Electrocardiograhic characteristics in patients with coronavirus infection: A single-center observational study
Abstract
Background
A global outbreak of coronavirus disease (COVID-19), caused by severe acute respiratory coronavirus 2 (SARS-CoV-2), has emerged since December 2019, in Wuhan, China. However, electrocardiograhic (ECG) manifestations of patients with COVID-19 have not been fully described. We aim to investigate ECG characteristics in COVID-19 patients and risk factors of intensive care unit (ICU) admission.
Methods
This retrospective observational study included the patients with COVID-19 at the Wuhan Asia General hospital between February 10, and 26, 2020. Demographic, clinical, and ECG characteristics were collected, and comparisons were made between the ICU and non-ICU admission groups. Logistic regression was used to identify risk factors of ICU admission.
Results
Among 135 included patients (median age: 64 years [interquartile range: 48–72]), ST-T abnormalities (40%) were the most common ECG feature, followed by arrhythmias (38%). Cardiovascular disease (CVD) was presented in 48% of the patients. Six (4.4%) died during hospitalization, and 23 (17.0%) were admitted to the ICU. Compared with non-ICU group, the ICU group showed higher heart rate (p = .019) and P-wave duration (p = .039) and was more frequently associated with CVD (p < .001), ST-T abnormalities (p = .007), arrhythmias (p = .003), QTc interval prolongation (p = .003), and pathological Q waves (p < .001). Twenty-seven patients were re-examined ECG during admission, and 17 of them presented new findings compared with their initial ECG presentations. ST-T abnormalities (p = .040) and history of CVD (p = .0047) were associated with increased risk of ICU hospitalization.
Conclusions
COVID-19 is frequently related to cardiovascular manifestations including ECG abnormalities and cardiovascular comorbidities. ST-T abnormalities and CVD at admission were associated with increased odds of ICU admission.
1 INTRODUCTION
The novel coronavirus 2019 (COVID-19) refers to infection caused by SARS-CoV2. As of May 30, more than 5 million individuals have been infected worldwide, which has become a global pandemic. Comprehensive investigation for the performance of cardiac abnormalities should be assessed in patients with COVID-19 because the novel coronavirus has been proven to have definite effects on the cardiovascular system (Madjid et al., 2020). However, there is no specific research on initial electrocardiogram (ECG) abnormalities, which were not uncommon especially in COVID-19 patients with underlying CVDs (Lakkireddy et al., 2020). Here, we retrospectively investigated the patients with COVID-19 in Wuhan Asia General hospital, described the features of ECG and identified the risk factors of the admission to intensive care unit (ICU).
2 METHODS
2.1 Patients
We retrospectively included the patients with confirmed COVID-19 admitted to Wuhan Asia General Hospital in Wuhan, China, from February 10, to 26, 2020. Definition of a case was based on the COVID-19 guidelines of seventh edition established by the Chinese Centers for Disease Control and Prevention (CDC), requiring computed tomographic evidence of pulmonary involvement accompanying RNA detection of the novel coronavirus in nasopharyngeal swab samples. The baseline characteristics were recorded on admission, including age, gender, symptoms, medication history, cardiovascular comorbidities, blood pressure, and heart rate. Admission to the ICU was arranged if vital signs and oxygen saturation were difficult to maintain, or the pulmonary infection progressed rapidly.
The study complied with the edicts of the Declaration of Helsinki (World Medical Association, 2013) and was approved by the Research Ethics Commission of Wuhan Asia General Hospital (WAGHMEC-KY-2020005). Given the retrospective review of this study, informed consent was waived.
