Prehospital recognition of stroke is associated with a lower risk of death
Funding information
This study was funded by the Swedish state under the agreement between the Swedish Government and the County Councils, the ALF agreement (ALFGBG-720211), grants from the Region of Västra Götaland (VGFOUREG-858941), P-O Ahl's Foundation, Wennertröms Foundation, and Rune and Ulla Amlöv's Foundation
Abstract
Objective
Among patients assessed by the emergency medical service (EMS) and hospitalized with a final diagnosis of stroke, to describe delays, patient characteristics, actions taken and outcome in relation to the early recognition of stroke by the EMS clinician.
Methods
Patients admitted to any of six stroke units in Region Västra Götaland, Sweden, with a final diagnosis of stroke from 1 January 2013 to 31 December 2015 were included. Data on follow-up were retrieved from the Swedish Stroke Register.
Results
In all, 5467 patients were included. Stroke was recognized by the EMS clinician in 4396 cases (80.4%). The mean difference in the time from dialling 112 until arrival at the stroke unit was 556 min shorter when stroke was recognized, while the mean difference in the time from dialling 112 until a preliminary report from a computed tomography (CT) scan was 219 min shorter as compared with the patients in whom stroke was not recognized. After adjustment for age, sex, neurological deficits and coma, a lack of suspicion of stroke on EMS arrival was associated with an increased risk of death during three months of follow-up (odds ratio 1.66; 95% confidence interval 1.19–2.32; p = .003).
Conclusion
Among patients with a stroke, more than 80% were recognized by the EMS clinician. Early recognition of stroke was associated with a markedly shorter time until arrival at the stroke unit and until the preliminary report of a CT scan. A lack of early stroke recognition was associated with an increased risk of death.
1 INTRODUCTION
Stroke is one of the most common cardiovascular diseases and may be caused by a broad spectrum of causes/ aetiologies. It has been suggested that about 12 million people suffer a stroke each year from a global perspective.1 Stroke is associated with a high risk of death, as well as various degrees of limitations in daily activities.1, 2 There is a critical time factor in the early phase of stroke which means that, as the minutes pass without optimal treatment, a large number of nerve cells will die.3 The early phase and particularly the time to treatment are therefore critical.4
In the best of scenarios, the patient or a witness will call for an ambulance when there is a suspicion of stroke. Previous experiences suggest that an ambulance is called for in a large proportion of cases with stroke but with some variability between countries.5, 6 If an ambulance is called, it is of the utmost importance that the emergency medical service (EMS) clinician recognizes the disease on the first encounter. Previous experiences from western Sweden suggest that stroke is recognized by the EMS clinician in about two thirds of cases.5 It has also been shown that a minor proportion (2–3%) of patients with TIA/stroke will be assessed as suffering from a harmless condition not requiring ambulance transport to hospital.7
If a suspicion of stroke is raised by the EMS clinician, a prenotification to the hospital can be made, and in smaller studies, this has been shown to reduce the subsequent delays to further investigation and the delivery of treatment.8 Prenotification is a telephone consultation with a neurologist to bypass the emergency department (ED) in order to reduce the time to imaging and intervention. As a result, the optimal early chain of care for stroke starts with early contact with the EMS, followed by the early recognition of stroke by the EMS clinician and finally a prenotification to the hospital.
The aim of the present study was to describe, from a regional perspective, how often cases of stroke are recognized by the EMS clinician and how early recognition will influence the subsequent early chain of care and the final outcome. To the best of our knowledge, no eventual association between the prehospital recognition of stroke and survival has previously been described.
The primary endpoints in the study were as follows: 1) the time from dialling 112 until admission to the stroke unit, 2) the time from dialling 112 until a preliminary report from a computed tomography (CT) scan was delivered and 3) the adjusted risk of death during three months of follow-up.
2 METHODS
2.1 Target population
All the patients who were admitted to any of six of seven stroke units in Region Västra Götaland (all except Södra Älvsborg Hospital) were included in the study. In the geographical catchment area for the study, there are approximately 1.4 million inhabitants.
2.2 EMS organization
Sweden consists of 21 regions, all with their own responsibility for the healthcare provided within the region. In Region Västra Götaland, the EMS is organized in five geographical areas responding to an average of 140,000 primary assignments annually (Södra Älvsborg excluded). The EMS covers an area of 25,000 km2, including both rural and urban areas, with the City of Gothenburg as the most densely populated area (579,000 inhabitants). The EMS is tax funded and a regional emergency medical dispatch centre (EMDC) is responsible for dispatching ambulance resources when a patient telephones the Swedish emergency number (112). All ambulances are equivalent to advanced life-saving (ALS) units with regard to equipment, type of assignments and competence level. According to Swedish legislation, all ambulances are staffed by at least one registered nurse. Within the region, the majority of the registered nurses also have a postgraduate education, specializing in prehospital emergency care.
