Visual outcomes after surgery for childhood cataracts
Abstract
Purpose
To describe long-term objective and subjective visual outcomes in a group of Danish children after cataract surgery.
Methods
Follow-up examination of 56 children aged 7–18 years who had undergone uni- or bilateral cataract surgery. Subjective visual function was assessed using the Cardiff Visual Ability Questionnaire for Children (CVAQC) and compared to objective visual acuity for distance and near, contrast vision and stereopsis.
Results
Better visual acuity on the better seeing and contrast vision on worst seeing eye were significant predictors of increased subjective visual function in a multivariate analysis, p = 0.024. Children in the unilateral group had a significantly better CVAQC ratio compared to children in the bilateral group, median of 0.88 (range 0.50–1.00) versus 0.80 (range 0.55–0.98), p = 0.027. Reading small print, playing ball games and seeing friends in the playground were the most difficult CVAQC items in the unilateral group and reading small print, seeing the board in the classroom and seeing friends in the playground were the most difficult in the bilateral group.
Conclusion
Children with unilateral disease often have a healthy eye to support the operated eye, why they overall have better subjective visual function. Many of the most difficult visual tasks were related to academic activities which might hamper future academical capabilities.
Introduction
The global incidence of childhood cataract is estimated to be 1.8–3.6 per 10 000 children per year (Sheeladevi et al. 2016). Cataracts are responsible for 5–20% of childhood blindness worldwide making it a major cause of preventable blindness in children (Gilbert & Foster 2001; Sheeladevi et al. 2016). It is recommended that congenital cataracts should undergo surgery when the child is between 6 and 8 weeks to reach an optimal outcome (Birch et al. 2009; Lim, Buckley & Grace Prakalapakorn 2017; Stuart 2017). Juvenile cataracts can develop throughout childhood or remain visually insignificant, and the threshold for surgery should be tailored to the individual child. Studies describing long-term outcomes are scarce, presumably in part because surgery and early surgical follow-up are often performed in centralized centres whereas postsurgical follow-up and care is often performed in local centres.
Previous studies have focused on selected groups of patients, and focus has mainly been on visual acuity outcomes whereas the subjective visual function has only been the focus of a few studies (Birch, Cheng & Felius 2007; Kirwan, Lanigan & O'Keefe 2011; Castañeda et al. 2016; Tailor et al. 2017; Fox, Keefe & Lanigan 2018). We aimed at investigating the subjective visual function in children operated for childhood cataracts and to evaluate which factors affect their subjective vision and which daily situations these children find challenging due to their impaired vision.
Materials and methods
Recruitment of study participants
We investigated the long-term outcome of patients who had undergone cataract surgery during childhood (<15 years of age) between 2000 and 2018 and who had been followed at our institution. Since 2010, surgery for cataracts <6 years of age has been a highly specialized treatment in Denmark that takes place in Copenhagen (Rigshospitalet) and Aarhus (Aarhus University Hospital). After surgery, the children can be followed at the operating hospital or in local hospitals depending on the age at time of surgery, refractive correction (e.g. use of aphakia contact lenses), distance from residential place to Copenhagen/Aarhus and the clinical course of the child. In general, children operated <6 months of age were left aphakic and children operated >6 months had an intra ocular lens (IOL) implanted.
We invited children between the age of 7 and 18 at the time of examination who had undergone surgery for uni- or bilateral, congenital or juvenile cataract via mail to participate in the study. Mail invitations were followed by a telephone call if the children and their parents did not respond to the initial invitation. Children with severe intellectual disabilities were not invited as participants had to be able to comply with examination procedures. In addition, only children who lived in the Capital or Zealand region of Denmark were invited.
Controls
Concerning the data related to each eye (e.g. distance and near visual acuity, biometrical measurements, and diagnosis of glaucoma), the non-affected eyes in the unilateral cases were used as controls.
