One hundred-year-old human corneal and transplanted corneal graft endothelium
Abstract
Purpose
To investigate and analyse one hundred-year-old endothelial cells of human transplanted corneal grafts and compare them with intact endothelium of unoperated eyes.
Subjects and methods
Specular microscopy was performed on seven individuals (14 eyes) aged >100 years and on seven transplanted corneas with endothelial cells of at least 100 years old. All keratoplasties were performed by the same surgeon (PR) 25–35 years before the time of examination. As controls, 14 unoperated healthy individuals (26 eyes) of 90–100 years, 12 individuals (24 eyes) of 48–52 years, 12 students (24 eyes) of 19–24 years and 11 children (22 eyes) from 10 to 14 years of age were photographed and analysed.
Results
The mean cell density in the oldest age group, over 100 years of age (average 102 years), was very good 2365 cells/mm2. The mean cell density in the transplanted corneas, the endothelial cells of which were over 100 years old (mean 106 years), was 923 cells/mm2 (range 585–1800 cells/mm2).
Conclusion
Corneal endothelial cells may remain viable and capable to perform their function over 100 years. Donor corneas up to 70–75 years of age can be approved for transplantation, provided that the endothelial cells have been thoroughly evaluated with vital staining before the operation.
Introduction
Human corneal endothelium is composed of a monolayer of hexagonal cells whose main function is to keep cornea clear. They are derived from neural crest and are arrested in the postmitotic state. They do not divide after birth (Joyce et al. 1996). This makes the ageing process of corneal endothelial cells different from that of many other cells in our body where the cells divide constantly replacing the dying cells.
Newborn infants have tightly packed corneal endothelium, and in 2-month-old infants, cell densities as high as 5624 cells/mm2 have been reported (Speedwell et al. 1988). Because of the normal growth of the eye and increasing corneal size, the endothelial cell density decreases rapidly during early childhood (Murphy et al. 1984; Nucci et al. 1990). Thereafter, the total number of endothelial cells decreases more slowly, approximately 0.6%/year (Bourne & Kaufman 1976; Laing et al. 1976; Williams et al. 1992; Bourne et al. 1997). Despite of this age-associated decline, the average reserve is usually high enough for maintaining critical barrier and pump function for the whole lifetime, provided that no disease such as endothelial dystrophy or glaucoma develops (Setälä 1979; Senoo et al. 2000).
When endothelial cells get damaged, the structural integrity is maintained by spreading of neighbouring cells to cover the area of dead cells (Kaufman et al. 1965; Capella 1971). Until now, it is not clear how many viable endothelial cells are needed to keep the cornea or the corneal graft clear. Previously, we have found clear grafts with cell densities of only 500 cells/mm2 (Ruusuvaara & Setälä 1988a,b). Ruusuvaara (1979, 1980); Vasara et al. 1999) showed in his studies great disparities between the endothelial cell densities of the graft and the recipient cornea. After the transplantation, endothelial cell density decreased more rapidly in the graft than in the recipient cornea. This difference suggests strongly that there is little, if any cell migration between graft and recipient (Ruusuvaara 1980).
The main purpose of this study was to evaluate endothelial cell density and morphology of healthy corneas of subjects with high age (up to 100 years) and compare the results with those of transplanted corneal grafts with 100-year-old endothelial cells (donor age + postoperative follow-up time).
Subjects and Methods
The study was carried out at the Helsinki University Eye Hospital. The study followed the tenets of the Declaration of Helsinki and was approved by the Helsinki University Eye Hospital Ethics Committee. All subjects, in case of children their legal guardian, gave their written informed consent. The inclusion criteria for those who had undergone corneal transplantation were as follows: physical age of the graft at least 100 years at the time of study examination, no eye trauma, no other intraocular surgery, no rejection of the graft, no other eye disease (e.g. glaucoma or uveitis), no corneal dystrophy, and grafts clear enough for photographing of endothelial cells. The inclusion criteria for the controls were as follows: no corneal dystrophy or eye diseases, no eye trauma, and no previous intraocular surgery and no contact lens wear (Setälä et al. 1998).
The elderly control population was recruited from the patients scheduled for cataract operation. The subjects aged from 48 to 52 years were recruited from the staff and the students amongst the medical students during their course in ophthalmology. The children from 10 to 14 years were recruited at their visit with their legal guardian in the neuro-ophthalmological clinic, and they had no eye diseases, but some neurological symptoms, for example visual field defects or diplopia. The hospital record on corneal transplantations was used to identify potential patients for the study. Six patients were found and five attended the follow-up visit. All keratoplasties were performed by the same surgeon (PR), and all grafts had been preserved in the M–K medium for <1 week before surgery.
Five individuals with seven corneal transplants were included in the study. The reason for transplantation was keratoconus (five eyes) and corneal opacity due to previous herpes simplex keratitis (two eyes), and no reactivation had been observed during the long postoperative period. At the time of transplantation, the age of the donor corneas was from 64 to 80 years. The follow-up time to the time of follow-up visit was from 24 to 39 years. Thus, at the control visit, the age of the corneal endothelial cells of the graft was from 100 to 114 years.