2.3 Time of inclusion
Patients who were hospitalized between 1 January 2013 and 31 December 2015 were included in the study. Patients were included if they were admitted to a stroke unit, had a final diagnosis of stroke, arrived at hospital by ambulance and were reported to the Swedish Stroke Register. Patients arriving at hospital in an ambulance from another region were excluded, as prehospital delays outside Region Västra Götaland were not available.
2.4 Data sampling
Data were obtained from two registers: 1) the Swedish Stroke Register and 2) Väststroke.
The Swedish Stroke Register is a national quality register to which all patients hospitalized with a final diagnosis of TIA/ stroke in Sweden are reported.
Väststroke is a local quality register for patients with TIA/ stroke who are admitted to a stroke unit at one of the three hospitals in the Municipality of Gothenburg. During the time of the survey (1 January 2013–31 December 2015), Väststroke was extended to include the whole of Region Västra Götaland, excluding Södra Älvsborg Hospital.
Data were transferred from the local hospital databases to the quality registers by local co-ordinators (dedicated nurses who received specific education for this work). Data were entered in the hospital databases prospectively, and the transfer from the hospital databases to the quality registers was made retrospectively.
Data obtained from the Swedish Stroke Register included age, sex, history of stroke, amaurosis fugax, atrial fibrillation, diabetes, hypertension and smoking, living conditions pre-stroke, level of consciousness on admission to hospital, National Institutes of Health Stroke Scale (NIHSS) on admission to hospital, treatment with thrombolysis, treatment with thrombectomy and outcome measurements at three months post-stroke, including living conditions, mobility, need for help with toilet visits, difficulty reading, writing, talking and swallowing, self-reported feeling depressed, general health, fatigue, Modified Ranking Scale and mortality.
Data obtained from Väststroke included suspicion of stroke by the EMS clinician, delays including dialling 112 – EMS dispatch, EMS response time, time on scene, transport time, dialling 112 – arrival at hospital, dialling 112 – arrival at stroke unit, dialling 112 – start of CT scan, dialling 112 – preliminary report of CT scan, dialling 112 – thrombolysis, dialling 112 – thrombectomy; priority at the EMDC and by the EMS clinician; neurological deficits measured by the prehospital modified NIHSS (m NIHSS) and categorized as focal neurology in arms and legs, dysphasia and degree of consciousness; vital parameters including heart rate, systolic blood pressure, oxygen saturation and body temperature; ECG recordings; blood glucose measurement and blood glucose levels. We also obtained data on prenotification by telephone consulting with a stroke physician or a stroke coordinator and whether patients were transported as an acute stroke alert or admitted directly to the stroke unit (both bypassing the ED).
2.5 Ethics
The study was approved by the ethical review board in Gothenburg (approval no. DNR 284–17).
2.6 Data analyses
For descriptive analyses, frequencies and percentages are presented for categorical variables and the mean, median and quartiles, Q1-Q3, respectively, are presented for continuous variables. For comparisons between two groups, Fisher's exact test was used (lowest one-sided p-value multiplied by 2) for dichotomous variables, the Mantel–Haenzel chi-square test for ordered categorical variables and Fisher's non-parametric permutation test for continuous variables. Mean differences with 95% confidence intervals (CI) with effect sizes will be the main results. The confidence interval for dichotomous intervals is the unconditioned exact confidence interval. If no exact limits can be computed, the asymptomatic Wald confidence limits with continuity correction are calculated instead. The confidence interval for the mean difference between groups is based on Fisher's non-parametric permutation test. For the multivariable analysis in Table 4, a logistic regression was used, with three-month mortality as the dependent variable and age, sex, neurological deficit, speech disturbance and decreased consciousness on the arrival of the EMS as covariates. The adjusted risk of death was defined as the odds ratio with 95% confidence limits. In Table 5, univariable and multivariable analyses are presented with odds ratios and 95% confidence intervals for each of the prehospital clinical findings: neurological deficit, speech disturbance, decreased consciousness, heart rate, systolic blood pressure, oxygen saturation, level of blood glucose and EMS performance: EMDC priority, ECG recorded, EMS priority and contact with hospital in terms of association with suspicion of stroke.