Examinations
All objective visual examinations were performed using the best optical correction for distance and near. Subjective refractioning was performed before the visual acuity test for far and near in all children able to comply. The subjective refractioning was guided by the child's own prescription and objective refractive measures performed using a Retinomax K Plus 3 autorefractor (Righton, Tokyo, Japan). Best-corrected visual acuity at distance was measured using HOTV 3 Meter visual chart (HOTV3M) (Precision Vision Inc., Woodstock, IL, USA) and was reported in logMAR (logarithm of the Minimum Angle Resolution). Near visual acuity was measured using the Precision Vision HOTV Near Vision Card (HOTV40CM) (Precision Vision, Inc) at 40 cm distance using the child's near-correction. For near visual acuity testing, M-unit was used where 0.40 M-units corresponds to 0.00 LogMAR. Near visual acuity was determined as the line with the smallest letter size which the child could read a minimum of three of the five letters. The level of visual impairment was categorized according to WHO criteria (WHO 2018) with mild visual impairment as a visual acuity worse than 0.3 logMAR, moderate visual impairment worse than 0.5 logMAR, severe visual impairment worse than 1.0 logMAR and blindness worse than 1.3 logMAR. Stereopsis was measured using the TNO-test (Lameris Ootech, Ede, The Netherlands) using the child's near-correction. Best-corrected contrast vision was tested using the Freiburg Visual Acuity and Contrast Test (Bach 2007) in a completely dark room using computer with screen brightness set to full. Presence of strabismus or nystagmus was evaluated by inspection and Hirschbergs test.
Subjective visual function was evaluated using a Danish translation of the Cardiff Visual Ability Questionnaire for Children (CVAQC) (Khadka et al. 2010). The Danish version the CVAQC consisted of 24 questions on vision in daily visual situations distributed on 7 subscales dealing with education, near vision, distance vision, getting around, social interaction, entertainment and sports. The question related to school lessons on geography was omitted since this was not applicable to the Danish school system. The child was informed to rate his or her vision using any low vision aids in the 24 specific situations as: very easy (4 points), easy (3 points), difficult (2 points) or very difficult (1 point). The CVAQC ratio was calculated as the ratio between the number of points scored by each child and the maximal possible score (96 points). If a child could not answer a question, for example using public transportation bus/train (as some young children did not use public transportation) the amount of possible points related to that question (4 points) was subtracted from the maximal possible score. To compare which CVAQC subcategories and questions between the unilateral and the bilateral group we created grouped ratios by dividing the sum of the CVAQC-points of all children in each group by the highest possible amount of points attainable by each group, respectively.
Medical files
Medical files were assessed for information relevant to the study such as the date of the cataract surgery and subsequent surgeries, if any, implantation of an IOL, postoperative complications and systemic and ocular comorbidities, for example microphthalmia, secondary glaucoma, strabismus and nystagmus. Congenital cataracts were defined as those present <1 year of age. Glaucoma was defined according to a classification system for paediatric glaucoma (Thau et al. 2018). Eyes were defined as having glaucoma if meeting two of the following criteria: intraocular pressure > 21 mmHg, visual field defects, optic nerve cupping, corneal findings such as Haab striae or increased corneal diameter, increased axial length (AL) or myopic shift that outpaced normal growth. Also, if the eye had undergone surgery for glaucoma it was regarded as a glaucoma eye. Eyes meeting one criterion only, except for glaucoma surgery, were considered glaucoma suspect.
Optical biometry
Swept source optical coherence tomography based optical biometry was performed using the IOLmaster 700 (Carl Zeiss Meditec Inc., Dublin, CA, USA) providing information about the AL, anterior chamber depth, and white-to-white (WTW). Microphthalmia was defined as an AL of <20 mm and WTW <10 mm (Feldkamp et al. 2014) or if an ophthalmologist had diagnosed the child with microphthalmia.
Permissions
This study followed the tenets of the Helsinki declaration and was approved by The Committee on Health Research Ethics for the Capitol Region Denmark (j.nr.: H-17037037) as well as the Danish Data Protection Agency (RH-2018-47, I-Suite no. 6244).