For controls, altogether 57 healthy individuals were examined: seven individuals (14 eyes) of 100–102 years of age, 14 individuals (28 eyes) of 90–98 years of age, 12 individuals (24 eyes) of 48–52 years of age, 12 individuals (24 eyes) of 19–24 years of age and 11 children (22 eyes) of 10–14 years of age.
Specular microscopy was performed on the central cornea, using Keeler-Konan contact specular microscope (SP 5500). The endothelial cells were videotaped and photographed. Three images from central cornea were taken, and at least 50 contiguous cells from each image were manually marked by the examiner. The built-in software program (the Konan cell analysis system KC-87 A) was used for analysis. The mean cell density (MCD), the smallest and largest cell sizes, the mean cell size, the coefficient of variation (CV) of the mean cell area and the percentage of hexagons were calculated.
For the analyses, mean of the two eyes of each control subjects was calculated for MCD, CV and percentage of hexagons. Linear regression analysis of the IBM spss Statistics v. 21 software (Armonk, NY, USA) package was used to analyse decrease in cell density/year amongst the control subjects. Normality of cell parameters of the grafts and the oldest age group was tested with the Shapiro–Wilk test and the Mann–Whitney U-test was used in the analysis.
Results
The results of the transplanted corneas are shown in Table 1. The grafts of seven eyes of five patients were analysed. The age of the endothelial cells varied from 100 to 115 years. Both eyes of the patients I and II, and right eye of the patient V had undergone penetrating keratoplasty because of keratoconus. Patients III and IV had been operated on because of cloudy cornea caused by herpes simplex infection. The transplant of the patient V had the highest endothelial cell density (1800 cells/mm2). The physiological age of these endothelial cells was a few months over 100 years (Fig. 1). Visual acuity of this eye was 0.9. The next highest cell density was 1081 cells/mm2 (patient I B) in an eye with 106-year-old endothelial cells. Visual acuity of this eye was 0.6 due to mild macular degeneration. The lowest cell density, 585 cells/mm2, was in the eye of patient II B. However, the graft was still clear, and visual acuity was 0.4 due to high astigmatism. The age of these cells was 101 years.
| Graft | Donor age (years) | Postop. follow-up time (years) | Total age of endothelial cells (years) | Transplant cells/mm2 | CV | Hexagonal |
|---|---|---|---|---|---|---|
| I A | 78 | 37 | 115 | 728 | 0.38 | 48 |
| I B | 71 | 35 | 106 | 1081 | 0.40 | 50 |
| II A | 80 | 34 | 114 | 643 | 0.42 | 48 |
| II B | 71 | 30 | 101 | 585 | 0.40 | 52 |
| III | 73 | 32 | 105 | 763 | 0.42 | 52 |
| IV | 64 | 39 | 103 | 859 | 0.42 | 54 |
| V | 76 | 24 | 100 | 1800 | 0.30 | 66 |
| Mean | 73 | 33 | 106 | 923 | 0.39 | 53 |
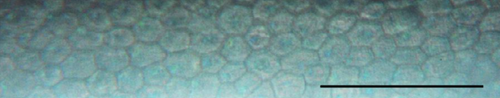
The results of the control eyes are shown in Table 2. The age group from 100 to 102 years included 14 eyes of seven subjects. The endothelial cell densities varied from 1180 to 3344 cells/mm2 with the mean of 2365 cells/mm2. Figure 2 displays a photograph of endothelial cells from a 100-year-old woman who had the best cell density (3344 cells/mm2) in this age group. Compared with the endothelial cells of the grafts, these control eyes had significantly higher cell density (p < 0.001, Mann–Whitney U-test), but no significant differences were detected in CV or percentage of hexagonal cells.
| Age | Patients | Cells/mm2 Mean (range) | CV Mean (range) | Hexagonal Mean (range) | |||
|---|---|---|---|---|---|---|---|
| Range | n | RE | LE | RE | LE | RE | LE |
| 100–102 | 7 | 2366 (1265–2620) | 2365 (1180–3344) | 0.36 (0.28–0.51) | 0.34 (0.26–0.44) | 55 (50–63) | 56 (48–63) |
| 90–98 | 14 | 2201 (1426–2816) | 2163 (1364–2622) | 0.37 (0.33–0.42) | 0.36 (0.32–0.42) | 55 (50–60) | 56 (50–68) |
| 48–52 | 12 | 2876 (2012–3703) | 2947 (2066–4048) | 0.29 (0.20–0.38) | 0.29 (0.22–0.40) | 68 (55–70) | 62 (58–72) |
| 19–24 | 12 | 3220 (2409–3802) | 3269 (2597–3649) | 0.26 (0.20–0.34) | 0.27 (0.20–0.32) | 63 (56–74) | 64 (54–78) |
| 10–14 | 11 | 3632 (3039–4149) | 3603 (3076–4484) | 0.16 (0.13–0.20) | 0.16 (0.10–0.19) | 93 (86–98) | 92 (80–100) |

In the control eyes, the endothelial cell density decreased, CV increased, and percentage of hexagons decreased with age (Fig. 3A–C). According to linear regression analysis, the decrease in cell density was 0.4%/year [cell density = 3681 − (15.2 × Age)]. Age explained most of the change with time (R2 = 0.60).