3 RESULTS
In all were 5,467 patients, who were assessed by the EMS with a final diagnosis of stroke, included in the study. Among them, a suspicion of stroke was already raised on the first assessment by the EMS clinician in 4,396 cases (80.4%). In what follows, the results will be presented for the total population, as well as in relation to whether or not an early suspicion of stroke was raised. Among all patients, 12.0% had a haemorrhagic stroke, 77.3% had an ischaemic stroke and 10.7% had a stroke of undetermined aetiology.
3.1 Baseline characteristics
Overall, the mean age was 77.2 years and 47.7% were women (Table 1). There were no major differences between the two groups with regard to age, sex and previous history. More than two thirds were living in their own homes without any home care service before the stroke event. Half the patients were living alone. There were no major differences in terms of living conditions, as defined in Table 1, between the two groups.
|
All patients (n = 5467) |
Suspicion of stroke (n = 4396) |
No suspicion of stroke (n = 1071) |
|
|---|---|---|---|
| Age in years (1105)a | |||
| Median (Q1, Q3) | 79 (70,87) | 79 (70,87) | 79 (70,86) |
| Mean ± SD | 77.2 ± 12.5 | 77.4 ± 12.3 | 76.5 ± 13.3 |
| Sex | |||
| Female | 2609 (47.7) | 2103 (47.8) | 506 (47.2) |
| Past medical history | |||
| Stroke (1155) | 1075 (24.9) | 891 (25.0) | 184 (24.4) |
| Amaurosis fugax (1208) | 374 (8.8) | 309 (8.8) | 65 (8.7) |
| Atrial fibrillation (1149) | 1368 (31.7) | 1135 (31.9) | 233 (30.7) |
| Diabetes (1158) | 833 (19.3) | 668 (18.8) | 165 (21.7) |
| Hypertension (1168) | 2607 (60.6) | 2177 (61.5) | 430 (56.8) |
| Smoking (1433) | 464 (11.5) | 384 (11.4) | 80 (11.8) |
| Living conditions (1125) | |||
| Own living without home service | 3004 (69.2) | 2489 (69.6) | 515 (67.2) |
| Own living with home service | 807 (18.6) | 634 (17.7) | 173 (22.6) |
| Specific community living | 518 (11.9) | 444 (12.4) | 74 (9.7) |
| Other | 13 (0.3) | 9 (0.3) | 4 (0.5) |
| Living alone (1134) | |||
| Yes | 2241 (51.7) | 1810 (50.7) | 431 (56.5) |
| Independent in ADL (1112) | |||
| Yes | 39 (0.9) | 33 (0.9) | 6 (0.6) |
| Diagnosis | |||
| Ischaemic stroke (I63) | 4228 (77.3) | 3444 (78.3) | 784 (73.2) |
| Haemorrhagic stroke (ICD I61) | 656 (12.0) | 482 (11.0) | 174 (16.2) |
| Stroke of undetermined aetiology (ICD I64) | 583 (10.7) | 470 (10.7) | 113 (10.6) |
Note
- For categorical variables n (%) is presented.
- Abbreviations: ADL, activities of daily living; ICD, International classification of diseasesQ1, quartile 1; Q3, quartile 3; SD, standard deviation.
- a Missing information.
3.2 Delays
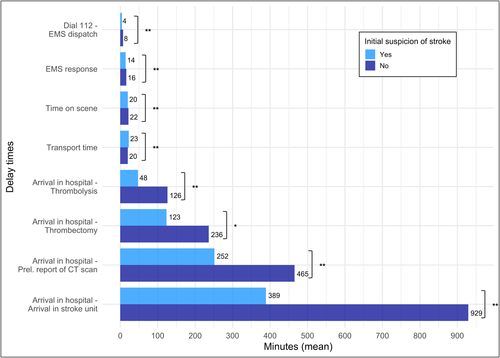
The EMS response time, time on scene and transport time did not differ markedly between the two groups while the mean difference in delay from dialling 112 until EMS dispatch was 3.5 min shorter among patients with initial suspicion of stroke (4.2 versus 7.7 min). The total prehospital delay time from dialling 112 until arrival in hospital was 5 min shorter among patients where there was an initial suspicion of stroke as compared with those in whom it was not (61 versus 66 min). The mean delay from arrival in hospital until there was an initial report from a CT scan was 213 min shorter if there was an initial suspicion of stroke. The mean delay from arrival in hospital until the start of thrombolysis was 78 min shorter and the mean delay from arrival in hospital until thrombectomy was 113 min shorter if there was an initial suspicion of stroke. The mean delay from arrival in hospital until arrival in the stroke unit was 540 min shorter when suspicion of stroke was already raised by the EMS (Figure 1). Thus, there was a marked reduction in system delay, that is time from dial 112 until initial report of CT scan and arrival in stroke unit. We also observed that most delays were much shorter if there were neurological deficits on the arrival of the EMS (Supplementary Table 1). Supplementary Table 2 shows the various delays in relation to whether there was an ‘acute stroke alert’.
