mean ± standard error of the mean (SEM). Statistical analysis was performed by two-way analysis of variance, post hoc Bonferroni test in the case of multiple concentration comparisons. The paired Student's t-test was used for two paired groups comparisons (GraphPad Prism 9.3.1, San Diego, CA, USA). Hystological data were analysed using the Mann–Whitney test. The values were expressed as the mean ± SEM of independent experiments. p values <0.05 were considered statistically significant.
3 RESULTS
3.1 The effect of cumulative diclofenac sodium and hyoscine-N-butyl bromide administration on basal mean tension
Raw recordings of the effects of hyoscine-N-butyl bromide and diclofenac sodium on basal mean tension are presented in Figure 1.
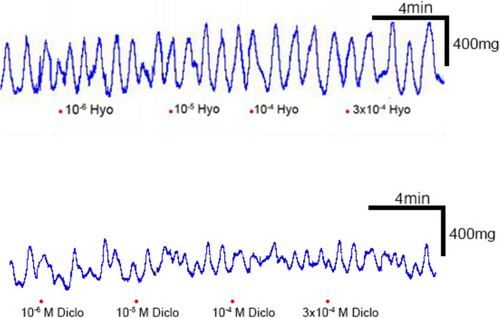
Diclofenac sodium and hyoscine-N-butyl bromide did not significantly change the basal mean tension value in tubal strips at all concentrations (p > 0.05) (Figure 2).
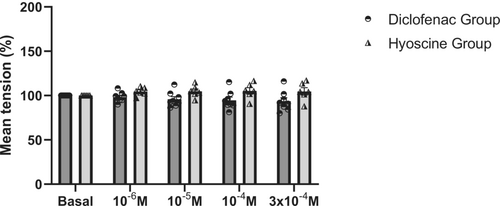
Basal mean tension for all doses was not statistically different in the diclofenac and hyoscine groups (p > 0.05) (Figure 2).
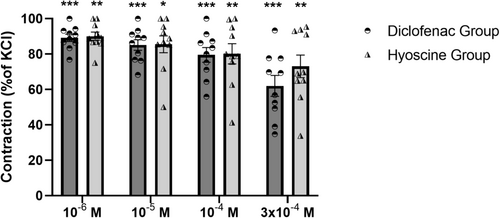
3.2 The effect of cumulative diclofenac sodium and hyoscine-N-butyl bromide administration on KCl induced contractions
Raw recordings of the effects of hyoscine-N-butyl bromide and diclofenac sodium on KCl induced contractions are presented in Figure 3.
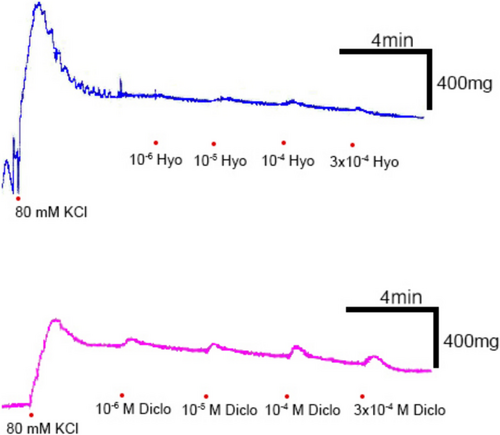
Both diclofenac sodium and hyoscine-N-butyl bromide relaxed KCl-contracted tissues statistically significantly at all concentrations starting from 10−6 M. Although this relaxation appeared to be greater in the diclofenac group, it was not statistically different from the hyoscine group at all concentrations (p > 0.05) (Emax ± SEM for diclofenac group = %37.96 ± 5.91; Emax ± SEM for hyoscine group = %26.89 ± 6.38; p = 0.22) (Figure 4).
3.3 The histopathological evaluation
The typical ciliated single-layered columnar epithelium of the fallopian tube and the tunica intima (TI) layer is clearly visible in the control tissue. The regular arrangement and normal morphological structure of the smooth muscle cells belonging to the tunica media (TM) layer are seen in the control group. In the diclofenac group (B), the epithelial structure is impaired, the epithelium is thinned and the ciliated cells are decreased. The TI layer has become very thin in places and has lost its regular appearance. In the TM layer, the connections between smooth muscle cells are broken, and there are edematous parts between the cells. In the hyoscine group, the TI layer was thinned and the epithelium lost its regular appearance. Along with a certain level of damage was observed in the TI layer of the hyocine tissue, the TM layer was better than the diclofenac group (Figure 5).

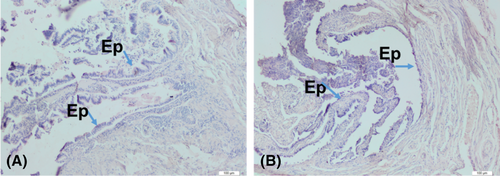
3.4 The immunohistochemical evaluation
In the control group, a weak (+) staining was observed in the epithelial part of the fallopian tube. However, no staining was observed in the diclofenac group (Figure 6).