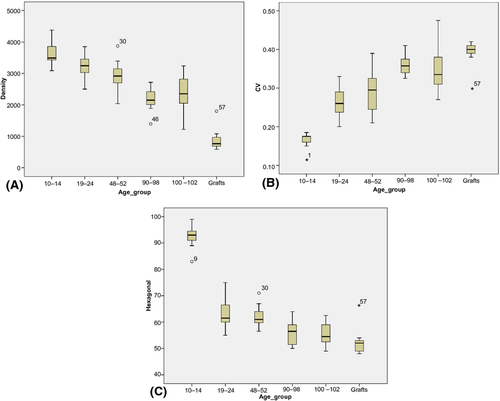
Between the age groups of 10–14 and 19–24 years, cell density did not change much, but great change was noted in CV and percentage of hexagons.
Discussion
Our study showed that 100-year-old endothelial cells, both in transplanted corneas and in healthy unoperated eyes, are able to maintain corneal clearness even if the cell number is fairly low. Nowadays, it is not easy to find 100-year-old people who have healthy, intact eyes and have not undergone cataract operation. In our study, one individual from the oldest control group had a very good cell density in both eyes (3144/3344 cells/mm2). Also the MCD in this age group was very good (2365 cells/mm2). Endothelial cells do not divide. Under favourable conditions, the corneal endothelium longevity may be as long as 150–200 years before ageing-related cell loss reduces cell density to a critical level (Murphy et al. 1984).
It is well known that human central corneal endothelial cell density decreases with age, and polymegethism and pleomorphism increase gradually (Laing et al. 1976; Williams et al. 1992; Bourne et al. 1997; Moller-Pedersen 1997; Yunliang et al. 2007). Although our study was cross-sectional and the number of patients was rather low, we wanted to get an estimate for the decrease of cell density in the control group, it was 0.4%, which is in accordance with other studies (Bourne & Kaufman 1976; Laing et al. 1976; Williams et al. 1992; Bourne et al. 1997). Hashemian et al. (2006) reported that the endothelial cell density and age correlated up to 60 years of age, after which no correlation was observed.
Great concern has been connected with high age of the donor. According to the Cornea Donor Study Investigator Group et al. (2008), grafts from subjects up to the age of 75 years are suitable for transplantation (Lass et al. 2010). Also Probst et al. (1997) showed that 67% of the corneas of the phakic eyes in the age group of 86–90 years and 50% in the age group of 91–95 years were suitable for transplantation. Our study agrees that donors from individuals up to 80 years of age may be suitable for transplantation. Recently, Visby et al. (2014) also studied grafted corneas with a tissue age of more than 100 years and showed that they can still function well. In their study group, the lowest cell density was 700 cells/mm2, and we had one patient with clear graft and cell density of 585 cells/mm2. Visby et al. observed the highest cell density in one graft being 3700 cells/mm2, and our highest was 1800 cells/mm2. The initial cell density of the donor has possibly no significant influence on the course of endothelial cell loss after transplantation (Bertelmann et al. 2006). The endothelial cells suffer from manipulation during the operation, and the remaining healthy cells have to move to cover the damaged areas. Postoperatively, the cell density decreases rapidly, but after the first 2 years, the cell loss slows down (Ruusuvaara 1979; Matsuda & Bourne 1985). Similarly, Abbott et al. (1983) did not find any significant change in the cell counts of the grafts photographed 10–15 years and again 20–35 years after transplantation. It may be assumed that decline in the cell count stabilizes 1–2 years after transplantation to a level that parallels the loss observed with increasing age. (Bourne 1980; Ruusuvaara 1980; Schultz et al. 1985; Ruusuvaara & Setälä 1988a,b).
Evaluation of endothelial cells before transplantation is of utmost importance. A skilful operator is mandatory. In our patients, the primary trephination of the cornea (12–13 mm) was performed with an electric rotor trephine (designed by Draeger) from the epithelial side. The final trephination of the transplant (7–8 mm) was performed with the Polack punch from the endothelial side with the protective viscoelastic fluid (PR). One must also remember careful control of postoperative intraocular pressure. Long-standing (>3 days) high intraocular pressure in acute glaucoma has been shown to decrease endothelial cell density by 50% (Setälä 1979). Endothelial cells of a graft may be even more susceptible to high pressures.
However, both our study and that of Visby et al. (2014) show positive results; very old endothelial cells can still function well and keep cornea clear.