3.3 Priority and clinical findings before arrival in hospital
Patients in whom there was an initial suspicion of stroke were given a higher priority at the dispatch centre, as well as in the ambulance (Table 2). In terms of neurological deficits before arrival in hospital, those in whom there was an initial suspicion of stroke had a higher mean value of mNIHSS; they more frequently had focal neurological deficits in their arms or legs (72.5% versus 19.5%); they more frequently had dysphasia (57.1% versus 14.0%). In contrast, patients with an initial stroke suspicion less frequently had a decreased level of consciousness (4.8% versus 10.0%).
| Total (n = 5467) | Suspicion of stroke (n = 4396) | No suspicion of stroke (n = 1071) | p-value | Difference between groups mean (95%CI) | |
|---|---|---|---|---|---|
| EMDC priority (57)a | |||||
| 1 | 3703 (68.4) | 3194 (73.5) | 509 (47.9) | ||
| 2 | 1640 (30.3) | 1125 (25.9) | 515 (48.5) | ||
| 3 | 67 (1.2) | 29 (0.7) | 38 (3.6) | <.0001 | |
| EMS priority (73) | |||||
| 1 | 2151 (39.9) | 1970 (45.4) | 181 (17.1) | ||
| 2 | 2640 (48.9) | 2016 (46.5) | 624 (59.0) | ||
| 3 | 603 (11.2) | 351 (8.1) | 252 (23.8) | <.0001 | |
| Neurological symptoms mNIHSS (2089) | |||||
| Median (Q1, Q3) | 4 (2, 11) | 5 (2, 12) | 2 (0, 6) | ||
| Mean ± SD | 7.3 ± 7.4 | 7.8 ± 7.5 | 4.4 ± 6.5 | .002 | 3.3 (2.6, 4.0) |
| mNIHSS | |||||
| 0–5 | 1877 (55.6) | 1496 (52.1) | 381 (74.9) | ||
| 6–14 | 912 (27.0) | 823 (28.7) | 89 (17.5) | ||
| ≥15 | 589 (17.4) | 550 (19.2) | 39 (7.7) | ||
| Focal neurologic deficits in arms or legs (622) | 3106 (64.1) | 2946 (73.2) | 160 (19.5) | <.0001 | |
| Dysphasia (694) | 2348 (49.2) | 2226 (57.1) | 122 (14.0) | <.0001 | |
| Not awake (90) | 314 (5.8) | 209 (4.8) | 105 (10.0) | <.0001 | |
| Vital signs | |||||
| Heart rate (beats/min) (143) | |||||
| Median (Q1, Q3) | 80 (70, 91) | 80 (70, 90) | 80 (70, 95) | ||
| Mean ± SD | 82.3 ± 18.0 | 81.8 ± 17.5 | 84.1 ± 20.1 | .004 | −2.23 (−1.04, −3.48) |
| Systolic blood pressure (mmHg) (171) | |||||
| Median (Q1, Q3) | 160 (140, 180) | 160 (140, 180) | 151 (133, 176) | ||
| Mean ± SD | 161.0 ± 30.1 | 162.2 ± 29.7 | 155.8 ± 31.3 | .002 | 6.45 (4.45, 8.55) |
| Oxygen saturation (%) (161) | |||||
| Median (Q1, Q3) | 96 (95, 98) | 96 (95, 98) | 96 (94, 98) | ||
| Mean ± SD | 95.5 ± 3.7 | 95.6 ± 3.2 | 95.0 ± 5.2 | .002 | 0.61 (0.35, 0.87) |
| Body temperature (ºC) (1060) | |||||
| Median (Q1, Q3) | 36.6 (36.2, 37.0) | 36.6 (36.2, 37.0) | 36.6 (36.2, 37.0) | ||
| Mean ± SD | 36.6 ± 0.7 | 36.6 ± 0.6 | 36.6 ± 0.8 | .92 | 0.003 (−0.044, 0.053) |
| Examinations | |||||
| ECG recorded (290) | 3183 (61.5) | 2635 (63.1) | 548 (54.9) | <.0001 | |
| Blood glucose recorded (996) | 4471 (81.8) | 3786 (86.1) | 685 (64.0) | <.0001 | |
| Level of blood glucose (mmol/L) | |||||
| Median (Q1, Q3) | 7.4 (6.3, 9.1) | 7.3 (6.2, 8.9) | 7.9 (6.7, 10.1) | ||
| Mean ± SD | 8.3 ± 3.4 | 8.1 ± 3.3 | 9.0 ± 4.0 | .002 | −0.93 (−0.65, −1.17) |
| Contact with hospital | |||||
| Contact with hospital (6) | 2731 (50.0) | 2697 (61.4) | 34 (3.2) | <.0001 | |
| Yes, with a neurologist on call (75) | 868 (16.1) | 851 (19.7) | 17 (1.6) | <.0001 | |
| Yes, with stroke coordinator (75) | 1359 (25.2) | 1339 (30.9) | 20 (1.9) | <.0001 | |
| Yes, acute stroke alarm (331) | 1441 (26.5) | 1435 (32.9) | 6 (0.6) | <.0001 | |
| Direct admission to stroke unit (37) | 859 (15.8) | 847 (19.4) | 12 (1.1) | <.0001 | |
Note
- For categorical variables n (%) is presented.