Statistical analysis
When comparing operated and non-operated healthy eyes of children with unilateral cataract (control), only one eye (the right eye) of the bilaterally operated children was included. p-values <0.05 were regarded as statistically significant. Most data did not follow a normal distribution (Shapiro–Wilks test of normality, p < 0.05). When data followed a normal distribution, unpaired or paired t-test was performed and Wilcoxon rank-sum test or Wilcoxon signed-rank test when not. Multiple regression analysis was used to assess visual outcome predictors and adjusting for possible confounders. Data were collected and managed using REDCap electronic data capture tools (Harris et al. 2009). Statistical analysis was performed using Rstudio (RStudio Inc., Boston, MA, USA) (RStudio Team 2016).
Results
Invitations were sent to 93 children who met the inclusion criteria, 56 (60%, 30 male and 26 female) agreed to participate. Of the 56 children, 28 had bilateral cataract surgery and 28 unilateral surgery. One participant with bilateral Peters anomaly but unilateral cataract surgery was excluded from the control group. The median age at time of surgery for operated eyes was 1132 days (range 42–4187). Seventeen children were aphakic with a median age at surgery of 91 days (range 42–1569), and 39 children were pseudophakic with a median age at surgery of 1474 days (range 151–4187). Thirty eyes (19 children) had surgery <1 year of age, and six eyes (four children) had surgery within the first 8 weeks of life. An overview of included patients is presented in Table 1.
| Bilateral | Unilateral | All operated eyes | Control eyes | |||
|---|---|---|---|---|---|---|
| Aphakia | Pseudophakia | Aphakia | Pseudophakia | |||
| Male/Female | 8/4 | 7/9 | 1/4 | 14/9 | 30/26 | 15/12 |
| Visual acuity (logMAR) | 0.64 (0.02–1.06) | 0.1 (−0.1 to 0.98) | 1.1 (0.6–1.1) | 0.8 (0.06–1.1) | 0.62 (−0.1 to −1.1) | −0.06 (−0.3 to 0.2) |
| Near vision (M)) | 1.25 (0.25–6.30) | 0.63 (0.40–6.30) | 3.50 (2.00–5.00) | 2.25 (0.25–8.00) | 1.43 (0.25–8.00) | 0.40 (0.25–0.63) |
| Eyes unable to read 8.0 M | 0 (0%) | 0 (0%) | 3 (60%) | 3 (13%) | 6 (11%) | 0 (0%) |
| Refractive correction (glasses/contact lenses) | 6/6 | 16/0 | 1/4 | 21/2 | 44/12 | – |
| Contrast vision (logCS)* | 1.57 (0.07–2.31) | 1.82 (0.57–2.70) | 0.00 (0.00–0.00) | 0.60 (0.00–2.70) | 1.08 (0.00–2.70) | 2.70 (1.18–2.70) |
| CVAQC-score | 0.72 (0.55–0.89) | 0.86 (0.58–0.98) | 0.92 (0.54–0.94) | 0.86 (0.50–1.00) | 0.84 (0.50–1.00) | – |
| Age at surgery (days) | 103 (42–1570) | 1920 (151–4187) | 88 (49–1474) | 1334 (251–3877) | 1132 (42–4187) | – |
| Age at follow-up (years) | 11.1 (7.5–18.1) | 12.61 (8.6–18.00) | 9.0 (8.0–15.3) | 10.6 (7.5–16.1) | 11.2 (7.5–18.1) | 10.4 (7.5–16.1) |
| Axial length (mm) | 21.74 (20.15–28.52) | 22.73 (20.05–24.89) | 22.36 (20.39–31.06) | 22.76 (20.77–27.36) | 22.49 (20.05–31.06) | 22.92 (21.60 – 24.63) |
| Axial length difference > 1mm | 2 (17%) | 1 (6%) | 3 (60%) | 9 (39%) | 15 (27%) | – |
| Stereopsis | 0 (0%) | 5 (31%) | 0 (0%) | 3 (13%) | 8 (14%) | – |
| Strabismus | 7 (58%) | 5 (31%) | 3 (60%) | 11 (48%) | 26 (46%) | 0 (0%) |
| Glaucoma | 5 (42%) | 1 (6%) | 3 (60%) | 1 (4%) | 10 (18%) | 0 (0%) |
| Nystagmus | 8 (67%) | 1 (6%) | 1 (20%) | 0 (0%) | 10 (18%) | 0 (0%) |
| Microphthalmia | 0 (0%) | 0 (0%) | 3 (60%) | 4 (17%) | 7 (13%) | 0 (0%) |
- Values are presented as median (range) except when numbers are given. logMAR = logarithm to the minimal angle of resolution; M = letter size at 40 cm distance, 0.40M-units corresponds to 0.00LogMAR; logCS = logarithm to contrast sensitivity; CVAQC = Cardiff visual ability questionnaire for children; mm = millimetre. In the bilateral groups visual acuity, near vision, contrast vision and axial length represents the right eye to avoid paired data. Stereopsis, strabismus and glaucoma are presented as number of children. Microphthalmia are given in number of eyes affected.
