Pharmacomechanical thrombectomy of iliofemoral deep vein thrombosis is associated with a low incidence of post-thrombotic syndrome and perioperative complications
Abstract
Background
Iliofemoral deep venous thrombosis (IFDVT) is associated with an incidence of post-thrombotic syndrome (PTS) of up to 50%. PTS is associated with high morbidity, impaired quality of life and a significant economic burden. The aim of the current study was to assess the impact of a single session pharmacomechanical thrombectomy (PMT), dedicated venous stents and a risk mitigation protocol on the rate of PTS.
Methods
Between 2015 and 2022, patients presenting with acute or subacute IFDVT treated with the same protocol of single session PMT, dedicated venous stents, and risk-mitigation measures were included. Procedural success rate, complications, stent patency and incidence of PTS were determined.
Results
Of 60 patients (58 ± 19 years; 65% male), the procedural success rate was 93%, with 7% of patients experiencing complications but no long-term sequelae or mortality. Most (n = 52; 87%) patients were stented, including 46% across the inguinal ligament. At 3 months post-procedure, primary, assisted primary and secondary stent patency rates were 89%, 93% and 98%, respectively, with no loss of patency or re-interventions after that. At latest follow-up of a median 48 months (n = 32), stent patency rate was 97%, with only three patients (9%) experiencing symptoms of PTS.
Conclusion
Single session PMT, dedicated venous stents and a risk-mitigation protocol results in high success rate, excellent long-term stent patency and low incidence of PTS without compromising safety. These results support early intervention for iliofemoral DVT.
Introduction
Venous thromboembolism (VTE) comprises deep vein thrombosis (DVT) and pulmonary embolism (PE) and is the third most common vascular disease globally after myocardial infarction and stroke.1 DVTs are the more common manifestation of VTE, and iliofemoral DVTs (IFDVT) account for ~25% of all DVTs.2 These have a worse prognosis than other DVTs3 and around 20–50% of those with an iliofemoral DVT develop post-thrombotic syndrome (PTS).4, 5 PTS is characterized by leg pain and heaviness, venous claudication, oedema, skin changes and in some patients, venous ulcers.2 It is associated with a high morbidity rate and impaired quality of life,6 and represents a significant economic burden.7, 8
PTS is more common after an iliofemoral than an infrainguinal DVT for several reasons. First, the recurrence rates of IFDVT are 2.6 times higher than in other locations.9 Second, the iliofemoral segment has a very low rate, about 20%, of recanalization.10 This causes pelvic venous obstruction, which is associated with more venous claudication and ulceration, and more rapid disease progression.11 Third, in IFDVT, deep valve dysfunction increases advanced disease development.12 Such post thrombotic changes result in incompetence and reduced vein diameter and compliance in the infrainguinal segment. This compromises the chances of success with later interventions since these “inflow vessels” become unsuitable for future stenting procedures.
Early intervention in IFDVT may prevent the inflow vessels from becoming damaged due to PTS and accordingly, assist with maintenance of long-term patency. Indeed, the patency rates of stents used to treat underlying stenosis in acute IFDVTs are high, comparable to those for non-thrombotic lesions and better than those for post-thrombotic obstruction.13 However, the rationale behind early thrombus removal was put into question after the results of the ATTRACT trial (Acute Venous Thrombosis: Thrombus Removal with Adjunctive Catheter Directed Thrombolysis) were published,14 which suggested that early intervention of acute DVT did not reduce PTS.15, 16 Reasons behind the discordance between the ATTRACT trial conclusions and others' experience have been extensively discussed,10-12 and include: (i) the use of outdated technology; (ii) heterogeneous techniques; (iii) inclusion of both femoro-popliteal and iliofemoral DVTs; (iv) a very low stenting rate; and (v) a lack of follow-up imaging to verify the open vein hypothesis. Catheter directed thrombolysis (CDT) in the treatment of IFDVT is expensive as it requires more than one interventional session and a prolonged hospital stay to yield successful outcomes.
