Giant colonic diverticulum: perioperative management with ERAS protocol
A 41-year-old woman presented to the emergency department with a 2-month history of an abdominal enlarging palpable mass, causing lower abdominal tenderness and increasing urinary frequency.
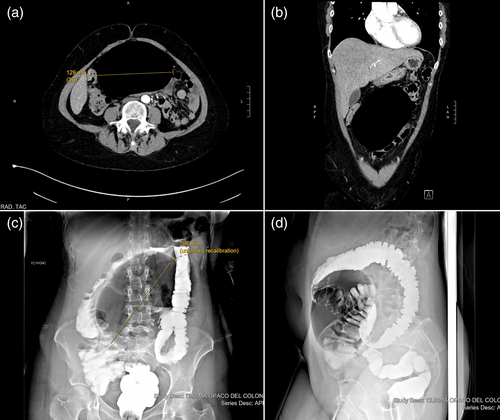
Abdominal contrast-enhanced CT revealed a smooth-walled, air-filled cavity with no septations measuring 196 × 87 × 129 mm, suggesting for a giant colonic diverticulum. A close relationship between the mass and the left annexa was also described (Fig. 1a, b). However water-soluble contrast enema still did not show a direct connection with the intestinal lumen (Fig. 1c, d).
The patient was scheduled for elective colorectal surgery and prepared with ERAS preoperative protocol.
Despite a laparoscopic exploration, laparotomic conversion was deemed necessary because of the size of the mass and the risk of intraperitoneal mass rupture (Fig. 2a, b). An ellipsoidal thin-walled, gas-filled mass arising from the antimesenteric border of the sigmoid colon was found, measuring 210 × 90 × 130 mm, with a volume of 1.25 L (Fig. 2c, d).
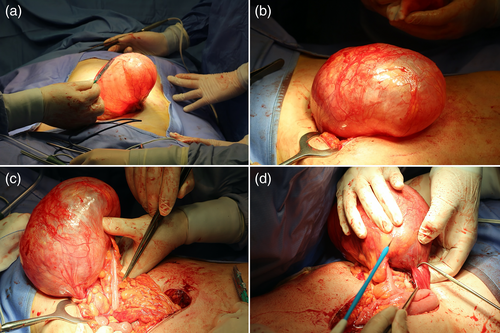
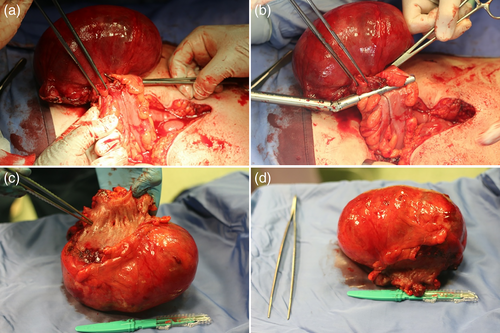
After lysis of inflammatory adhesions with the left annexa (Fig. 2d), a segmental sigmoid resection was performed, with side-to-side linear stapler anastomosis (FIg. 3a, b).
No drain tubes were placed. Nasogastric tube was removed before awakening.
The patient introduced oral clear fluids a few hours after surgery in POD0. Urinary catheter was removed in POD1. Effective analgesia and early mobilization, along with soft diet from the POD2, were essential for a quick bowel and physical recovery. Postoperative course was uneventful and the patient was discharged on POD4.
Pathology examination confirmed the diagnosis of a giant colonic diverticulum (GCD) with chronic inflammatory characteristics.
Post-discharge follow-up was implemented for 7 days with daily calls, up to the first ambulatory control. The patient had no complications, readmission, nor emergency department visits after 2 months from discharge.
GCD is defined as a colonic diverticulum greater than 4 cm and1 represents a rare presentation of colon diverticulosis, with less than 300 cases reported to date.2
Its etiopathogenesis is still a matter of debate. The main hypothesis refers to unidirectional ball-valve mechanism through a tiny communicating diverticular neck, which causes air entrapment and gradual enlargement of the diverticulum.
Clinical presentation includes abdominal pain, vomiting, constipation or diarrhoea, sensation of an abdominal mass and rarely rectal bleeding. Perforation and abscess formation are the most common complications, along with volvulus and obstruction.
Differential diagnosis includes also pneumosalpinx secondary to diverticulitis.
CT scan leads to correct diagnosis in nearly all cases. Barium enema might show a direct communication with the intestinal lumen, while endoscopic exploration is generally avoided because of the risk of perforation.
The recommended treatment for symptomatic uncomplicated GCD is surgical intervention with sigmoidectomy, with either laparoscopic or laparotomic approach.
The latest ERAS guidelines in colorectal surgery were applied.3 Compliance of ERAS preoperative items was 88%, with no perioperative morbidity.
Acknowledgement
Open Access Funding provided by Universit degli Studi di Sassari within the CRUI-CARE Agreement.
Author contributions
Simone Veneroni: Conceptualization; formal analysis; project administration; software; writing – review and editing. Silvia Porzani: Writing – original draft; writing – review and editing. Alessandro Fancellu: Supervision; visualization.




