Fragmented QRS in prediction of ischemic heart disease diagnosed by stress cardiovascular magnetic resonance imaging
Abstract
Background
In patients with ischemic heart disease (IHD), many studies demonstrated an association between fragmented QRS complex (fQRS) on 12-lead ECG and myocardial scar, heart failure, and increased mortality. However, data in adults without history of IHD is limited. We aimed to evaluate whether there is an association between fQRS and IHD diagnosed by stress cardiac MRI.
Method
We retrospectively reviewed demographic data, 12-lead ECG, and stress cardiac MRI data from 604 patients. Fragmented QRS was defined as the presence of additional R wave (R’), notching in the nadir of R or S wave, or the presence of more than one R’ in any ECG leads. Both cardiac MRI and ECG were analyzed by two independent observers.
Result
Final analysis included 554 patients, 39% were male, with a mean age of 67.8 ± 11.1 years. There was positive stress cardiac MRI in 219 patients (39.5%). Older age, diabetes mellitus, and hypertension were more frequent in the positive group (p < .05). fQRS was identified in 300 patients (54.2%). Baseline characteristic did not differ significantly between patients with and without fQRS. There is an association between fQRS and IHD, OR 1.605 (95% CI 1.14–2.27), p = .007. After adjustment for age, diabetes, hypertension, renal function, and left ventricular ejection fraction, the strong association between fQRS and IHD persisted, OR 1.71 (95% CI 1.18–2.47), p = .004.
Conclusion
In patients without known history of coronary artery disease, fragmented QRS is independently associated with ischemic heart disease diagnosed by stress cardiac MRI.
1 INTRODUCTION
Ischemic heart disease (IHD) is among the most common cause of death worldwide (Roth et al., 2017). Despite a trend toward a lower cardiovascular disease (CVD) mortality in Western countries, the burden is markedly increasing in developing countries (Roth et al., 2017; Townsend et al., 2016). In those who have significant coronary artery stenosis, early diagnosis is mandatory to guide a timely treatment.
Several noninvasive stress tests are available for the detection of coronary artery disease (CAD) with different sensitivity and specificity (Montalescot et al., 2013). Among these, stress cardiovascular magnetic resonance imaging (MRI) has an excellent accuracy in diagnosis of significant CAD, without significant difference between vasodilator stress test, or dobutamine stress test. Moreover, with combined use of the delayed enhancement imaging technique, the diagnostic accuracy of CAD increases over stress perfusion imaging alone (Klem et al., 2006). With a negative test result, the risk of either nonfatal myocardial infarction or cardiovascular death is <1% per year (Lipinski, McVey, Berger, Kramer, & Salerno, 2013). MRI can provide other associated cardiac information, resulting in a comprehensive assessment on myocardial structure and function, valvular heart disease, as well as the adjacent extracardiac structures, such as the thoracic aorta and pulmonary arteries. In addition, detection of myocardial scar from late gadolinium enhancement sequence is associated with worse cardiovascular outcome.
Standard 12-lead ECG is readily available, not time-consuming, and is among the first investigation recommended in all patients with suspected CAD (Montalescot et al., 2013). Recent studies demonstrated that fragmented QRS complex (fQRS) on ECG was associated with history of myocardial infarction and detection of myocardial scar (Das, Khan, Jacob, Kumar, & Mahenthiran, 2006; Das et al., 2008; Tangcharoen et al., 2013), arrhythmia (Das et al., 2010; Take & Morita, 2012), and increased cardiovascular mortality (Das et al., 2008; Pietrasik & Zareba, 2012; Rosengarten, Scott, & Morgan, 2015). However, majority of patients in these studies were already diagnosed with heart disease, namely IHD and cardiomyopathies. Data in adults without known history of CAD are still limited. In the present study, we aimed to determine the importance of fQRS as a screening tool for CAD by evaluating the association between fQRS and significant coronary artery stenosis diagnosed by stress cardiac MRI.
2 METHODS
2.1 Study design and population
Consecutive data from adults age 18 years or older, who underwent stress cardiac MRI at Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand, between 1st January 2015 and 31st December 2017 were reviewed. Referred patients who did not have in-hospital medical records were excluded, as well as those who had established CAD. Demographic data were reviewed, which included age, sex, weight, height, presenting symptoms that necessitate the stress testing, personal history of smoking and medical comorbidities, and family history of atherosclerotic cardiovascular events. Age, sex, and character of chest pain were used to calculate pretest probability of having obstructive CAD, according to the European Society of Cardiology guideline (Montalescot et al., 2013).