The aims of this study were to determine: the incidence of PTS and procedural and stent-related complications: long-term stent patency rates; and inflow vessel patency and competency in a group of patients with IFDVT treated with a low dose single session PMT with AngioJet™ and dedicated venous stents. The outcome measures were procedural success and safety, long-term stent patency rates and inflow vessel patency and competency, and PTS incidence.
Materials and methods
Study design and patients
This was a retrospective analysis of prospectively collected data of patients who presented to The Wollongong Hospital in New South Wales, Australia with symptomatic IFDVT between 2015 and 2022. Ethical approval for this study was granted by the University of Wollongong Human Research Ethics Committee (approval number: 2020/290), which included an approved waiver of consent. The inclusion criteria were patients who had a diagnosis of IFDVT with severe symptoms for less than 6 weeks (i.e., acute or subacute) and unsuccessful trial of conservative management (at least 24 h of anticoagulation, leg elevation and compression), with no contra-indication to lytic agents, and who had undergone treatment with a protocol of PMT with the AngioJet™ (Boston Scientific) followed by balloon angioplasty and/or stenting during a single treatment session. The exclusion criteria included mild symptoms or symptoms present for greater than 6 weeks, a favourable response to conservative management with the ability to mobilize comfortably, renal failure and high risk of bleeding.
Protocol for the treatment of acute IFDVT
Under general anaesthesia and intravenous heparin infusion, all patients were supine allowing for multiple access points. Intravenous fluids were maintained throughout, and an indwelling urine catheter (IDC) was inserted to monitor urine output.
Percutaneous venous access was achieved using duplex guidance via a patent vessel distal to the thrombosis, preferably a calf vein, usually the posterior tibial vein, but internal jugular, small saphenous, popliteal or femoral vein access were also be used.
Thrombolysis with the AngioJet™ in Power Pulse Spray mode and 30 min of “maceration time” preceded thrombectomy. Alteplase was diluted 10 mg in 100 mL of saline. Thrombectomy was kept under 240 s in all cases, with close attention paid to the catheter tubing to minimize thrombectomy in segments with flowing blood.
Balloon angioplasty followed thrombectomy, as a clot maceration tool and to treat underlying stenosis. Stenosis of >50% was considered significant. Dedicated venous stents (sinus-Venous™ from Optimed) were used to treat underlying severe stenosis in the common femoral vein (CFV), external iliac vein (EIV), common iliac vein (CIV) and/or inferior vena cava (IVC). Duplex ultrasound was used for stent patency assessment during follow-up.
We followed a strict risk-mitigation protocol to minimize bleeding, access site complications, PE, acute kidney injury and re-thrombosis (Table 1).
| Risk category | Intra-operative | Post-operative |
|---|---|---|
| Bleeding |
|
|
| Access site complications |
|
|
| Pulmonary Embolism |
|
|
| Acute Kidney Injury |
|
|
| Re-thrombosis |
|
|
Post-procedure care
Access sheaths were removed in the operating theatre and manual pressure was applied, followed by compression stockings/bandages and sequential compression devices. Patients were sent to the ward, not the Intensive Care Unit (ICU) and encouraged to mobilize as soon as possible.
Patient follow-up
A duplex ultrasound was arranged prior to discharge and at follow-up visits at 1, 3, 6 and 12 months and yearly afterwards. Villalta scoring17 was used at each visit.
Data collection and statistical analysis
Data collected included patient characteristics (age, sex and comorbidities, renal function and presence of PE), DVT characteristics (side affected and veins involved), procedural details (lytic dose, thrombectomy time, stenting rate), safety outcomes, procedural success (defined as <30% residual thrombosis burden, <50% residual stenosis and restoration of flow) and stent patency: primary patency (ongoing vessel patency without re-intervention), assisted primary patency (patency requiring intervention but without occlusion) and secondary patency (patency after intervention of an occluded vessel).
