The atherosclerotic cardiovascular disease risk score is a reliable tool to identify patients with arteriogenic erectile dysfunction
Abstract
Background
The atherosclerotic cardiovascular disease risk score is a validated algorithm predicting an individual's 10-year risk of developing acute cardiovascular events (cardiovascular disease). Patients who suffer from arteriogenic erectile dysfunction are susceptible to developing cardiovascular disease in the future.
Objectives
To apply the atherosclerotic cardiovascular disease score at a homogenous cohort of men with erectile dysfunction undergoing a dynamic penile colour Doppler duplex ultrasound and explore its predictive ability to identify patients with vasculogenic erectile dysfunction at colour Doppler duplex ultrasound.
Materials and methods
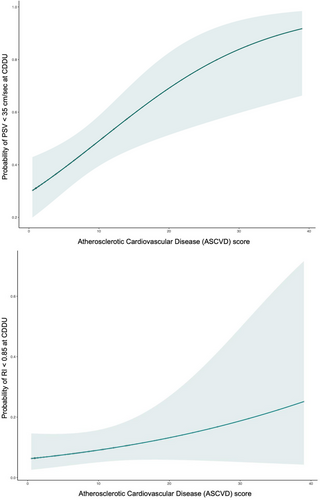
Complete data of 219 patients undergoing colour Doppler duplex ultrasound were analysed. All patients completed the International Index of Erectile Function. The atherosclerotic cardiovascular disease score and Charlson comorbidity index were applied to the entire cohort. Patients were divided into those with normal vs. pathological parameters at colour Doppler duplex ultrasound. Descriptive statistics were used to explore differences between the two groups. Logistic regression models tested the potential role of atherosclerotic cardiovascular disease to predict arteriogenic and/or venogenic erectile dysfunction. Local polynomial smoothing models graphically displayed the probability of pathological colour Doppler duplex ultrasound parameters at different atherosclerotic cardiovascular disease scores.
Results
Overall, arteriogenic erectile dysfunction and venous leakage were diagnosed in 88 (40.2%) and 28 (12.8%) patients respectively. The median (interquartile range) atherosclerotic cardiovascular disease score was 7.7 (3.9–14). Patients with pathologic colour Doppler duplex ultrasound were older (59 vs. 54 years, p < 0.001), had higher Body Mass Index (26.5 vs. 25.6 kg/m2, p = 0.04), more comorbidities (Charlson comorbidity index ≥ 1) (76.5% vs. 54.4%, p = 0.002) and higher median atherosclerotic cardiovascular disease scores (9.95 vs. 7, p = 0.005), respectively. At logistic regression analysis, a higher atherosclerotic cardiovascular disease risk score was independently associated with arteriogenic erectile dysfunction at colour Doppler duplex ultrasound (odds ratio: 1.03, 95% confidence interval: 1.01–1.08, p = 0.02) after adjusting for Body Mass Index, physical activity, alcohol consumption and severe erectile dysfunction.
Discussion
As vasculogenic erectile dysfunction may precede by some years the onset of acute cardiovascular diseases, the rigorous identification of patients with deficient cavernosal arterial blood flow, would definitely allow the implementation of earlier and more effective cardiovascular prevention strategies in men with erectile dysfunction.
Conclusions
The atherosclerotic cardiovascular disease risk score represents a reliable tool to identify patients with arteriogenic erectile dysfunction in everyday clinical practice.