Cardiac MRI was performed using 1.5 Tesla magnetic resonance scanner (Philips Achieva release 3.2). Resting left ventricular systolic function was acquired with steady-state free precession sequence in short-axis orientation. Stress test was done using medication, either adenosine (dosage of 140 mcg/kg/min for 4 min) or dobutamine infusion (titrated per protocol to achieve the target heart rate). First-pass perfusion scan was performed immediately after completion of adenosine or dobutamine, with the administration of gadolinium-based contrast. Resting perfusion scan images were acquired 5 min later. All perfusion images were obtained in short-axis view using gradient echo pulse sequence. Late gadolinium enhancement imaging was acquired with phase-sensitive inversion recovery sequence in short-axis and long-axis views (2-, 3-, and 4-chamber views). Total amount of gadolinium use was 0.075–0.1 mmol/kg per case. Images were analyzed by two observers using Extended MR WorkSpace release 2.6.
All patients had 2 sets of standard 12-lead ECG done on the same day with cardiac MRI, before and after stress testing. The ECG obtained prior to stress test were used for analysis of fQRS, which were done by two observers who were blinded from the MRI result. The study protocol was approved by the institutional ethics committees.
2.2 Definition
A positive stress cardiac MRI result was defined by either (a) a stress-induced perfusion defect or a stress-induced regional wall motion abnormality that was detected in at least 2 contiguous myocardial segments corresponding to epicardial coronary territory, or (b) a presence of ischemic myocardial scar, defined as hyper-enhanced area of subendocardial or transmural myocardium in late gadolinium enhancing sequence. Transient thin subendocardial low signal intensity during first-pass perfusion study (dark rim artifact) and nonischemic myocardial scar were not counted as positive stress MRI.
In patients with narrow QRS complex (QRS duration <120 ms), fQRS was defined as the presence of additional R wave (R’), or notching in the nadir of R or S wave, or the presence of more than one R’ (Das et al., 2006). In wide QRS complex patients (QRS duration ≥ 120 ms), fQRS was defined as the presence of >2 R waves, or >2 notches in the R wave, or >2 notches in the upstroke or downstroke of the S wave (Das et al., 2008). The presence of abnormal QRS morphology according to these criteria in any ECG leads was classified as having fQRS.
2.3 Statistical analysis
Patient characteristics were reported as mean ± standard deviation for continuous variables and as frequencies and percentages for categorical variables. Student's t test and chi-square test were used for between-group comparison. Association between fQRS and IHD was derived from regression analysis, while the area under the curve of receiver operating characteristic (ROC) curve was used to evaluate the diagnostic accuracy of fQRS. All analyses were performed using Statistical Package for the Social Sciences (SPSS) version 25.0.0.
3 RESULTS
During 1st January 2015 to 31st December 2017, there were 604 patients who underwent stress cardiac MRI. Forty-seven patients were excluded due to known history of CAD, and three patients whose stress testing were incomplete because of medication adverse effects were also excluded. The final analysis included 554 patients; 216 (39%) were male, with a mean age of 67.8 ± 11.1 years. Hypertension and dyslipidemia were common among the cohort (77.5% and 90.9%, respectively), while diabetes mellitus and chronic kidney disease were less prevalent.
Stress cardiac MRI was performed using adenosine as a vasodilator agent in 520 patients, and dobutamine was used in other 34 patients. Gadolinium-based contrast agent was not administered in seven patients due to advanced renal dysfunction. There was positive stress test in 219 patients (39.5%); 192 patients had drug-induced perfusion defect without ischemic myocardial scar (median 6 segments). Ischemic myocardial scar was presented in 27 patients; one patient had only transmural scar, 17 had subendocardial scar, and nine patients had both subendocardial and transmural gadolinium enhancing pattern. Median of myocardial segments with scar was 5.5 segments. There was only three patients who had perfusion defect corresponding to the area of ischemic scar, and while in another 24 patients, the segments with perfusion defect extended beyond the segments with scar. Of 547 patients who received gadolinium injection, nonischemic pattern of late gadolinium enhancement (e.g., enhancement of right ventricular insertion point or midwall enhancement) was observed in 169 patients, with 71 patients having positive stress test and 98 patients with negative stress MRI. Baseline clinical characteristics between those with positive and negative test result is shown in Table 1, which showed that older age, diabetes, and hypertension were more prevalent in the positive test group. Mean baseline left ventricular ejection fraction (LVEF) was slightly higher in those with negative stress test.