Results
Patient characteristics
There was a total of 60 patients (65% male) included in analyses, with mean age 58.2 ± 18.7 years, not significantly different between males and females (P = 0.310). Pre-operative plasma creatinine was 75.1 mg/dL ± 22.6 (range: 27–161). Just over one-half (n = 31) of the patients had a normal eGFR >90 mL/min, and the mean for the remaining 29 with a low eGFR was 69.0 ± 14.6 mL/min (range 37–89). On admission, 25 patients (43%) had a concurrent PE; this was significantly more prevalent among males than females (56% vs. 20%; χ2 = 7.111; P = 0.008). In terms of comorbidities: 42% had hypertension, 37% had thrombophilia, 20% had malignancy, 8% had diabetes, 5% had chronic renal failure and 3% had ischaemic heart disease. Almost one-third (30%) had a history of a venous thromboembolism.
DVT characteristics
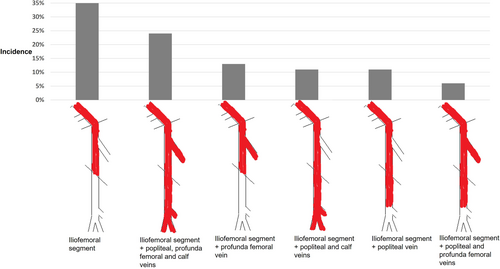
The majority (n = 39; 65%) of DVTs were on the left side, while 10 (17%) were bilateral and 11 (18%) were right-sided. Among those with a bilateral DVT, seven had bilateral symptoms, two had symptoms on the left only and two on the right side only. The IVC had thrombus in 13 cases: of these, eight had bilateral DVT and five had only left-sided DVT. Most patients (n = 40; 67%) had extension of the thrombus beyond the femoral vein; the prevalence of which veins were involved is shown in Figure 1.
After thrombus removal, 57 (95%) of patients had an underlying stenosis of >75% of the iliofemoral segment, and 42 (70%) had underlying stenosis of >75% of the femoro-popliteal segment. A significantly higher proportion of males than females (83% vs. 17%) had underlying stenosis of the femoro-popliteal segment (χ2 = 13.636, P < 0.001).
Procedural details and success, and safety outcomes
The mean dose of Alteplase used was 6.8 ± 2.7 mg with a mean thrombectomy time of 156 ± 79 s. The procedural success rate was 93% (56/60). Of the four cases not considered successful, one procedure was a failure with immediate re-occlusion of the stents due to poor inflow vessels. The other three patients could not receive a stent to fix the underlying stenosis: one due to IVC atresia; another had a complex iliac artery branch device and there were concerns about ischaemia; the third had metal hardware from a spinal operation that prevented passing the balloon. There was a total of 6 (9%) procedure-related complications affecting 5 (8%) patients. This included minor bleeding (n = 1), major bleeding (n = 1), acute kidney injury (n = 3), access site complications (n = 1) and pulmonary embolism (n = 1). There was no mortality and no case of intracranial haemorrhage, limb loss or cardiac events. There was no mortality and no long-term sequelae from any of the complications.
Stenting rates and location
Of the 56 patients for whom the procedure was successful, four received balloon angioplasty only, and 52 were stented. The majority (85%) of stents were deployed into the CIV and EIV; more than half of these extended into the IVC and/or CFV, with 46% (24/52) crossing the inguinal ligament (Table 2). Apart from the case of immediate failure described above, the remaining 51 of the 52 stents (98%) were patent at the end of the procedure. There were no stent-related complications (migration, mal-deployments, fractures or stent compressions) at any stage.
| Vessels stented | Number |
|---|---|
| CIV, EIV | 20 (38%) |
| CIV, EIV + CFV† | 16 (31%) |
| IVC, CIV, EIV | 6 (11.5%) |
| EIV + CFV† | 6 (11.5%) |
| IVC, CIV, EIV + CFV† | 2 (4%) |
| EIV | 2 (4%) |
- †Indicates where the stent has crossed the inguinal ligament. CFV, common femoral vein; CIV, common iliac vein; EIV, external iliac vein; IVC, inferior vena cava.