1 INTRODUCTION
Erectile dysfunction (ED) is defined as the inability to achieve or sustain a sufficient erection for satisfactory sexual intercourse.1 Compelling evidence has accumulated over the years regarding the relevant interconnection between vasculogenic ED and serious cardiovascular diseases (CVD).2-5 In this context, it has been demonstrated that the persistence of commonly recognised vascular risk factors (e.g. smoking, arterial hypertension, hyperglycaemia, hypercholesterolemia, etc.) may uniformly affect blood vessels thus resulting in endothelial dysfunction, tunica media thickening and flow-limiting stenosis.6-8 Overall, smaller blood vessels such as cavernosal arteries are more susceptible to endothelial damage, which can occur at levels that are already damaging larger vessels such as the coronary arteries of the heart.2 As such, it has been widely established that vasculogenic ED can precede even by almost 5 years of coronary artery disease (CAD) onset. In fact, it is crucial from a clinical perspective to identify patients with ED who are most in need of personalized preventive cardiological strategies.2, 7 The American College of Cardiology (ACC) and the American Heart Association (AHA) guidelines suggest using a validated tool to predict an individual's 10-year risk of developing acute CAD, namely the atherosclerotic cardiovascular disease (ASCVD) risk score.9-11 Likewise, the diagnostic use of the dynamic colour Doppler duplex ultrasound (CDDU) has been suggested to better study the sonographic anatomy of the corpora cavernosa (CC) along with arterial blood flow and patency of veno-occlusive mechanisms, thus giving additional benefits in terms of better decision-making over ED management work-up.12-15 As such, CDDU measurements are informative for diagnosing vasculogenic ED with objective radiological findings.16-18 Since patients with vasculogenic ED are more likely to develop future CAD, we aimed to i) apply the ASCVD score at a homogenous cohort of men undergoing dynamic penile CDDU throughout ED diagnostic work-up; and, ii) explore its predictive ability to identify patients with arteriogenic and venogenic ED at CDDU.
2 MATERIALS AND METHODS
Data from the last 274 men seeking first medical help for ED as their primary and only complaint undergoing CDDU at a single tertiary academic centre were analysed. Of those, 219 (79.9%) men had available data and eligibility criteria for ASCVD calculation. Eligible criteria for ASCVD calculation were: i) individuals aged 40–79 years old; and, ii) available data on smoking, arterial hypertension, hypertension treatment, cholesterol level, diabetes mellitus and ethnicity (white-European population). All subjects were assessed via a detailed medical history including data on health-significant comorbidities as scored using the Charlson comorbidity index (CCI).19-21 Body mass index (BMI; kg/m2) and waist circumference (cm) were measured for each patient. Clinical data were collected as reported: hypertension, defined by the measurement of the arterial systolic pressure ≥ 140 mm/Hg and/or arterial diastolic pressure ≥ 90 mm/Hg, or by the daily use of one or more antihypertensive drugs22; hypercholesterolaemia, defined according to ESC guidelines as low-density lipoprotein cholesterol level of 190 mg/dl or higher23; and, type 1 or 2 diabetes mellitus, according to the definition of ESC-EASD guidelines.24 Additionally, data on patients’ subjective responses after initial treatment with PDE5i were collected. Data on recreational habits, including smoking history, alcohol consumption and physical activity (defined as at least 2 self-reported physical exercise sessions per week per individual) were also comprehensively investigated. Total testosterone and luteinising hormone levels were also measured in every patient. Moreover, all patients were invited to complete the International Index of Erectile Function (IIEF) at the first clinical assessment; ED severity was classified according to Cappelleri's criteria.25 Furthermore, all patients compiled the Beck's Inventory for Depression (BDI), with clinical depression defined as a BDI score ≥ 17.26, 27 Lower urinary tract symptoms were assessed using the International Prostate Symptom Score (IPSS).28 All patients underwent CDDU after intracavernosal injection of 20 μGr of PGE1 (Alprostadil).29, 30 Both peak systolic velocity (PSV) and the resistivity index (RI) were assessed bilaterally at 5 and 20 min after alprostadil injection. A PSV < 35 cm/s was used as a threshold to define penile cavernosal arterial insufficiency. A RI of < 0.85 was used to define the presence or coexistence of penile veno-occlusive dysfunction. Hence, pathological CDDU was defined as the presence of PSV < 35 cm/s and/or RI < 0.85. A mean value between the two sides of the corpora cavernosa was considered for both PSV and RI. At the time of CDDU, each patient's initial assessment involved the manual calculation of their ASCVD score, which was performed to assess the patient's 10-year risk of experiencing cardiovascular events (e.g. myocardial infarction).11, 31, 32 Data collection followed the principles outlined in the Declaration of Helsinki. All patients signed an informed consent form agreeing to share their own anonymous information for other future studies. The study was approved by the local ethic committee (IRCCS OSR Prot. 2014 – Pazienti Ambulatoriali).