2.2 ECG collections
18-lead electrocardiogram (ECG) and laboratory tests are the main observation indicators. The first ECG on admission was recorded with GE MAC 5000 electrocardiograph (General Electric Company). Patients with worsening conditions or heart-related symptoms during admission rechecked for ECG after assessment. The criteria of parameter measurement and ECG diagnosis are based on the recommendation of American Heart Association (AHA) et al (AHA/ACCF/HRS, 2007–2009). ST-T abnormalities were defined as the following criteria: (1) Abnormalities in the ST segment: the ST segment was measured at 80 ms after J point, and the meaningful change was described as ST-segment depression ≥0.05 mV, or ST-segment elevation ≥0.10 mV in limb leads and/or ≥0.20 mV in chest leads. (2) T-wave abnormalities: a. high and sharp T wave: the peak of T wave was >0.5 mV in limb leads and/or >1.5 mV in chest leads; b. low and flat T wave: the peak of T wave was <0.1 mV in limb leads or <0.2 mV in chest leads; c. bidirectional T wave; d. inversed T wave (inversion depth ≥0.1 mV). Secondary ST-T changes caused by ventricular pre-excitation, intraventricular conduction block, and ventricular pacing rhythm were not included. QT interval is determined between the earliest ventricular depolarization point and the latest T-wave ending point. QTc interval prolongation was defined as corrected QT (QTc) interval (Bazett formula) was ≥450 ms in male and ≥460 ms in female. The measurement and diagnosis of each case were independently analyzed by two experienced cardiologists.
2.3 Statistical analysis
Categorical variables were depicted as frequency rates with percentages, and continuous variables were described using median and interquartile range (IQR) values. After the normal distribution test, Mann–Whitney U test, chi-square test, or Fisher's exact test were used to compare differences between the ICU group and non-ICU group where appropriate. p < .05 was considered statistically significant. The inclusion criteria of independent variables in binary regression analysis were as follows: a. dichotomous variables with statistically significant differences; b. variables with no potentially collinearity (such as CVDs and coronary heart disease, arrhythmias, and atrial tachycardia); c. variables associated with adverse cardiac events and may aggravate the condition in patients with COVID-19. All statistical analyses were calculated by Statistical Package for the Social Sciences (SPSS) version 21.0 software.
3 RESULTS
3.1 Baseline characteristics
A total of 135 hospitalized patients with COVID-19 were included in this analysis. Twenty-three (17.0%) patients were admitted or transferred to the ICU since the aggravation of infection and multiple organs injury. Six (4.4%) patients died during hospitalization. The median age of 135 patients was 64 years (IQR, 48–72), and over half of patients were male (Table 1). About 45.2% of patients had cardiovascular diseases (CVDs). Hypertension (32.6%), diabetes (14.8%), and coronary heart disease (8.1%) were the top three most common comorbidities. The most common cardiovascular medication prescribed was calcium channel blockers, followed by oral antidiabetic agents and angiotensin-converting enzyme inhibitors/angiotensin receptor blocker (ACEI/ARB). Compared with patients who were not admitted to ICU (n = 112), patients who received ICU care (n = 23) are significantly older (71 years [55–76] vs. 64 years [47–69]; p = .037) and were more likely to complicate with underlying CVDs (18 [78.3%] vs. 43 [38.4%]; p < .001).
| No. (%) | ||||
|---|---|---|---|---|
| Total (n = 135) | ICU (n = 23) | Non-ICU (n = 112) | p value | |
| Age, median (IQR), years | 64 (48–72) | 71 (55–76) | 64 (47–69) | .037 |
| Male | 69 (51.1) | 17 (73.9) | 52 (46.4) | .016 |
| Cardiovascular comorbidity | 61 (45.2) | 18 (78.3) | 43 (38.4) | <.001 |
| Hypertension | 44 (32.6) | 10 (43.5) | 34 (30.4) | .221 |
| Diabetes | 20 (14.8) | 5 (21.7) | 15 (13.4) | .481 |
| Hyperlipidemia | 2 (1.5) | 1 (4.3) | 1 (0.9) | .313 |
| Coronary heart disease | 11 (8.1) | 5 (21.7) | 6 (5.4) | .028 |
| Previous myocardial infarction | 2 (1.5) | 0 | 2 (1.8) | >.999 |
| Stroke | 7 (5.2) | 4 (17.4) | 3 (2.7) | .017 |
| Previous PCI procedure | 7 (5.2) | 4 (17.4) | 3 (2.7) | .017 |
| Permanent pacemaker | 2 (1.5) | 0 | 2 (1.8) | >.999 |
| Medication history | ||||
| β receptor blocker | 4 (3.0) | 1 (4.3) | 3 (2.7) | .531 |
| Calcium channel blocker | 20 (14.8) | 6 (26.1) | 14 (12.5) | .178 |
| ACEIs/ARBs | 13 (9.6) | 2 (8.7) | 11 (9.8) | >.999 |
| Oral anti-diabetic agents | 15 (11.1) | 3 (13.0) | 12 (10.7) | >.999 |
| Antiplatelet agents | 6 (4.4) | 1 (4.3) | 5 (4.5) | <.999 |
- Abbreviations: ACEIs, angiotensin-converting enzyme inhibitors; ARBs, angiotensin receptor blockers; IQR, interquartile range; PCI, percutaneous coronary intervention.