Long-term stent patency
A flowchart of patients with loss to follow-up is included in Figure 2. At 1-month post-procedure, the primary patency was 49/52 stents (94%), and secondary stent patency was 51/52 stents (98%). There was one immediate failure, and two occlusions post procedure: one re-thrombosed in the same admission due to poor inflow and required balloon angioplasty of the PFV, the other occluded after 4 weeks and needed an extension of the stents due to a missed lesion. Within the first 3 months post-procedure, two other patients, with patent stents, required re-intervention: one needed a stent extension due to a missed lesion found on duplex, and the other had in-stent thrombus due to sub-therapeutic anticoagulation. All re-interventions were successful. There were data for 46 patients at 3-months post-procedure, with a stent patency rate of 98% (45 of 46 stents); this included 41 (89%) primary patency, 43 (93%) assisted primary patency and 45(98%) secondary patency.
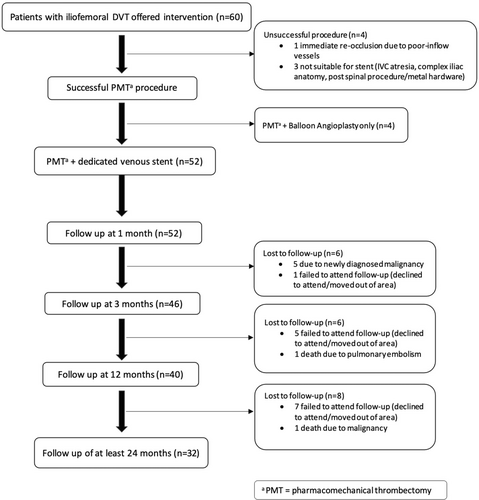
There was no loss of patency after the first 3 months. At 12 months, there were data for 40 patients, and at the latest follow-up (median 48 months; range: 24–72 months; interquartile range: 48 months), there were data for 32 patients. There were no instances of late stent occlusion, with a stent patency rate of 97% at each of 12 months (39/40) and at latest follow-up (31/32).
Incidence of PTS
At the latest follow-up of median 48 months (n = 32), 29 had a Villalta score of <5 (normal), two patients had a score of 5 (mild PTS) and one had a score of 16 (severe PTS), giving a total of three (9%) with PTS. The one patient with severe PTS had an unsuccessful procedure, which resulted in pelvic and infra-inguinal obstruction, as well as deep vein incompetence. Of the other two patients with mild PTS, both had patent stents but evidence of deep venous incompetence on the femoro-popliteal segments. All three reported swelling and claudication, and two had skin changes. Another three patients (9%) had residual oedema, but they still scored <5 on Villalta scoring system.
Patency and competency of inflow vessels and associations with PTS
At the latest follow-up of median 48 months (n = 32), the femoral and popliteal veins were patent and competent in 70% and 58%, respectively, while there was residual thrombus of >30% in 3% and 6%, respectively.
When patients were classified as being asymptomatic (n = 26) versus any symptoms (e.g., pain, oedema) and/or PTS as per Villalta score (n = 6) at the latest follow-up of the median of 48 months, a significantly higher proportion of those who did not have symptoms had a patent and competent popliteal vein (Table 3). Almost double the proportion of patients without symptoms had a patent and competent popliteal vein compared with those who had any PTS related symptoms.
| No PTS (n = 26) | PTS symptoms (n = 6) | Comparison† | |
|---|---|---|---|
| Femoral vein | |||
| Patent and competent | 72% | 60% | χ2 = 5.186 P = 0.075 |
| Patent and incompetent | 28% | 20% | |
| Residual thrombus | 0 | 20% | |
| Profunda femoral vein | |||
| Patent and competent | 83% | 0 | χ2 = 2.917 P = 0.088 |
| Patent and incompetent | 17% | 100% | |
| Residual thrombus | 0 | 0 | |
| Popliteal vein | |||
| Patent and competent | 64% | 33.3% | χ2 = 9.127 P = 0.010 |
| Patent and incompetent | 36% | 33.3% | |
| Residual thrombus | 0% | 33.3% |
- †Comparisons are chi-square tests. PTS, post-thrombotic syndrome.