- * Visual acuity was too poor to complete the contrast vision test in one eye in the bilateral pseudophakic group, two eyes in the bilateral aphakic group, five eyes in the unilateral aphakic group and six eyes in the unilateral pseudophakic group.
Visual acuity
Best-corrected distance visual acuity for all operated eyes was 0.52 logMAR (median, range −0.1 to 1.1). The median near visual acuity was 1.43M (0.25–8.00) but six eyes (11%) could not read 8.00M (Table 1). One child had mild, six had moderate and one had severe visual impairment according to WHO definitions (WHO 2018), but no children were blind. All children with visual impairment were bilateral aphakic except for one child with unilateral aphakia and bilateral Peters anomaly. In the unilateral group, 23 of the 28 (82%) operated eyes had moderate visual impairment or worse and 6 eyes were blind. In the bilateral group, 21 of the 56 operated eyes (38%) had moderate visual impairment or worse and 3 eyes were blind. In the bilateral group, there was no significant difference in the visual outcome between the right or left eyes (p = 0.339 using Wilcoxon signed-rank test) or between the eye that was operated first or last (p = 0.626). Older age at surgery and bilateral surgery were predictors of better visual acuity using multivariate analysis, p < 0.001, whereas older age at the examination, aphakia or pseudophakia did not affect visual acuity in a multivariate analysis.
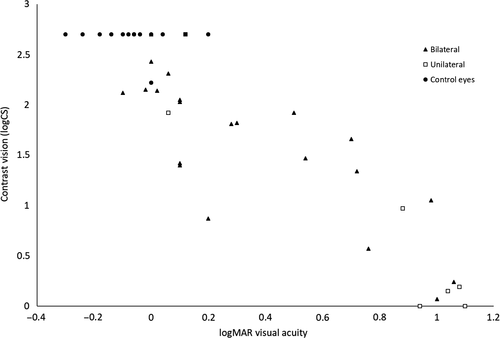
Contrast vision
Contrast vision could be measured in 77 out of the 112 examined eyes. Unoperated control eyes had a significantly better contrast vision with a median of 2.70 LogCS (range 1.18–2.70) compared to operated eyes in the unilateral (median 0.18 LogCS (range 0.00–2.70), p = 0.001 Wilcoxon rank-sum test) and the bilateral group (median 1.81 LogCS (range 0.07–2.70), p < 0.001), see Fig. 1. Bilateral surgery was the only significant predictor of a better contrast vision, p = 0.002. Age at surgery, age at the examination and lens status were not significantly associated to contrast vision outcome in a multivariate analysis.