2.1 Statistical analysis
For the specific purpose of this study, we divided our cohort into two distinct groups, as follows: Group 1: patients with normal CCDU; and, Group 2: patients with pathologic parameters (PSV < 35 cm/s and /or RI < 0.85) at CCDU. Statistical analyses consisted of several steps. First, medians and interquartile ranges or frequencies and proportions were reported for continuous or categorical variables, respectively. Mann-Whitney and Chi-square tests were used to compare the statistical significance of differences in the distribution of continuous or categorical variables between groups (normal CCDU vs. pathologic CCDU), respectively. Second, univariable, and multivariable logistic regression models were fitted to assess potential independent association with PSV < 35 cm/s at CDDU (i.e. arteriogenic ED). Exploratory analyses were initially applied to all variables and variables were then retained when deemed clinically significant. In this regard, the selection of variables in our logistic regression model was not solely based on their statistical significance, but also on their clinical relevance. As such, these variables could provide important clinical insights and help to explain the observed associations between other variables and the outcome. Third, univariable linear regression models tested the association between CDDU parameters (mean PSV and mean RI) with patients’ clinical characteristics, lifestyle habits and baseline ASCVD score. Lastly, local polynomial regression models graphically explored the probability of having PSV < 35 cm/sec and RI < 0.85 at CDDU at different ASCVD scores. All statistical tests were two-sided with a significance value set at 0.05. The analyses were conducted using R (2019), a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria.
3 RESULTS
Table 1 displays the socio-demographic and clinical characteristics of the whole cohort of patients, along with those of patients with normal CDDU (Group 1) vs. those with pathological CCDU (Group 2). Of all, 119 (54.3%) had normal CDDU and 100 (45.7%) had pathologic parameters at CDDU. Overall, Group 2 patients were older (p < 0.001), and had higher BMI (p = 0.04), greater waist circumference (p = 0.005) and higher cholesterol levels (p = 0.04) compared to Group 1 patients. Moreover, Group 2 patients depicted higher rates of comorbidities (i.e. CCI ≥ 1) (p = 0.002) and a higher median ASCVD score (p < 0.005) compared to Group 1 patients. No other differences were detected between the groups (Table 1).
| Variable | Whole Cohort | Normal CDDU | Pathologic CDDU††† | p-Value |
|---|---|---|---|---|
| Number of patients, No. (%) | 219 (100) | 119 (54.3) | 100 (45.7) | |
| Age (years), median (IQR) | 57 (50–63) | 54 (49–60) | 59 (53–65) | <0.001 |