|
All n = 554 |
Stress MRI (+) n = 219 |
Stress MRI (−) n = 335 |
p-Value | |
|---|---|---|---|---|
| Age (years) | 67.84 ± 11.05 | 69.38 ± 9.99 | 66.83 ± 11.60 | .006 |
| Male sex |
216/554 (39%) |
85/219 (38.8%) |
131/335 (39.1%) |
.945 |
| BMI (kg/m2) | 26.03 ± 4.32 | 25.84 ± 4.54 | 26.16 ± 4.17 | .394 |
| Pretest probability | 43.55 ± 17.39 | 45.12 ± 17.47 | 42.52 ± 17.28 | .085 |
| Diabetes mellitus |
166/504 (32.9%) |
81/208 (38.9%) |
85/296 (28.7%) |
.016 |
| Hypertension |
428/552 (77.5%) |
179/218 (82.1%) |
249/334 (74.6%) |
.038 |
| Dyslipidemia |
470/517 (90.9%) |
196/213 (92%) |
274/304 (90.1%) |
.463 |
| Chronic kidney disease |
111/554 (20%) |
50/219 (22.8%) |
61/335 (18.2%) |
.184 |
| eGFR (ml/min/1.73 m2) | 77.20 ± 17.83 | 75.41 ± 17.85 | 78.38 ± 17.75 | .056 |
| LVEF (%) | 67.39 ± 8.34 | 66.39 ± 9.29 | 68.04 ± 7.60 | .029 |
| Ischemic LGE |
27/547 (4.9%) |
27/216 (12.5%) |
0/331 (0%) |
.148 |
| Nonischemic LGE |
169/547 (30.9%) |
71/216 (32.9%) |
98/331 (29.6%) |
.548 |
Note
- Data are shown as n (%) or mean ± SD.
- Abbreviations: BMI, body mass index; eGFR, estimated glomerular filtration rate (calculated by CKD-EPI formula); LGE, late gadolinium enhancement; LVEF, left ventricular ejection fraction.
fQRS was identified in 300 out of 554 patients (54.2%), with 134 patients having positive stress MRI (61.2% prevalence among the positive MRI group). There was no statistically significant difference in demographic data between those with or without fQRS, as shown in Table 2. Mean resting left ventricular systolic function and the presence of myocardial scar, either ischemic or nonischemic pattern, did not significantly differ between groups. The majority of patients with fQRS had ≤3 leads of involvement (median was one lead; frequency reported in Table 3), and the most frequent lead with positive fQRS was the limb lead III (distribution of fQRS reported in Table 4). Presence of two or more contiguous leads with fQRS was observed in 180 out of 300 patients (60%) and was most frequently identified in inferior leads (II, III, or aVF; n = 152 (84.4%)).
|
All n = 554 |
fQRS (+) n = 300 |
fQRS (−) n = 254 |
p-Value | |
|---|---|---|---|---|
| Age (years) | 67.84 ± 11.05 | 67.92 ± 10.74 | 67.75 ± 11.43 | .861 |
| Male sex |
216/554 (39%) |
122/300 (40.7%) |
94/254 (37.0%) |
.379 |
| BMI (kg/m2) | 26.03 ± 4.32 | 26.01 ± 4.20 | 26.07 ± 4.46 | .874 |
| Pretest probability | 43.55 ± 17.39 | 44.07 ± 17.10 | 42.93 ± 17.73 | .441 |
| Diabetes mellitus |
166/504 (32.9%) |
83/272 (30.5%) |
83/232 (35.8%) |
.21 |
| Hypertension |
428/552 (77.5%) |
237/300 (79.0%) |
191/252 (75.8%) |
.369 |
| Dyslipidemia |
470/517 (90.9%) |
257/280 (91.8%) |
213/237 (89.9%) |
.451 |
| Chronic kidney disease |
111/554 (20%) |
61/300 (20.3%) |
50/254 (19.7%) |
.849 |
| eGFR (ml/min/1.73 m2) | 77.20 ± 17.83 | 76.14 ± 17.61 | 78.46 ± 18.04 | .126 |
| LVEF (%) | 67.39 ± 8.34 | 67.13 ± 8.80 | 67.70 ± 7.77 | .423 |
| Ischemic LGE |
27/547 (4.9%) |
20/295 (6.8%) |
7/252 (2.8%) |
.163 |
| Nonischemic LGE |
169/547 (30.9%) |
101/295 (34.2%) |
68/252 (27.0%) |
.078 |
Note
- Data are shown as n (%) or mean ± SD.