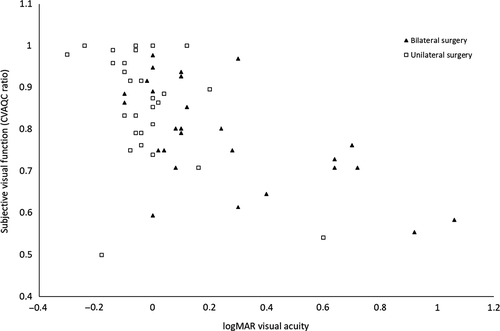
Subjective visual function
The subjective visual function (CVAQC ratio) was significantly better in bilateral pseudophakic children compared to bilateral aphakic children, with a median CVAQC ratio of 0.86 (range 0.59–0.98) versus 0.72 (range 0.55–0.89), p = 0.006. For children with unilateral surgery, there was no effect of lens status on subjective visual function median CVAQC ratio of 0.87 (range 0.50–1.00) versus 0.92 (range 0.54–0.94), p = 1.00. Children in the unilateral group had a significantly better CVAQC ratio compared to children in the bilateral group, median CVAQC of 0.88 (range 0.50–1.00) versus 0.80 (range 0.55–0.98), p = 0.027.
Better visual acuity on the better seeing eye was a significant predictor of increased subjective visual function, as was better contrast vision of the worst seeing eye, p = 0.024, see Fig. 2. There was no significant effect on subjective visual function of visual acuity of the worst seeing eye, contrast vision of the better seeing eye, bilateral compared to unilateral surgery, age at surgery or at examination in a multiple regression analysis. When restricting the analysis to the subjective distance vision subscale of the CVAQC, we found better distance visual acuity of the better seeing eye and older age at the examination to be associated to a better CVAQC ratio after adjusting for the abovementioned factors, p = 0.041. When investigating the relationship between visual acuity for near and the near vision subscale of the CVAQC, we found no significant association after adjusting for the abovementioned factors, p = 0.390.
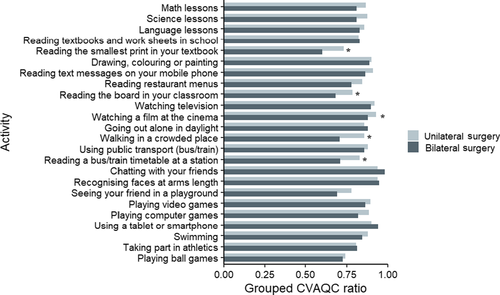
Using grouped CVAQC ratios, we found the three most difficult CVAQC items for the unilateral group to be reading the smallest print in textbooks (0.73), playing ball games (0.74) and seeing friends in the playground (0.78). The three easiest visual tasks were recognizing faces at arm's length (0.94), chatting with friends (0.94) and watching a film at the cinema (0.93). In the bilateral group, the three most difficult CVAQC items were reading the smallest print in textbooks (0.56), reading on the board in the classroom (0.65) and seeing friends in the playground (0.66). The easiest were chatting with friends (0.96), recognizing faces at arm's length (0.92) and using tablets or smartphones (0.90), see Fig. 3.
Discussion
We investigated the long-term objective and subjective visual outcomes of Danish children operated for congenital or juvenile cataracts. The subjective visual function was evaluated using a Danish version of the CVAQC. Overall, subjective visual function was associated with visual acuity of the better seeing eye and contrast vision of the worse seeing eye. No children were blind, but one had severe, six had moderate and one child had mild visual impairment according to WHO criteria (WHO 2018). In general, children operated for bilateral cataract had better visual outcomes in the operated eyes than unilateral cataract eyes. Subjective visual outcome was better in children who had unilateral cataract surgery because all of them, except one with bilateral Peters anomaly, had good visual acuity in the unoperated eye.
A few studies have focused on the subjective vision of cataract operated children but in different age groups (range 0.3–33 years) using different questionnaires or structured interviews (Birch, Cheng & Felius 2007; Kirwan, Lanigan & O'Keefe 2011; Castañeda et al. 2016; Tailor et al. 2017; Fox, Keefe & Lanigan 2018). One study on children aged 2–16 years reported a trend towards better CVAQC with better visual acuity but was underpowered to show a significant association (Tailor et al. 2017). A study on young adults who had undergone cataract surgery in the first year of life found an association between the visual acuity of the best seeing eye and the vision-related mental health subscale evaluated using the National Eye Institute Visual Function Questionaire-25 (NEI-VFQ-25) (Kirwan, Lanigan & O'Keefe 2011). However, the follow-on study containing many participants from the original study could not reproduce this finding but they found distance and near activity subscales to correlate with the visual acuity of the worse seeing eye in the bilateral group (Fox, Keefe & Lanigan 2018). Maybe this is caused by the different questionnaires used in the studies, the lower number of participants in the follow-on study or that the visual acuity of the worse seeing eye becomes more important later in life.
