Intra-operative microscope-integrated swept-source optical coherence tomography guided placement of Argus II retinal prosthesis
This project was funded by the NIH Bioengineering Research Partnership Grant: R01- EY-023039 “Intraoperative OCT Guidance of Intraocular Surgery” (Izatt/Toth).
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Paul Hahn reports a consulting agreement with Second Sight Medical Products, Inc. Sylmar, CA. No other disclosures were reported. The authors have full control of all primary data.
The Argus II Retinal Prosthesis System (Second Sight Medical Products, Sylmar, CA, USA) is an epiretinal device approved for implantation in severe retinitis pigmentosa (RP). During implantation, the most challenging surgical manoeuvre is correct positioning and tacking the electrode array to the retina (Rizzo et al. 2014). Proximity of electrodes to the retinal surface is important for proper function and is challenging to confirming intra-operatively as the surgical microscope may not provide optimal axial resolution (Ahuja & Behrend 2013). We demonstrate a research-prototype microscope-integrated high-speed (100 000 A-scans/second) swept-source optical coherence tomography (MIOCT) device for intra-operative optical coherence tomography (OCT) acquisition simultaneous with surgical manoeuvres allowing intra-operative array position confirmation (Hahn et al. 2013).
A 46-year-old phakic male with advanced RP and bare light-perception vision underwent Argus II implantation. Following phacoemulsification, the coil and scleral band were positioned as described previously (Rizzo et al. 2014; Ho et al. 2015). A complete vitrectomy was performed, and the array tacked centred over the fovea, followed by closure (Rizzo et al. 2014; Ho et al. 2015).
Intra-operative OCT images were acquired at 2-10 volumes/second, concurrent with live surgical manoeuvres. The acquired MIOCT data were processed in real time and displayed in three formats: B-scans, en face maximum intensity projections (MIP), and denoized volumes rendered in real time with lighting, edge and depth-enhanced ray casting. All three formats were projected on a wall-mounted operating suite display for real-time surgeon feedback.
The MIOCT imaging protocol consisted of 6 × 7.5 × 7.5 mm scans acquired during array positioning, tack placement and post-tacking. Specific advantages were noted in each step:
Preretinal tack placement: Microscope-integrated swept-source optical coherence tomography (MIOCT) permitted real-time confirmation of appropriate array positioning prior to proceeding with tack placement (Fig. 1A shows the array tilted in relation to the retina as it is lowered to the retinal surface). Microscope-integrated swept-source optical coherence tomography (MIOCT) can also determine the adequacy of epiretinal membrane peel, if performed (Rizzo et al. 2014).
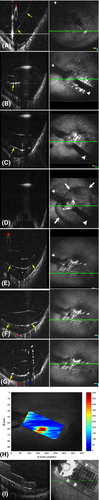
Retinal tack placement: Microscope-integrated swept-source optical coherence tomography (MIOCT) allowed real-time visualization of retinal tack placement (Video S1) (Fig. 1B–F). When using the tack forceps to secure the electrode array over the macula, pressure is applied perpendicular to the retinal surface to penetrate the tack through the sclera (Sight 2013). On B-scan images, array boundaries were visualized as hyper-reflective surfaces and the array handle as a hyper-reflective oval. As pressure was applied with the tack forceps, array apposition was directly visualized on OCT.
Postretinal tack placement: After release of the tack forceps, MIOCT permitted intra-operative confirmation of electrode-inner retinal surface apposition (Fig. 1E–G) and centration over the foveal pit. Electrode-inner retinal surface distances, which have been shown to correlate with threshold levels of electrode stimulation, were determined by manually creating a distance map that also confirmed array centration over the foveal pit (Fig. 1H) (Ahuja et al. 2013). Array position variability in the intra-operative prone position and the postoperative standing or sitting position has been questioned (Rizzo et al. 2014). We confirmed this stability by comparing intra-operative and postoperative OCT scans (Fig. 1I).
Dislodged or improperly positioned retinal tacks were reported in 2/30 (6.7%) eyes during clinical trials. Improper positioning was not noted in either case intra-operatively and both required revision surgeries (Ho et al. 2015). Microscope-integrated swept-source optical coherence tomography (MIOCT)-based intra-operative confirmation of array position can potentially avoid this scenario. Microscope-integrated swept-source optical coherence tomography (MIOCT) allows near real-time capture of volumetric data and the ability to view individual B-scans in any area of interest. This is in contrast to spectral-domain-based intra-operative OCT systems, wherein an area of interest needs to be identified prior to image acquisition, and maintained in the same plane intra-operatively, which is challenging.
In conclusion, Argus II implantation with a prototype MIOCT device was successfully performed, enabling intra-operative cross-sectional visualization. MIOCT allowed real-time confirmation of array position pre-, intra- and post-tack placement and confirmed the adequacy of tacking in securing the array in close contact with the retina. This may help optimize outcomes and prevent known complications of Argus II implantation, and further investigation into its utility is warranted.