3.2 ECG characteristics
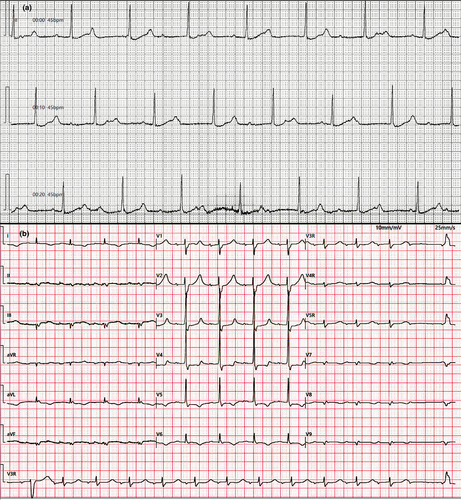
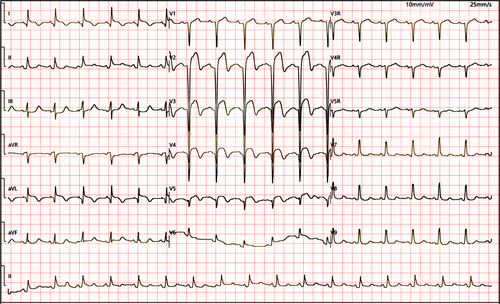
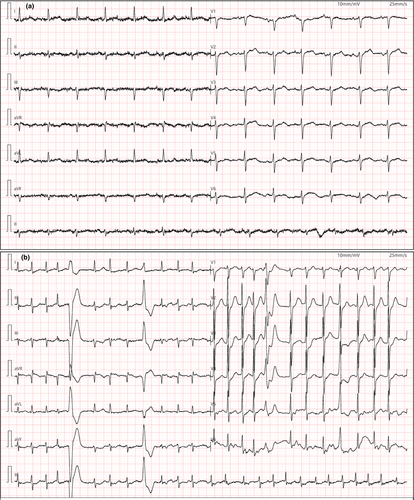
ECG characteristics showed a variety of difference between the two groups. Patients in the ICU presented higher heart rate (93.2 ± 26.4 vs. 79.0 ± 14.6 bpm; p = .019) and P-wave duration (110 [92–111] vs. 110 [102–117] ms; p = .039) (Table 2). ST-T abnormalities (40%) were the most common ECG changes in patients with COVID-19, followed by total arrhythmias (37.8%) and left atrial abnormality (14.8%). Two patients with acute myocarditis developed third-degree atrioventricular block (Figure 1a), and one patient with coronary heart disease presented second-degree type I atrioventricular block (Figure 1b). Five patients were admitted with ST-segment elevation, which was later diagnosed as acute ST-segment elevation myocardial infarction by coronary angiography (Figure 2). Compared with the non-ICU group, patients in ICU were more prone to manifest ST-T abnormalities (15 [65.2%] vs. 39 [34.8%]; p = .007), QTc interval prolongation (8 [34.8%] vs. 10 [8.9%]; p = .003), and pathological Q wave (7 [30.4%] vs. 4 [3.6%]; p < .001), as well as arrhythmias (Table 2). During hospitalization, 27 patients were re-examined ECG and 17 of them presented new findings compared with their initial ECG results (Table 3). ST-T abnormalities (5/17), atrial fibrillation (3/17) and left ventricular hypertrophy (3/17) were the three most common emerging ECG changes (Figure 3). The initial ECG abnormalities of 4 patients were resolved in re-examination.