4 DISCUSSION
In our study, while diclofenac sodium and hyoscine-N-butyl bromide did not significantly change the basal mean tension, they decreased the contractions induced by KCl statistically significantly. The relaxant effect of diclofenac sodium and hyoscine-N-butyl bromide on KCl-contracted tissues was not statistically significantly different from each other. This finding indicates that the in vitro relaxant effect of diclofenac sodium on the fallopian tube in contracted tissue is similar to hyoscine-N-butyl bromide. Therefore, it has the potential to be used as an alternative to hyoscine-N-butyl bromide in premedication in HSG used for the diagnosis of tubal occlusion.
According to histopathological analysis, both diclofenac and hyoscine applied tuba uterina tissues had a certain amount of damage. Since the histological examination of the diclofenac and hyoscine groups was performed after the pharmacological experiments, this damage may have occurred due to the experimental process. This is a limitation of our studies.
Diclofenac inhibits PG synthesis, and its relaxant effect on contracted tissues may be due to inhibition of PGs. The fact that the presence of COX-2 enzyme in the fallopian tube was demonstrated by immunohistochemical studies in our study and that COX-2 inhibition was demonstrated in the diclofenac-treated tissue supports this finding. The absence of staining with COX-2 primary antibody in the diclofenac administered group provides information that COX-2 expression may have decreased in epithelial cells. Kaur and Sanyal demonstrated that COX-2 expression was lower, notably in the diclofenac-treated group in the colonic mucosa. Diclofenac significantly inhibited the expression of COX-2.16
In vitro administration of PGs has been shown to regulate human fallopian tube contraction.17 Lindblom et al. showed the different effects of PGE2 and PGI2 on the circular and longitudinal muscles of the fallopian tube. In vitro administration of PGE2 and PGI2 inhibited the circular muscle and stimulated the longitudinal muscle.18 In another study, in vitro administration of PGE2 to longitudinal fallopian tube strips increased the AUC of contractions dose dependently.17
PGE1 showed a dose-dependent inhibitory effect on human fallopian tube contractions. PGF2α has been shown to increase human fallopian tube contractions.17 As a result, an increase or decrease in tubal contractions has been observed with in vitro application of different types of PGs to the fallopian tube. In our study, the relaxation observed with the application of diclofenac sodium in the fallopian tube tissue contracted with KCl was probably related to the distribution of PG receptors in that region, and the net effect emerged as relaxation.
PGI2 and PGE2 are the main products of PG biosynthesis in the human fallopian tube. It is known that the expression of EP1 among PGE2 receptors EP1–EP4 and PGF2α receptor FP is highest in the ampullar-isthmic region of the fallopian tube.17 Postreceptor second messengers of the EP1 receptor are DAG/IP3. It subsequently increases intracellular Ca2+ levels. In vitro administration of PGE2 and PGI2 has been shown to inhibit the circular muscle of the fallopian tube and stimulate the longitudinal muscles.18 In our study, the relaxation observed with the administration of diclofenac sodium in the fallopian tube contracted by KCl may have occurred due to less stimulation of the EP1 receptor, which is expressed more highly than other PG receptors in the ampullar part of the fallopian tube.
Today, hyoscine-N-butyl bromide, a spasmolytic agent, is commonly used in premedication in the diagnosis of proximal tubal occlusions. Premedication with hyoscine-N-butyl bromide prior to HSG may reduce the rate of false positive tubal obstruction. This may reduce unnecessary second HSG or laparoscopy procedures. Thus, patients can be prevented from being exposed to unnecessary procedures, and the increase in complications and mortality rates can be prevented. In our study, we found that diclofenac sodium was as effective as hyoscine-N-butyl bromide in relaxing contracted tissue. Therefore, the use of diclofenac sodium, which can benefit pain control with its smooth muscle relaxant effect in addition to its analgesic properties, can be an important alternative to hyoscine-N-butyl bromide in proximal tubal occlusions. In addition to the spasmolytic effect of hyoscine-N-butyl bromide, the analgesic effect of diclofenac sodium may contribute to patient comfort. Our study is the first study in this area, and further studies are needed to support and improve this finding.
5 CONCLUSION
Diclofenac may have the potential to be used as an alternative to hyoscine-N-butyl bromide in premedication in HSG.
AUTHOR CONTRIBUTIONS
All of the authors declare that they have all participated in the conception, design, execution, acquisition, analysis and interpretation of data and that they have approved the final version.
ACKNOWLEDGEMENTS
This research was presented as an oral presentation on 23 November 2023, at “27th National 2nd International Pharmacology Congress.”
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.