- Abbreviations: CI, confidence interval; ECG, electrocardiogram; EMDC, emergency medical dispatch centre; EMS, emergency medical service; mmol/L, millimoles per litre; mNIHSS, modified national institutes of health stroke scale; ºC, degree Celsius; Q1, quartile 1; Q3, quartile 3; SD, standard deviation.
- a Missing information.
There were small, most likely clinically irrelevant differences between the two groups in terms of heart rate, systolic blood pressure and oxygen saturation on EMS admission. An ECG was recorded and blood glucose was measured more frequently if there was an initial suspicion of stroke. A prenotification was made in 61.4% of cases when there was an initial suspicion of stroke versus 3.2% if there was no suspicion. Among patients in whom stroke was recognized, 19.4% were directly admitted to a stroke unit versus 1.1% when it was not recognized.
3.4 Findings and treatment in hospital
The level of consciousness was slightly higher when there was an initial suspicion of stroke and NIHSS was higher among these patients (mean 7.8 versus 4.4) (Table 3). Thrombolysis was given to 15.8% of patients and thrombectomy was performed in 4.5% of patients when a stroke was recognized early versus 1.7% and 0.7%, respectively, when it was not.
|
Total (n = 5467) |
Suspicion of stroke (n = 4396) |
No suspicion of stroke (n = 1071) |
Differences between groups mean (95%CI) | |
|---|---|---|---|---|
| Level of consciousness at admission (1187)a | ||||
| 1 | 3448 (80.6) | 2853 (80.8) | 595 (79.7) | |
| 2 | 614 (14.3) | 519 (14.7) | 95 (12.7) | |
| 3 | 218 (5.1) | 161 (4.6) | 57 (7.6) | |
| NIHSS (2089) | ||||
| Median (Q1, Q3) | 4 (2, 11) | 5 (2, 12) | 2 (0, 6) | |
| Mean ± SD | 7.3 ± 7.4 | 7.8 ± 7.5 | 4.4 ± 6.5 | 3.3 (2.6, 4.0) |
| Thrombolysis (1155) | ||||
| Yes | 573 (13.3) | 560 (15.8) | 13 (1.7) | |
| Thrombectomy (1151) | ||||
| Yes | 165 (3.8) | 160 (4.5) | 5 (0.7) | |
Note
- For categorical variables n (%) is presented; Level of consciousness at admission 1: Awake, 2: Drowsy or confused responsive to stimulation, 3: Unconscious.
- Abbreviations: CI, confidence interval; NIHSS, national institutes of health stroke scale; Q1, quartile 1; Q3, quartile 3.
- a Missing information.
3.5 Unadjusted and adjusted mortality after three months
Unadjusted mortality did not differ between the patients in whom a stroke was recognized early and those in whom it was not (Table 4). However, unadjusted mortality was much higher among women than among men, in the elderly as compared with younger patients and among patients who had various neurological deficits on the arrival of the EMS as compared with those who had not. When adjusting for these factors, the risk of death within three months was significantly higher among patients in whom stroke was not recognized on the arrival of the EMS (odds ratio 1.66; 95% confidence interval 1.19–2.32; p = .003).