- Abbreviations: BMI, body mass index; eGFR, estimated glomerular filtration rate (calculated by CKD-EPI formula); LGE, late gadolinium enhancement; LVEF, left ventricular ejection fraction.
| Number of leads | n | % |
|---|---|---|
| 0 | 254 | 45.8 |
| 1 | 93 | 16.8 |
| 2 | 111 | 20 |
| 3 | 69 | 12.5 |
| 4 | 21 | 3.8 |
| 5 | 5 | 0.9 |
| 6 | 0 | 0 |
| 7 | 1 | 0.2 |
| Lead | n |
|---|---|
| I | 6 |
| II | 58 |
| III | 199 |
| aVL | 39 |
| aVF | 167 |
| V1 | 95 |
| V2 | 43 |
| V3 | 15 |
| V4 | 10 |
| V5 | 7 |
| V6 | 2 |
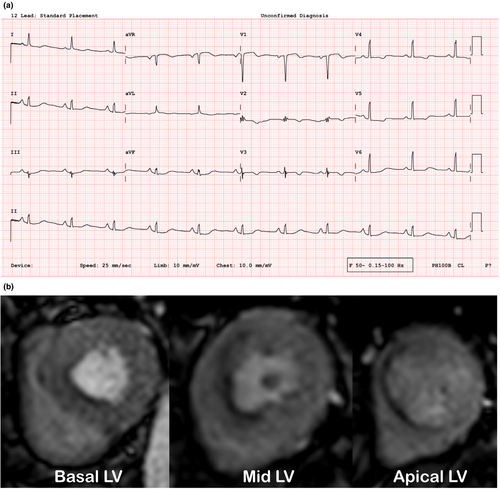
There was an association between fQRS and IHD diagnosed by positive stress MRI, OR 1.61 (95% CI 1.14–2.27), p = .007. Moreover, the presence of fQRS was associated with an ischemic myocardial scar detected by late gadolinium enhancing MRI sequence, OR 2.55 (95% CI 1.06–6.12, p = .037). Analysis of 520 patients without ischemic scar detected from cardiac MRI showed that fQRS was associated with positive stress cardiac MRI test with an odds ratio of 1.47, 95% CI 1.03–2.11 (p = .036). Using linear regression model, the number of leads with positive fQRS showed an association with IHD (OR 1.20 (95% CI 1.06–1.37), p = .005). Presence of fQRS in 2 or more contiguous leads was also associated with positive stress MRI, OR 1.90 (95% CI 1.32–2.73), p = .001. Figure 1 showed an example of a patient with multiple fQRS who was found to have a positive stress MRI. Nonischemic myocardial scar was not significantly associated with the presence of fQRS (OR 1.39 (95% CI 0.96–2.00), p = .08). Using multivariate analysis adjusted for age, diabetes, hypertension, renal function, and LVEF (as shown in Table 5), fQRS remained an independent predictor for positive stress MRI, OR 1.71 (95% CI 1.18–2.47), p = .004.
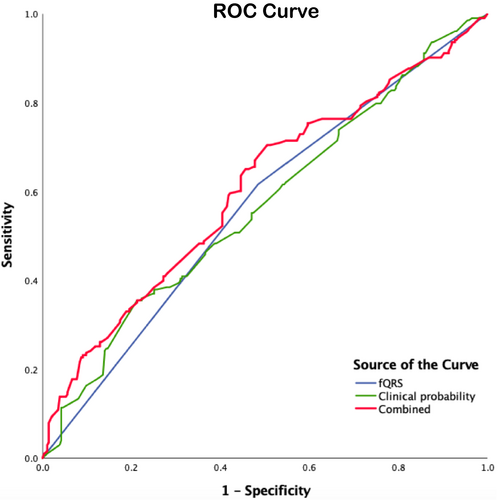
When considering stress cardiac MRI as a gold standard test, sensitivity of using fQRS alone in diagnosis of IHD was 61.2%, and specificity was 50.5%. Positive and negative predictive values were 44.7% and 66.5%, respectively. Clinical probability derived from multiple patient characteristics: pretest probability (which includes age, sex, and symptom of chest pain), diabetes, hypertension, dyslipidemia, and chronic kidney disease, yielded the area under the ROC curve of 0.57. The area under the curve of fQRS yielded similar value (AUROC = 0.57). The combination of clinical probability together with fQRS slightly increased the AUROC to 0.61, as shown in Figure 2.
| OR | 95% CI | p-Value | |
|---|---|---|---|
| Age | 1.013 | 0.992–1.035 | .234 |
| Diabetes mellitus | 1.532 | 1.032–2.274 | .034 |
| Hypertension | 1.194 | 0.737–1.935 | .471 |
| eGFR | 0.999 | 0.987–1.011 | .904 |
| LVEF | 0.972 | 0.950–0.994 | .014 |
| fQRS | 1.709 | 1.182–2.470 | .004 |
- Abbreviations: eGFR, estimated glomerular filtration rate; LVEF, left ventricular ejection fraction.
