What paediatric obesity treatment programmes work, and how can we measure their success?
The medical significance of paediatric obesity needs little introduction. It is estimated that in 2025, there will be more than 268 million children and adolescents who are overweight and obese around the globe 1. Despite numerous novel and exciting findings on the gut microbiome, xenobiotics and environmental, genetic and epigenetic changes relating to paediatric obesity, the adiposity of children is still related to their diet and levels of activity 2. Therefore, until those exciting findings from basic science studies are translated into clinical treatments, we have to continue to focus our efforts on the fundamental aspects of energy balance when treating children with obesity.
The causes of obesity in children and its treatment were already well understood decades ago. In 1920, Professor C G Kerley wrote that ‘Exceedingly fat children will usually be found to be hearty eaters and of inactive habits’, adding that ‘Obesity is rarely a serious condition and ordinarily requires little more than certain restrictions in diet and regularity in exercise’ 3. Little has changed a century later, as dietary modifications and regular physical activity are still the mainstay of therapy in many countries 4.
While eating less and exercising more are probably an axiom with regard to obesity treatment, the well-known problem is how to achieve this effectively in the long term. That is where scientific research and the strength of the evidence are of utmost importance. Dozens of paediatric obesity treatment programmes that have administered different combinations of diet, exercise and behavioural changes have been carried out over the years. Updated meta-analyses of interventions for the treatment of children and adolescents with overweight or obesity were published in 2016 and 2017 5-7. Clinicians might be extremely discouraged to learn from these key papers that the general quality of evidence is still low to moderate, probably due to the inherent limitations of such research. Examples of such limitations include the following: the natural lack of blinding, the limited sample sizes, the inability to completely administer all components of the recommended diet and exercise regimes, the cultural, ethnic and socio-economic diversity of humans and the high dropout rates. In addition, the content and duration of the interventions, the delivery modes, the comparators and the anthropometric outcomes have varied greatly across trials. Finally, we are faced with disappointing small effect sizes and magnitudes of mean weight, body mass index (BMI) and BMI standard deviation score (BMI SDS) changes despite such efforts. This should encourage us to re-think programme structures, or possibly to carry out an additional form of analysis?
In this issue of Acta Paediatrica, Dalla Valle et al. 8 evaluated the efficacy of a treatment programme for children and adolescents with obesity in Finland and explored the factors that contributed to its long-term success. This family-based multidisciplinary programme included all of the anticipated nutritional, exercise and behavioural counselling components. Yet several features of this paper are noteworthy. The most important feature is the high success rate and its presentation. Very frequently, authors describe pre–post changes of mean BMI and BMI SDS values. These authors do the same and show small reductions in the mean BMI SDS of −0.10, −0.09 and −0.06 after 12, 24 and 36 months, respectively. These were not very impressive at first glance, even though they were statistically significant. However, the categorical analysis should form part of any study analysing treatment success, as that identifies the proportion of children that had BMI SDS reductions and clinically meaningful reductions.
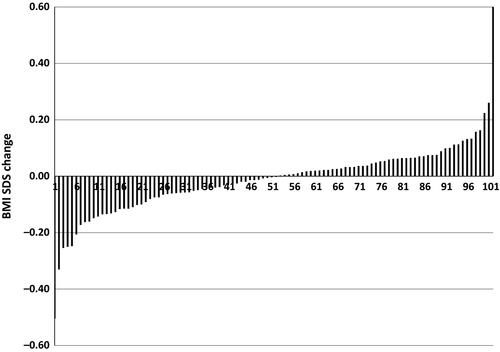
When Dalla Valle et al. 8 examined the proportions of participants with BMI SDS reductions, they found very encouraging results as follows: of the 493 children assessed at 12 months, 60% demonstrated a reduced BMI SDS from baseline, with 39% having a clinically meaningful reduction of at least 0.25 SDS 9. When such analyses are performed, we can become much more confident in the success rates of our obesity treatment programmes, as opposed to when we only analyse the average outcomes. We can easily demonstrate how a null change in mean BMI SDS does not at all suggest that a programme is ineffective. Figure 1 presents BMI SDS changes after a three-month multicomponent treatment for children with overweight and obesity from our centre. The mean BMI SDS change was zero, yet 50% of the children improved their anthropometric status. Looking at the average BMI SDS change alone would suggest that the programme had no effect, but this is only true if you look at average figures, as all the children in our programme either gained or lost weight in relation to their stature.
There are additional educational features in the article by Dalla Valle et al. 8. One is the clear reminder of the natural history of paediatric obesity, which was presented by the rise in BMI SDS in the year before the programme began. Therefore, even a halt in the rise in BMI SDS during treatment can be an initial positive effect, as in the saying ‘the glass is half full’. In addition, the relatively high adherence to the programme (80%) and its ability to maintain a meaningful BMI SDS reduction of −0.25 in more than one-quarter of the participants for three years was very encouraging for the programme leaders.
One of the main aims of the Dalla Valle et al. study was to recognise predictors of BMI SDS reductions, as several previous studies had attempted, yet with little success. Low BMI, high adherence, younger age and male sex were the most common findings. Conversely, in this study, a high BMI was identified as a predictor of success, as was the lack of acanthosis nigricans. This does not mean that we should give up on children who have a lower chance of success. On the contrary, we should offer them additional support and reinforcement to help them adhere to treatment. Predictors of success would probably differ between programmes, given the diversity of populations, ethnicities, socio-economic levels of the families, programme structures and the designated outcomes. Each programme should perform its own analysis in identifying the children who need more support, such as those on the far right side of Figure 1 in our case.
A final message relating to treating children and adolescents with overweight or obesity is the issue of body composition measurements, as opposed to just using body mass changes. Not enough studies that assess obesity treatment programmes have also measured and reported on body composition. In a meta-analysis of 44 trials of obesity treatment in youth, only 14 (32%) reported on body fat percentages 7. In a 2017 meta-analysis on children aged 6–11 years, only 11/70 (16%) studies presented fat percentage data that could be meta-analysed 6. Weight measurements need to be accompanied by estimates of body composition by any of the accepted methods, especially in growing children. In our own clinical experience, adolescents with obesity can gain 10, 12 or even 15 kg of fat-free mass over months and years of treatment, with frequent parallel reductions in fat mass and sometimes no net change in absolute mass. If only body weight or BMI were measured, such dramatic changes in body composition and fat percentages would not have been recognised and attrition would have been probable. This is also true for waist circumference measurements and their presentations as either crude values, waist-to-hip ratios or waist-to-height ratios. Many additional effects can occur ‘under the radar’ during obesity treatment. For example, in a 12-week resistance programme for adolescents with obesity, improvements in a long list of cardiovascular risk factors occurred, including reductions in total and visceral fat, but with no significant change in body mass 10. For the reasons detailed above, just using weight measurements in paediatric obesity treatment may be easier but would miss numerous changes in body composition and cardiovascular risk factors.
In summary, the paper by Dalla Valle et al. 8 describes a relatively effective paediatric obesity programme. It demonstrates several aspects related to reporting the success of such programmes and identifies several predictors of success. It is imperative that categorical analyses are used in such reports to best demonstrate the proportion of successful children. In addition, the analysis of body composition changes in children and adolescents adds significantly to the use of just body mass, BMI or BMI SDS in both clinical settings and research.
Funding
No funding to declare.
Conflict of Interest
No conflict of interests to declare.