| N (%) of event | Univariable | p-value | Multivariablea | p-value | |
|---|---|---|---|---|---|
| OR (95%CI) | OR (95%CI) | ||||
| Suspicion of stroke | |||||
| No | 205 (19.1) | 1.05 (0.89–1.25) | .55 | 1.66 (1.19–2.32) | .003 |
| Yes | 807 (18.4) | ||||
| Focal neurologic deficits in arms or legs | |||||
| No | 163 (9.4) | ||||
| Yes | 623 (20.1) | 2.43 (2.02–2.91) | <.0001 | ||
| Dysphasia | |||||
| No | 257 (10.6) | ||||
| Yes | 457 (19.5) | 2.04 (1.73–2.40) | <.0001 | ||
| Decreased consciousness | |||||
| Awake | 786 (15.5) | ||||
| Not awake | 194 (61.8) | 8.80 (6.92–11.18) | <.0001 | ||
| Sex | |||||
| Male | 353 (15.5) | ||||
| Female | 458 (22.0) | 1.54 (1.32–1.80) | <.0001 | ||
| Age in years | |||||
| <73.6 | 115 (7.9) | ||||
| 73.6–84.2 | 240 (16.5) | ||||
| >84.2 | 456 (31.4) | 2.01 (1.85–2.19) | <.0001 | ||
- Abbreviations: CI, confidence interval; OR, odds ratio.
- a Adjusted for focal neurological deficits in arms or legs, dysphasia, decreased consciousness, sex and age.
3.6 Place of living, activities three months after onset of symptoms
Three months after stroke onset, 56.0% lived in their own homes without any home care service (Supplementary Table 3). There was no statistical difference between the two groups.
More than half of all patients were able to move outdoors and indoors without help, with no major difference between the two groups.
The need for assistance with toilet visits was reported in 23.3% in overall terms.
Difficulty reading was reported in 19.3% in overall terms and difficulty swallowing was reported in 9.4%, with no major difference between the two groups. Difficulty writing was reported in 27.3% in overall terms and difficulty talking was reported in 18.9%, with higher figures among patients with an initial suspicion of stroke for both.
Always or often feeling depressed was reported in 17% in overall terms and slightly more often among patients with no initial suspicion of stroke.
About 75% of all patients assessed their general health as very good or relatively good, with no major difference between the two groups.
About 40% of all patients felt tired always or often, with no major difference between the two groups. There was no major difference on the Modified Ranking Scale between the two groups.
3.7 Association between early suspicion of stroke and clinical presentation and EMS performance
In terms of clinical presentation, there was an association between initial suspicion of stroke and focal neurological deficits in arms or legs, dysphasia, consciousness, heart rate, systolic blood pressure and levels of blood glucose on arrival of the EMS (Table 5). In terms of EMS performance, there was an association between suspicion of stroke and the priority given at the dispatch centre as well as by the EMS clinician and contact taken with hospital already at the scene.
| N (%) of event | Univariable | p-value | Multivariable | p-value | |
|---|---|---|---|---|---|
| Suspicion of stroke OR (95%CI) | Suspicion of stroke OR (95%CI) | ||||
| Clinical findings | |||||
| Focal neurologic deficits in arms or legs (622)a | |||||
| No | 1077 (61.9) | ||||
| Yes | 2946 (94.8) | 11.32 (9.39–13.63) | <.0001 | 8.92 (6.67–11.94) | <.0001 |
| Dysphasia (694) | |||||
| No | 1675 (69.1) | ||||
| Yes | 2226 (94.8) | 8.17 (6.68–9.99) | <.0001 | 4.89 (3.61–6.63) | <.0001 |
| Decreased consciousness (90) | |||||
| Awake | 4113 (81.2) | ||||
| Not awake | 209 (66.6) | 0.46 (0.36–0.59) | <.0001 | 0.35 (0.15–0.86) | .022 |
| Heart rate (beats/min) (143) | |||||
| <74 | 1461 (81.7) | ||||
| 74–86 | 1398 (81.1) | ||||
| >86 | 1425 (78.6) | 0.94 (0.90–0.97) | .0003 | 0.93 (0.86–1.00) | .039 |
| Systolic blood pressure (mmHg) (171) | |||||
| <149 | 1344 (76.1) | ||||
| 149–170 | 1442 (81.8) | ||||
| >170 | 1483 (83.9) | 1.08 (1.05–1.10) | <.0001 | 1.06 (1.01–1.11) | .011 |
| Oxygen saturation (%) (161) | |||||
| <96 | 1639 (79.9) | ||||
| 96–97 | 1537 (82.5) | ||||
| >97 | 1093 (78.6) | 1.04 (1.02–1.06) | <.0001 | 1.03 (0.99–1.08) | .14 |
| Level of blood glucose (mmol/L) (996) | |||||
| <6.7 | 1339 (88.8) | ||||
| 6.7–8.3 | 1270 (85.0) | ||||
| >8.3 | 1177 (80.1) | 0.94 (0.92–0.96) | <.0001 | 0.94 (0.92–0.97) | .0001 |
| EMS performance | |||||
| EMDC priority | |||||
| 1 | 3194 (86.3) | ||||
| 2 | 1125 (68.6) | ||||
| 3 | 29 (43.3) | 0.35 (0.31–0.40) | <.0001 | 0.63 (0.49–0.81) | .0003 |
| ECG recorded (290) | |||||
| No | 1544 (77.4) | ||||
| Yes | 2635 (82.8) | 1.40 (1.22–1.61) | <.0001 | 0.86 (0.65–1.12) | .26 |
| EMS priority | |||||
| 1 | 1970 (91.6) | ||||
| 2 | 2016 (76.4) | ||||
| 3 | 351 (58.2) | 0.35 (0.32–0.40) | <.0001 | 0.75 (0.57–0.98) | .033 |
| Contact with hospital (6) | |||||
| No | 1693 (62.0) | ||||
| Yes | 2697 (98.8) | 48.59 (34.34–68.74) | <.0001 | 28.98 (16.89–49.73) | <.0001 |
- Abbreviations: CI, confidence interval; EMDC, emergency medical dispatch centre; EMS, emergency medical service; mmol/L, millimoles per litre; OR, odds ratio.