Discussion
This study showed that a structured approach with a protocol of single session, low dose pharmacomechanical thrombectomy, with a risk mitigation protocol and dedicated venous stents was safe and effective in the management of acute and subacute IFDVT. Considering that 95% of patients in this series had severe underlying stenosis of the iliofemoral segment, and 65% of patients had extension of the DVT beyond the femoral vein, affecting the inflow vessels, this patient group was a challenging one to treat. Despite this, and not withstanding that 46% required stenting across the inguinal ligament, we were able to achieve long-term stent patency of 97% at 48 months with a 7% complication rate. Combined with a femoral and popliteal vein patency and competency of 70% and 58% respectively, our protocol achieved a low PTS rate of only 9%. The acceptable morbidity and absence of procedure-related mortality mirrored the results of others.18-21
Go et al. reported a two-year patency of 72.2% and 74.7% for the single and multiple sessions procedures, respectively, with an overall post-thrombotic syndrome rate of 28.4% at 5 years and no mortality.18 Ascher et al. described a single session technique with a 100% success rate, no re-intervention within 12 months, one access site complication and no mortality.19 Jiang et al. also reported a technical success rate of 100%, a 24-month primary patency rate of 91.1%, PTS rate of 2.17% and only one patient developed mild PTS, and no major bleeding or 30-day mortality.20
The main deterrent to offering invasive treatment, as with any surgical intervention, is the associated risks. For AngioJet™, the main risks associated with intervention can be divided into four categories: bleeding, access site complications, PE and acute kidney injury. Low dose alteplase (6.8 ± 2.7 mg) can minimize bleeding risk because our single session has allowed us to use a very low dose of comparable to others.19-22 Access site complications can be minimized by using duplex guidance. To reduce risk of PE, it is best to minimize catheter exchange, infuse the thrombus with lytic first and move in a cranio-caudal direction rather than ‘pushing’ through a large column of thrombus. To prevent acute kidney injury, we use aggressive peri-operative hydration with IVF, close monitoring of urinary output, and a time limit of 240 s for the thrombectomy.
Finally, this study supports the open vein hypothesis, with only one severe PTS case that was a procedural failure resulting in pelvic obstruction and deep vein incompetence. There were more than 30 patients reaching more than 24 months follow-up and only three patients who scored >5 on Villalta score at their latest consultation (median 48 months).
The limitations of this study are the small numbers and the retrospective nature of the analysis. Its strengths are the prospective data entry and strict adherence to a specific protocol.
Conclusion
A single session low dose PMT with AngioJet™ combined with dedicated venous stents and a risk mitigation protocol is associated with low peri-operative complications and low incidence of PTS.
Acknowledgements
The authors thank Monique Vorster for her assistance with data collection. Open access publishing facilitated by University of Wollongong, as part of the Wiley - University of Wollongong agreement via the Council of Australian University Librarians.
Author contributions
Theresa A. Larkin: Formal analysis; investigation; methodology; writing – original draft; writing – review and editing. Raeed Deen: Writing – review and editing. Taraneh Amirnezami: Formal analysis; investigation; methodology; writing – review and editing. Alisa Shvartsbart: Methodology; writing – original draft. Laurencia Villalba: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; writing – original draft; writing – review and editing.
Conflicts of interest
A/Prof Villalba is a consultant for Boston Scientific (AngioJet) and Phillips (IVUS), however, has not received any funding related to this manuscript. The authors declare that there is no conflict of interest.
Open Research
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.