Coronary angiography was performed in 117 patients who had positive stress MRI result. There were 15 cases with normal angiographic findings, and 102 patients had atherosclerotic coronary artery disease. Association between fQRS and angiographic findings of atherosclerotic CAD was observed with an odds ratio of 3.28 (95% CI 1.08–10.00), p = .037.
4 DISCUSSION
The present study demonstrated that in patients without prior history of CAD, the presence of fQRS on 12-lead ECG had a significant association with ischemic heart disease diagnosed from stress MRI, even after adjustment for age and other comorbidities. fQRS also had a similar predictive value as conventional clinical probability derived from multiple patient characteristics.
Previous researches have focused on the association between fQRS and myocardial scar. Early publication reported an association between various RSR’ pattern without a typical bundle-branch block feature on 12-lead ECG and left ventricular aneurysm and wall motion abnormalities (Reddy et al., 2006). Das, et al. subsequently conducted a research which showed that fQRS, compared to Q wave, was more sensitive and had a higher negative predictive value in detection of myocardial scar from nuclear stress test (Das et al., 2006). Further study in patients with wide QRS complex (QRS duration > 120 ms) also found that fragmented wide QRS was highly specific for myocardial scar (Das et al., 2008). Over half of the patients in these studies were already diagnosed with CAD before enrollment, compromising the use of fQRS as a screening tool for CAD. Moreover, the association between fQRS and myocardial ischemia without scar was not mentioned.
In this study, we demonstrated that fQRS was associated with ischemic myocardium detected from stress cardiac MRI regardless of the presence of absence of myocardial scar. And because only patients without history of CAD were included in this study, we propose the utility of fQRS to be broadened to those without established CAD. Therefore, the presence of fQRS in patients suspected to have CAD should warrant clinicians for prompt investigation, which may portend a better prognosis if early diagnosis is made and appropriately treated.
The mechanism causing fQRS remains unclear, but most studies suggested that the presence of injured myocardium, myocardial scar, or fibrosis may disturb a normal conduction, causing a slow conduction and inhomogeneous cellular activation in the area, resulting in abnormally slow myocardium depolarization which appeared as multiple small spikes within the QRS complex on surface ECG (Das et al., 2006; Mittal, 2016; Take & Morita, 2012). The prevalence of fQRS was higher in patients with positive stress cardiac MRI, but was not uncommon among patients with negative stress test. Interpreting fQRS alone, in the absence of other clinical context, as a marker of cardiovascular disease should be avoided as some studies reported no association between the two (Terho et al., 2014; Wang et al., 2014). The presence of fQRS found on annual check-up in healthy adult cohort has been previously reported (prevalence of 5.1%), but its clinical significance remained unknown during the 3-year follow-up period (Tian et al., 2017).
Although we could demonstrate an association between fQRS and IHD in this study, it is noteworthy to mention some limitations. First, data on major atherosclerotic cardiovascular risk were not mentioned in a large number of patients, especially history of stroke or peripheral arterial disease, personal history of smoking, and family history of premature cardiovascular events. Second, because our center is a university hospital, patients were likely to have multiple medical comorbidities and higher-than-average cardiovascular risk than general population. Third, the definition of fQRS varies between studies, as reflected by wide range of prevalence (19 to 55 percent) even in the similar population (Das et al., 2006, 2010; Take & Morita, 2012; Tangcharoen et al., 2013; Terho et al., 2014; Wang et al., 2014), making comparison and clinical application troublesome. Currently, various abnormal pattern of QRS complex are classified together as fQRS, but recent publication suggested that a universal criterion with more detailed classification of fQRS may help reducing data heterogeneity. Fourth, testing for coronary microvascular dysfunction (e.g., coronary flow reserve, acetylcholine provocative test) in patients whose angiographic result revealed nonsignificant coronary artery obstruction was not routinely performed at our institution. Although the MRI results in this study were interpreted by two independent physicians, dark rim artifact, which were to be excluded after having normal coronary anatomy and functional testing, might still be classified as positive stress MRI. Also, the prevalence of coronary microvascular dysfunction in this population was not known due to lack of confirmatory functional testing.
5 CONCLUSION
In patients without known history of CAD, fQRS is independently associated with IHD diagnosed by positive stress cardiac MRI. The presence of fQRS on standard 12-lead ECG in patients with risk factors of CAD or with clinical suspicious for CAD should prompt an early aggressive investigation, in order to confirm the diagnosis and to provide an appropriate treatment for CAD.
ACKNOWLEDGMENT
None.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.