- a Missing information.
4 DISCUSSION
4.1 The five main messages from this study are as follows
- In more than 80% of patients who called for an ambulance due to an acute stroke, the disease was already recognized by the EMS clinician at the scene.
- The early recognition of stroke by the EMS clinician was associated with a markedly reduced time from dialling 112 until arrival at the stroke unit.
- The early recognition of stroke by the EMS clinician was associated with a reduced time from dialling 112 until a preliminary report from a CT scan.
- The reduction in delays as described above was limited to the chain of care that took place after arrival in hospital.
- The adjusted risk of death during three months was 66% higher when stroke was not recognized on the arrival of the EMS.
Our finding that more than 80% of patients with a stroke were recognized by the EMS clinician is somewhat higher than previously reported from the same region.5 These data suggest that EMS clinicians have improved the accuracy of their assessments. It is only possible to speculate about the possible mechanisms behind this finding. The introduction of NIHSS in the prehospital workup may be a contributory factor. Another contributory factor may be increased awareness of and education on new treatment facilities in hospital, together with a lowered threshold for telephone consultation. In a previous study from Spain, a brief education intervention was associated with improved EMS stroke recognition, hospital prenotification and faster tissue plasminogen activator (tPA) delivery. Gains were primarily observed immediately following education and were not sustained through the provision of performance feedback to paramedics.9 Similar findings were made by others.10
It was previously reported that the sensitivity of the detection of stroke in the emergency department (ED) by physicians was 82%.5 It is therefore possible to argue that EMS clinicians are as skilful as ED physicians in the early recognition of stroke. One reason may be that both the EMS clinician and the physician in the ED use a structured scale for the identification of stroke, although there must be some suspicion from the start. It is also possible to speculate that a well-educated prehospital emergency nurse has a better ability to recognize a stroke than paramedics. The finding that the median age and the distribution of gender were both similar among the patients who were recognized early and those that were not indicates that the early recognition of stroke is not dependent on age or gender.
A previous literature review showed that, across 21 studies, 26% of patients who had a stroke that was not recognized by the EMS accounted for between 2% and 52% of stroke presentations not identified in the prehospital setting.11
We found that the recognition of stroke by EMS clinicians was associated with a surprisingly extensive reduction in the delay to admission to a stroke unit. Previous studies of the impact of prenotification from the ambulance to the hospital on delays suggest much smaller time benefits.8 Twenty per cent of the stroke patients who were recognized early were directly admitted to a stroke unit. It has previously been reported that direct admission from the ambulance to a stroke unit was associated with a shortening of the delay to admission to a ward of about four hours.12
The time to the preliminary report from a CT scan was also shorter among patients who had an early recognition of stroke. However, the mean time from dialling 112 until the preliminary report was also relatively long among patients who were recognized early. Moreover, not all these patients had an ‘acute stroke alert’. As a result, the need for an early CT scan will most probably also differ within the group of patients who have an early recognition of stroke, since not all of them are candidates for reperfusion therapy. Furthermore, the distance for the ambulance will most probably influence the total system delay (from calling for the EMS until a CT scan).
Three further studies were conducted between 2010 and 2019 and they showed that EMS-recognized strokes had faster door-to-CT times (34.6 vs 84.7 min; p < .001), but this did not translate into higher rates of thrombolysis delivery, although there was a trend in this direction.13-15
Only in 60% of the patients in whom the EMS clinician suspected a stroke was the hospital prenotified. We are not aware of the mechanisms behind this finding. Possible explanations may include lack of awareness of the opportunity to make a prenotification among some EMS clinicians or refraining to contact the hospital when the suspicion of stroke was vague. In some of the hospitals, the stroke unit was not available for direct admission during the night. Other studies have reported 70% prenotification in cases where stroke was recognized.15
Blood glucose was measured more frequently among patients in whom stroke was recognized early, despite the fact that these patients were more often fully awake. This finding suggests that the EMS clinicians became more active on the scene when a stroke was suspected. The observation of more ECGs being recorded in this subgroup was in agreement with a hypothesis of this kind.