| No. (%) | ||||
|---|---|---|---|---|
| Total (n = 135) | ICU (n = 23) | Non-ICU (n = 112) | p value | |
| Basic parameters | ||||
| Heart rate, bpm | 81.4 ± 17.8 | 93.2 ± 26.4 | 79.0 ± 14.6 | .019 |
| P-wave durationa, median (IQR), ms | 110 (101–116) | 110 (92–111) | 110 (102–117) | .039 |
| PR intervald, ms | 157.3 ± 24.7 | 151.6 ± 23.7 | 158.4 ± 24.9 | .274 |
| QRS complex duration, median (IQR), ms | 93 (86–102) | 94 (85–105) | 92 (86–102) | .572 |
| Frontal plane QRS axis, degree | 33.6 ± 44.6 | 32.2 ± 75.4 | 33.8 ± 35.7 | .921 |
| QTc interval, ms | 435.0 ± 31.7 | 447.8 ± 52.9 | 432.4 ± 24.8 | .184 |
| ECG diagnosis | ||||
| Normal | 30 (22.2) | 1 (4.3) | 29 (25.9) | .024 |
| ST-T abnormalitiesb | 54 (40.0) | 15 (65.2) | 39 (34.8) | .007 |
| Conduction block | 16 (11.9) | 4 (17.4) | 12 (10.7) | .584 |
| First degree AVB | 5 (3.7) | 0 | 5 (4.5) | .588 |
| Second-degree type I AVB | 1 (0.7) | 1 (4.3) | 0 | .170 |
| Third-degree AVB | 2 (1.5) | 2 (8.7) | 0 | .028 |
| Right bundle branch block | 5 (3.7) | 2 (8.7) | 3 (2.7) | .201 |
| Left anterior fascicular block | 2 (1.5) | 0 | 2 (1.8) | >.999 |
| Intraventricular conduction delay | 4 (3.0) | 1 (4.3) | 3 (2.7) | .531 |
| Atrial and ventricular arrhythmias | 20 (14.8) | 9 (39.1) | 11 (9.8) | .001 |
| Atrial premature complex | 5 (3.7) | 3 (13.0) | 2 (1.8) | .035 |
| Atrial tachycardia | 5 (3.7) | 4 (17.4) | 1 (0.9) | .002 |
| Atrial fibrillation | 8 (5.9) | 1 (4.3) | 7 (6.3) | >.999 |
| Ventricular premature complex | 6 (4.4) | 4 (17.4) | 2 (1.8) | .006 |
| Sinus tachycardia | 9 (6.7) | 1 (4.3) | 8 (7.1) | .976 |
| Sinus bradycardia | 11 (8.1) | 1 (4.3) | 10 (8.9) | .754 |
| Arrhythmias (total)c | 51 (37.8) | 15 (65.2) | 36 (32.1) | .003 |
| QTc interval prolongation | 18 (13.3) | 8 (34.8) | 10 (8.9) | .003 |
| Abnormal Q wave | 11 (8.1) | 7 (30.4) | 4 (3.6) | <.001 |
| Extensive anterior wall (V1-V6, I, aVL) | 1 (0.7) | — | — | — |
| Antero-septal wall (V1-V3) | 3 (2.2) | — | — | — |
| Anterior wall (V3-V5) | 2 (1.5) | — | — | — |
| Inferior wall (II, III, aVF) | 5 (3.7) | — | — | — |
| Posterior wall (V7-V9) | 1 (2.2) | — | — | — |
| Low voltage in limb leads | 6 (4.4) | 3 (13.0) | 3 (2.7) | .101 |
| Left ventricular hypertrophy | 8 (5.9) | 1 (4.3) | 7 (6.3) | >.999 |
| Left atrial abnormality | 20 (14.8) | 1 (4.3) | 19 (17.0) | .219 |
| Right atrial abnormality | 2 (1.5) | 0 | 2 (1.8) | >.999 |
| Othersd | 4 (3.0) | — | — | — |
- Abbreviation: AVB, atrioventricular block.
