Full robotic cholecystectomy: first worldwide experiences with HUGO RAS surgical platform
Abstract
Background
The Hugo RAS™ system (Medtronic, Minneapolis, MN, USA), approved for gynaecological and urological procedures, has been recently certified for the use in few general surgeries. Only bariatric and colorectal procedures have been described so far.
Methods
Here, we report the first worldwide experience with three cases of full-robotic cholecystectomies with the Hugo RAS™ system.
Results
A description of the operative room setup, of the docking angles and details of the procedures is reported. Docking time was 12, 10, and 6 min, respectively. The total operative time was 105 min in the first case, 100 min in the second and 88 in the third case. Intra- and post-operative courses were uneventful.
Conclusions
With this pre-defined set up, the innovative conformation of Hugo RAS™ system can safely allow performing full robotic cholecystectomy avoiding the need for additional ports.
Introduction
Since the first robotic cholecystectomy performed in 1997 in Belgium, many technological advancements have been achieved.1, 2
Unfortunately, the not-negligible costs still represent the Achille's heel of the current used technology.3
The need of cheapest and less cumbersome devices, together with the improvement of technology paved the way to the development of other robotic systems.
In this scenario, the Hugo RAS™ system (Medtronic, Minneapolis, MN, USA) has been recently introduced. This system shares the same core technology of the Intuitive Surgical but four different arms settled on four separated carts represent the main difference.
Hugo RAS™ allows a wide range of adaptability to different surgical procedures and surgical fields and, at the same time, has the potential advantage of being less cumbersome in the operating room.
To date, this Hugo RAS™ system technology has been applied mainly in gynaecology4 and urology,5 while experience of its use in general surgery is in the very early beginning.6-8
To the best of our knowledge, no data have been published till now on robotic cholecystectomy performed with the Hugo robotic system.
In this work, we report the first worldwide experience of three consecutive cases of full-robotic cholecystectomies with the Hugo RAS™ system. The position of the robotic arms, as well as the trocars sites and the docking angles have been developed and verified by our team in order to guarantee reproducibility and safety.
Methods
Surgical team
The surgical team, formed by an operating surgeon at the console, a bed assistant surgeon and a scrub nurse, after having completed the specific training for the Hugo RAS™ system and having achieved the user licence certification, performed three consecutives full robotic cholecystectomies with a novel set-up never used on humans before. The setting was previously tested by the same team on a porcine animal model.
Patient's characteristics
Patient 1
34-year-old female affected by asymptomatic cholelithiasis. BMI: 26. ASA II.
No previous abdominal surgery.
No pharmacological therapy.
Patient 2
69-year-old female affected by symptomatic cholelithiasis. BMI: 26. ASA II.
No previous abdominal surgery.
Chronic assumption of cardioaspirin for carotid stenosis.
Patient 3
74-year-old female affected by asymptomatic cholelithiasis. BMI: 27. ASA III.
No previous abdominal surgery.
Chronic assumption of cardioaspirin for chronic ischemic heart disease.
Robotic system, set-up and positioning of trocars
The Hugo RAS™ system, consisting of the central tower with the surgical console and four robotic arms, and the layout of the operating room are shown in Figure 1.
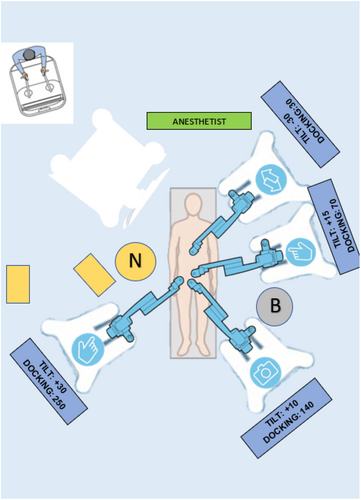
The patients were in the American position on the operating table. The first 11 mm periumbilical robotic trocar was positioned using the open technique. Pneumoperitoneum was induced at CO2 pressure values of 12 mmHg and a laparoscopy was performed using the camera of the robotic system without the need for its docking. Once the entire abdominal cavity has been explored and the absence of further pathological findings confirmed, the table was tilted in 15° anti-Trendelenburg position.
Three 8 mm robotic trocars were positioned after having identified the main body prominences (costal arches, antero-superior iliac spines) and considering the 11 mm periumbilical trocar as the central landmark.
- Epigastrium, below the xiphoid process, to the right of the falciform ligament about 13 cm from the periumbilical trocar in the first case and 15 cm in the second one. During the surgeries, this port hosted a double fenestrated forceps, used as liver retractor, to lift the fundus of the gallbladder and in order to medialize the elements of the hepatic pedicle according to the different steps of the procedures.
- Right hypochondrium, about 13 cm from the umbilical trocar, meant to host a forceps cadiere to be used as.
- Mesogastrium, 9 cm from the optical trocar and about 5 cm cranially for the use of monopolar scissors.
The sites of the trocars and the arms position are illustrated in Figure 2.

Once positioned the trocars, we set the lowest trocar (the one in the right hypochondrium in our cases) at the same level of the 70% of the scale present on each robotic cart.
The pre-defined Tilt and Docking angles did avoid any conflicts of the robotic arms with each other and with the patient (Table 1).
| Tilt angle | Docking angle | Instrument | |
|---|---|---|---|
| ARM 1 | +30° | 250° | Double fenestrated forceps |
| ARM 2 | +10° | 140° | Monopolar scissor |
| ARM 3 | +15° | 70° | Camera |
| ARM 4 | −30° | 30° | Cadiere forceps |
Results
Compared with the programmed and studied setup on the animal model, no modifications of TILT and Docking angles were needed. There were no serious system errors (e.g., red) during docking. Docking time was 12 min for the first case, 10 min for the second procedure and 6 min for the third one.