Almost all the patients who were revascularized were found in the group of stroke patients that was recognized early. The few revascularized patients who were identified from the group of patients who were not recognized early had a further delay of more than one hour until the start of treatment as compared with the patients who were recognized early. These findings suggest that the prehospital recognition of stroke is more or less a prerequisite for an optimal early chain of care.
Mortality and activities of daily living three months after the onset of symptoms were fairly similar, regardless of the early recognition of stroke. This finding must be related to the fact that the two groups were not strictly comparable. The cerebral area at risk on admission to hospital differed markedly since neurological deviations were much more frequent among the stroke patients who were recognized early. So, when adjusting for these differences at baseline, our results indicated a higher risk of death when stroke was not recognized by the EMS clinician.
4.2 Clinical implications
In four of five patients with a final diagnosis of stroke who are examined by an EMS clinician, the disease will be recognized before arrival at hospital in the study area. This proportion may improve even further. Recent experiences from Gothenburg suggest a recognition rate of 84%.16 The early recognition of stroke will have a major impact on the subsequent chain of care and is more or less a prerequisite for an optimal early chain of care.
There is an ongoing discussion in Sweden about whether EMS clinicians should perform a diagnostic workup before arrival in hospital or whether they should focus on the description of different symptoms and not think so much about possible aetiologies behind the symptoms. Our results strongly advise that, at least in terms of stroke, it is an advantage if the disease is already recognized in the prehospital setting.
4.3 Limitations
There was missing information in a large number of variables, which limits the internal validity of the data. It is possible to argue about the choice of factors that were adjusted for. We included age and sex, which is common practice. We furthermore adjusted for neurological signs and the level of consciousness on the arrival of the EMS, which differed markedly between the two groups. There were no major differences regarding previous history or other clinical signs on EMS arrival, and, as a result, no further covariate was included in the adjusted model.
We studied only one region of Sweden in which about one sixth of the Swedish population live. In terms of external validity, we do not know whether our results could be extrapolated to other parts of the country which include more rural areas. Furthermore, one EMS organization was excluded since we did not receive permission by their operation manager to include them in the study. However, the impact on delays was mainly limited to in hospital delay and geographical aspects should therefore play a minor role. Our results can most likely not be extrapolated to other parts of the world where health care may differ in many respects.
The results deal with prehospital care that took place in 2013–2015, which is a limitation, particularly with regard to the use of thrombectomy, which has increased in the last few years. However, with regard to the primary endpoints, there is no reason to assume that things have changed during the last few years.
It is possible to argue that the proportion of patients who are available for thrombolysis and thrombectomy should be much higher than reported in this study. However, it was recently reported that, even if the competence level is very high on the scene, the proportion of patients with a suspicion of stroke who receive thrombectomy will still be as low as 6.6%,17 a figure which does not differ markedly from our result. However, we only looked at patients who had a finally confirmed diagnosis of stroke, which gives higher percentage values than if all the patients with an initial suspicion of stroke are considered, regardless of the final diagnosis.
About 10% of the patients had a final diagnosis indicating uncertain stroke type. This is surprising since in principle all patients underwent a brain CT scan. Most likely the majority of these cases were ischaemic strokes that were misdiagnosed. However, we preferred to report them as they were reported in the hospital case records since information from brain CT scan was not available.
Finally, it can be argued that the difference in times between the two groups may be explained not only by the early recognition of the disease but also by the fact that there was a clear difference in the occurrence and severity of neurological symptoms between the two groups, which probably influenced the chain of care.
5 CONCLUSION
Among patients with a stroke in Region Västra Götaland in Sweden who called for an ambulance, more than 80% were already recognized in the prehospital setting. The early recognition of stroke was associated with a markedly shorter time to arrival at the stroke unit and to the delivery of the preliminary report on the brain CT scan, a higher rate of direct admission to the stroke unit and a much higher rate of treatment with thrombolysis and thrombectomy. Finally, the early recognition of stroke was associated with a lower risk of death during the first three months after the onset of the disease.
ACKNOWLEDGEMENT
We thank Bengt Bengtsson and Nils Gunnar Pehrsson for help with statistical evaluation.
CONFLICT OF INTEREST
The authors have no commercial associations or sources of support that might pose a conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on reasonable request to the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