- a P-wave duration and PR interval were not measured in a total of 11 patients (4 in ICU group and 7 in non-ICU group) with atrial fibrillation, the third-degree AVB or ventricular pacing rhythm.
- b ST-T abnormality: including 5 cases of acute myocardial infarction.
- c Arrhythmias: including sinus tachycardia, bradycardia, conduction block, atrial and ventricular arrhythmias. Multiple arrhythmias from one patient were counted once.
- d Others: including short PR interval and ventricular pacing rhythm.
| New ECG findingsa | No. |
|---|---|
| Pathological Q wave | 2 |
| ST-T abnormality | 5 |
| Atrial premature complex | 1 |
| Ectopic atrial rhythm | 1 |
| Atrial fibrillation | 3 |
| Ventricular premature complex | 1 |
| Limb lead low voltage | 1 |
| Intermittent bundle branch block | 1 |
| QTc prolongation | 1 |
| Left ventricle hypertrophy | 3 |
| Resolved ECG abnormalities | |
| Sinus tachycardia resolved | 1 |
| Atrial tachycardia resolved | 1 |
| ST-T abnormalities resolved | 1 |
| QTc prolongation resolved | 1 |
- a A total of 27 patients re-examined ECG during admission, and 10 of them presented no significant changes compared with their initial ECG results.
3.3 Risk factors for admission to ICU
After the procedure elaborated earlier, a history of CVD, cardiac arrhythmias, gender (male), ST-T abnormalities, and QTc prolongation were included into our final binary logistic regression. We found that ST-T abnormalities (p = .040, C.I. [1.054–9.298]) and CVD history (p = .047, C.I. [1.015–10.598]) at admission were associated with increased odds of ICU admission (Table 4).
| B | SE | Wal | Sig. | Exp (B) | 95% CI | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | 1.188 | 0.598 | 3.940 | 0.047 | 3.280 | 1.015–10.598 |
| Male | 1.127 | 0.599 | 3.545 | 0.060 | 3.087 | 0.955–9.983 |
| Arrhythmias | 0.594 | 0.582 | 1.042 | 0.307 | 1.811 | 0.579–5.662 |
| ST-T abnormalities | 1.141 | 0.555 | 4.221 | 0.040 | 3.130 | 1.054–9.298 |
| QTc interval prolongation | 0.727 | 0.640 | 1.287 | 0.257 | 2.068 | 0.589–7.256 |
- a Binary logistic regression: enter method.
4 DISCUSSION
This retrospective study revealed the ECG characteristics and risk factors of ICU admission in patients with COVID-19. Previous studies have confirmed that SARS-CoV can cause the ECG abnormalities in both animals and humans (Alexander et al., 1999; Yu et al., 2006). As a virus homologous to SARS-CoV, SARS-CoV-2 was also found to be potentially arrhythmogenic. Wang et al. showed 16.7% (23/138) of COVID-19 patients combined with arrhythmias and were more common in the ICU group (44.4% vs. 6.9%, p < .001) (Wang et al., 2020). However, comprehensive investigations on the ECG characteristics in patients with COVID-19 are still sparse.
In our study, we found that only 25% of COVID-19 patients presented generally normal ECG and ST-T abnormalities were the most prominent ECG manifestation among the patients with COVID-19. The ST-segment elevation in COVID-19 patients is mainly due to obstructive/nonobstructive coronary artery diseases, myocarditis, pericarditis, or stress cardiomyopathy (Dehghani et al., 2020; Inciardi et al., 2020). However, the exact reasons for the other nonspecific ST-T abnormalities remain unclear. Infection-mediated myocardial injury and prior CVD comorbidities may contribute.
Cardiac arrhythmias (37.8%) were the second most common ECG change and should be taken seriously because some arrhythmias can be life-threatening. Two patients in our cohort occurred complete AVB on admission, and one of them had undertaken a permanent pacemaker implantation due to syncope. Recent studies have shown fatal arrhythmias including complete AVB, polymorphic ventricular tachycardia, and ventricular fibrillation in patients with COVID-19 (Kochav et al., 2020; Kir et al., 2020; Guo et al., 2020). The high prevalence of arrhythmias may be attributed to metabolic disorders, hypoxia, neurohormonal imbalance, or inflammatory reaction in patients with or without prior CVD (Driggin et al., 2020).