Visual outcomes after surgery for childhood cataracts are often guarded even if patients and parents adhere to postsurgical treatment regimens and complications are discovered and treated timely (Haargaard et al. 2009; Lambert et al. 2016). Our findings agree with previous studies that report trends towards lower physical, psychosocial and vision-specific quality of life in children, teenagers and young adults operated for bilateral cataract when compared to unilateral cataract using the Pediatric Quality of Life inventory (PedsQL inventory) (Varni 1998), NEI-VFQ-25 (Kirwan, Lanigan & O'Keefe 2011; Fox, Keefe & Lanigan 2018), Children's Visual Function Questionnaire (CVFQ) (Birch, Cheng & Felius 2007) or the CVAQC (Tailor et al. 2017), telling us that children operated for unilateral cataracts have better subjective vision compared to children operated for bilateral cataracts across age groups, countries and questionnaires. The strongest predictor of a better CVAQC ratio in our study was good vision of the better seeing eye which likely explains the better subjective visual function in the unilateral group. Visual acuity of operated eyes in the unilateral group was poor but this did not seem to influence the children's subjective vision.
In general, children in our study rated subjective visual functions related to social interactions and entertainment high, such as use of smartphones and tablets, chatting with friends, watching television or playing video games. However, subjective visual functions related to near vision and academic achievements such as reading the smallest print in textbooks and reading on the board in the classroom were generally rated low. One could fear difficulties in such crucial visual abilities might have a negative impact on future academical capabilities. Children in the bilateral group had several significantly worse grouped CVAQC ratios compared to the unilateral group mainly explained by the importance of the visual acuity in the better seeing eye on subjective visual function.
Older age at surgery and bilateral surgery were associated with better visual acuity. That older age at surgery is associated to a better visual acuity outcome is consistent with a previous study (Ledoux et al. 2007) and is explained by the fact that children who first need surgery later in life usually have a normal visual development as the cataract only develops after the period of visual maturation. Aphakic eyes had worse visual outcomes compared to pseudophakic eyes, but when adjusting for age at surgery, age at examination and bilateral versus unilateral surgery then lens status alone was not associated with a better or worse CVAQC ratio or visual acuity.
As with all studies, this study has some limitations. Because of the low prevalence of childhood cataracts, we were not able to restrict the study to children who had undergone cataract surgery at specific time-points, for example before 6 months of age, or children who were only aphakic or pseudophakic. For some of the children, quite long time had elapsed since cataract surgery as we wanted the children to be old enough to comply with procedures. In this way, we do not know how cataract surgery impacts subjective visual function immediately after surgery but as the aim of the study was to evaluate subjective visual function in a steady-state situation when the child was used his/her visual function, this is less of a limitation. Also, we only included a smaller group of all those children in Denmark who have undergone cataract surgery. We used an age-limit and we excluded children with severe disabilities to be sure that participants would be able to comply with procedures. Sixty per cent of invited children participated. Unfortunately, the ethical board permission did not allow us to access the medical files of non-attendants and hence we do not know if attendants are representative of all children with childhood cataracts in Denmark.
In summary, we found a better CVAQC ratio after surgery for childhood cataracts to be associated with a better visual acuity of the best seeing eye and a better contrast vision of the worse seeing eye. Factors such as age at surgery, lens status, bilateral or unilateral cataract alone did not predict CVAQC ratio when taking relevant measures into account. As children with unilateral disease often have a healthy eye to support the operated eye, they have better CVAQC ratios. The self-perceived most difficult visual tasks were related to academic achievements such as reading the smallest print in textbooks and to read on the board in the classroom. Difficulties in such crucial visual abilities might hamper future academical capabilities.