The time for the preparation of the operatory room (from patient entry until the start of console time) amounted to 67 min for the first patient and 70 min for the second one. Fifty-five minutes were needed for the preparation in the third case.
The console operative time for the first procedure was 38 min. Sixty minutes were needed at the console for the second one and 54 in the third one.
The total operative time (from skin incision to skin closure) was 105 min in the first case, 100 min in the second and 88 in the third procedure.
During the operation, only few low intensity (e.g., yellow) errors occurred without any influence on the operative time.
In all the cases, the Calot triangle was approached first on the posterior peritoneal layer with the double fenestrated forceps used to medialize the hepatic pedicle elements while the cadiere lifted the infundibulum up and medially.
Then the anterior peritoneal layer was incised using the double fenestrated forceps as liver retractor and the cadiere moving the infundibulum to obtain the critical view of safety.
Once the artery and cystic duct were identified, the robotic scissors were removed and through the same trocar, the bed assistant surgeon applied 9.2 mm titanium clips avoiding the need for further service access.
Artery and cystic duct were dissected with robotic scissors repositioned and cholecystectomy completed.
The bed assistant inserted in the abdomen a catch through the optical trocar, taking care to keep its closure thread outside the abdominal cavity; the console surgeon retrieved the catch and put the gallbladder inside it. Extraction of the specimen was performed from the periumbilical access.
After re-induction of the pneumoperitoneum, haemostasis was checked and trocars removed.
Postoperative outcomes were acceptable. All the three patients were discharged, as usual, on the second post-operative day.
The check of the wounds at discharge did not reveal any critical issues; patient 2 presented a sub-centimetric hematoma at the epigastric trocar.
Data regarding patient characteristics, intra- and peri-operative times and post-operative course are summarized in Table 2.
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
| Age (years) | 34 | 69 | 74 |
| Sex | F | F | F |
| BMI | 26 | 26 | 27 |
| ASA score | II | II | III |
| Docking time (min) | 12 | 10 | 6 |
| Pre-operative time (min) | 67 | 70 | 55 |
| Console time (min) | 38 | 60 | 54 |
| Total operative time (min) | 105 | 100 | 88 |
| Conversion | NO | NO | NO |
| Post-operative complication | NO | NO | NO |
| Length of stay (days) | 2 | 2 | 2 |
Discussion
To date few are the reported experiences with the Hugo RAS™ in general surgery.
The first experience was published in 2022 by Balachandran who reported the first robotic inguinal hernia repair.6
In 2023, Raffaelli reported a first series of five cases of lateral trans-abdominal adrenalectomy with this new robotic platform.7
More recently, Bianchi published a technical note reporting the first series of Colorectal Surgeries with the HUGO RAS™ system.8
Here, to the best of our knowledge, we report the first experience and technique of full robotic cholecystectomies with the Hugo RAS™ system without the need of extra ports dedicated to the bed assistant.
The positioning of the trocars differs in part from that previously used for other robotic platforms.9
In our experience, the mean time needed for the assessment of the operating room with the Hugo RAS™ was longer than that reported for robotic cholecystectomies with the Da Vinci system (64 vs. 53 min).10
It is our opinion that this difference is related to the lack of experience of the team with this robotic platform and by the need of positioning four different carts.
However, the presence of four separate robotic arms may guarantee greater adaptability of the system to each single patient and procedure.
In our experience, the operating room setting proved to be safe and effective. The tilt and docking angles allowed the surgery to be completed without any conflict between the arms.
Even if our approach proved to be effective in all the cases without needing any modifications, modifications of ±5° degrees, if needed, can be acceptable.
Our total operative time was also slightly higher when compared with those reported by Huang for Intuitive Surgical,10 but in agreement with Bianchi, it is predictable that practice will improve it.8
Console operating times are comparable with what already published by Chang et al. for other robots.9
Regarding the time difference between the cases, it can be easily explained by the fact that the second patient presented multiple gallbladder-colic and duodenal-gallbladder adhesions which required lysis.
Intra-operative and post-operative outcomes, albeit of only three cases performed, were comparable with previous robotic experiences.11, 12
In addition, we would underline that, due to the absence of the availability of a monopolar hook, the operation was safely performed using the monopolar scissors. Nonetheless, the wide range of the articulation of this instrument allowed its use used in the same way of a monopolar hook.
However, it is our opinion that further implementations in the instrumentation availability (energy devices, staplers and integrated fluorescence imaging systems, hook) are necessary for future and larger applications of this new system in other types and more complex surgeries.
Conclusion
The Hugo RAS™ system proved to be helpful in safely performing three robotic cholecystectomies surgeries. The innovative conformation of this robotic system and the precise pre-defined set up allowed the use of all four robotic arms without the need for additional service ports.
Acknowledgement
A special thanks to Yussef Rashed Qaddourah, the Hugo RAS™ specialist for his help and technical assistance.
Author contributions
Damiano Caputo: Conceptualization; supervision; validation; writing – review and editing. Tommaso Farolfi: Conceptualization; data curation; formal analysis; methodology; validation; writing – original draft. Chiara Molina: Conceptualization; data curation; methodology. Roberto Coppola: Supervision; validation; writing – review and editing.
Conflicts of interest
None declared.