Although QTc prolongation was more common in the ICU group (34.8% vs. 8.9%), there was no significant difference in values between the two groups in our cohort (p = .184). Jain S et al. reported that 19.7% (103/524) of patients with COVID-19 had prolonged QTc interval and were more likely to be admitted to the ICU (Jain et al., 2020). Drugs for treating COVID-19 were regarded as the main cause of QTc prolongation, and this effect may be amplified when multiple QT-prolonging drugs were used in combination. Hydroxychloroquine (HCQ), lopinavir/ritonavir, and azithromycin have been confirmed to prolong the QTc interval in patients with COVID-19 (Sacher et al., 2020). Moreover, some inflammatory factors (TNF-α, IL-6) and electrolyte disturbance may potentially contribute to this process (Cipriani et al., 2020). Abnormal Q wave often indicated myocardial necrosis or stun, which may be caused by myocarditis and were associated with a poor prognosis (Buttà et al., 2020). This partially explained why the Q waves are more common in the ICU group.
As for risk factors, ST-T abnormalities and history of CVD were identified to increase the odds of ICU admission in our cohort. ST-T changes were not uncommon in patients with COVID-19 and often indicated ventricular repolarization abnormalities, which may be a potential cause of severe arrhythmias (Angeli et al., 2020). Comprehensive assessment on drug interactions, electrolyte abnormalities, and ECG changes was imperative for the patients with CVD history on admission, because they were more sensitive to factors that could potentially lead heart injury (Kochi et al., 2020).
Finally, ECG changes during admission cannot be ignored or may be even more important. Although we did not re-examine the ECG for all the patients because of minimizing exposure of healthcare workers, ECG changes were observed in more than 60% of patients (17/27). New or worsening ECG abnormalities in patients with pneumonia often indicated the degree of cardiac involvement (Corrales-Medina et al., 2013; Stein et al., 2012). Hui et al. (Hui et al., 2020) reported two critically ill patients with COVID-19 developed new AF during hospitalization and eventually died.
To the best of our knowledge, this is the largest retrospective study regarding initial ECG manifestations among patients with COVID-19. The novel findings of this study are the CVD comorbidities and ECG abnormalities were not uncommon in patients with COVID-19 and some of which could be life-threatening. History of CVD and ST = T abnormalities were associated with increased odds of ICU admission. The ECG is a simple and useful screening tool, which can help us promptly assess the cardiac complications while avoiding adverse cardiac events during admission.
4.1 Study limitations
The following limitations of our study should be noted. First, not all patients had serial ECG recordings, and therefore, some transient ECG changes might have been missed. Second, because of the difficulty in obtaining the prior medical data due to the COVID-19 pandemic, there is a lack comparison of patient's previous ECG. Finally, as the logistic regression analysis in this study did not include laboratory indicators and some confirmed risk indicators, there may be selection bias in the process.
ACKNOWLEDGMENTS
My deepest gratitude goes foremost to Professor Tong Liu and Miss Xue for their constant encouragement and guidance. They have walked me through all the stages of the writing of this article.
CONFLICT OF INTEREST
The authors declared that they have no conflicts of interest to this work. We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
AUTHOR CONTRIBUTIONS
Yi Li: Conceptualization, Software, Formal analysis, Resources, Writing original draft. Tong Liu: Methodology, Writing and Revision. Gary Tse: Investigation, Revision. Mingxiang Wu: Supervision. Jingjing Jiang: Data collection and curation. Ming Liu: Correction. Liang Tao: Validation.
ETHICS
The study complied with the edicts of the Declaration of Helsinki (World Medical Association, 2013) and was approved by the Research Ethics Commission of Wuhan Asia General Hospital (WAGHMEC-KY-2020005). Given the retrospective review of this study, informed consent was waived.