| BMI (Kg/m2), median (IQR) | 26.1 (23.4–27.9) | 25.6 (23.2–27.3) | 26.5 (24.1–28.8) | 0.04 |
| Waist circumference (cm), median (IQR) | 98.5 (91–105) | 97 (87.5–102) | 101 (94–108) | 0.005 |
| CCI ≥ 1, No. (%) | 121 (64.3) | 56 (54.4) | 65 (76.5) | 0.002 |
| Regular physical activity, No. (%) | 113 (51.6) | 60 (50.4) | 53 (53) | 0.3 |
| Alcohol consumption ≥ 1L/week, No. (%) | 148 (67.6) | 82 (68.9) | 66 (66) | 0.1 |
| Smoking, No. (%) | 0.08 | |||
| No | 143 (65.3) | 70 (58.8) | 73 (73) | |
| Ex-smoker/Yes | 51 (23.3) | 32 (26.9) | 19 (19) | |
| Patient's response to PDE5i, No. (%) | 85 (38.8) | 45 (37.8) | 40 (40) | 0.2 |
| Arterial Hypertension, No. (%) | 75 (34.2) | 32 (26.9) | 43 (43) | 0.03 |
| Mean systolic pressure (mmHg), median (IQR) | 120 (120–135) | 120 (120–130) | 120 (120–135) | 0.02 |
| Arterial Hypertension therapy, No. (%) | 74 (33.8) | 31 (26.1) | 43 (43) | 0.02 |
| Type 1/2 diabetes mellitus, No. (%) | 25 (11.4) | 11 (9.2) | 14 (14) | 0.2 |
| Cholesterol levels (mg/dl), median (IQR) | 192 (168.3–211.3) | 181 (162.5–206) | 195 (174.3–216) | 0.04 |
| High-density lipoprotein (mg/dl), median (IQR) | 50 (44.9–55.3) | 50 (47–56) | 50 (41–54) | 0.06 |
| tT (ng/mL), median (IQR) | 4.8 (3.7–6.3) | 4.9 (3.9–6.4) | 4.6 (3.4–6.2) | 0.3 |
| LH (ng/mL), median (IQR) | 4.1 (2.9–5.8) | 4 (2.8–5.3) | 4.5 (2.9–6.3) | 0.2 |
| IPSS—Total, median (IQR) | 6 (3–9) | 5 (3.8) | 7 (3–10) | 0.2 |
| IPSS—QoL, median (IQR) | 1 (0–3) | 1 (0–3) | 1 (0–2) | 0.8 |
| BDI, median (IQR) | 6 (3–13) | 7 (3–13) | 5 (3–11) | 0.3 |
| BDI ≥ 17, No (%) † | 13 (5.9) | 8 (6.7) | 5 (5) | 0.4 |
| Erectile dysfunction severity (as for IIEF-EF) †† | ||||
| Normal EF, No. (%) | 7 (3.2) | 6 (5) | 1 (1) | 0.4 |
| Mild ED, No. (%) | 25 (11.4) | 14 (11.8) | 11 (11) | 0.8 |
| Mild-to-moderate ED, No. (%) | 48 (21.9) | 20 (16.8) | 28 (28) | 0.9 |
| Moderate ED, No. (%) | 66 (30.1) | 37 (31.1) | 29 (29) | 0.8 |
| Severe ED, No. (%) | 73 (33.3) | 42 (35.3) | 31 (31) | 0.1 |
| Cardiovascular drugs, No. (%) | 10 (4.6) | 1 (0.8) | 9 (9) | 0.07 |
| Anti-diabetics, No. (%) | 25 (11.4) | 11 (9.2) | 14 (14) | 0.2 |
| Diuretics, No. (%) | 2 (0.9) | 0 (0) | 2 (2) | 1 |
| Antidepressants, No. (%) | 19 (8.7) | 9 (7.7) | 10 (10) | 0.2 |
| Antihypertensives, No. (%) | 75 (34.2) | 32 (26.9) | 43 (43) | 0.03 |
| CDDU parameters ††† | ||||
| Mean PSV (cm/sec), median (IQR) | 40.8 (29.8–50.8) | 50 (43.1–55.3) | 29.1 (22.1–34.5) | <0.001 |
| Mean RI, median (IQR) | 1 (0.99–1) | 1 (1–1) | 1 (0.8–1) | 0.001 |
| Arteriogenic ED (PSV < 35 cm/s) | 88 (40.2) | 0 (0) | 88 (88) | <0.001 |
| Venogenic ED (RI < 0.85) | 28 (12.8) | 0 (0) | 28 (28) | <0.001 |
| Mixed ED (PSV < 35 cm/s + RI < 0.85) | 99 (45.2) | 0 (0) | 99 (99) | <0.001 |
| ASCVD score, median (IQR) | 7.7 (3.9–14) | 7 (3.6–12.1) | 9.95 (5.5–14.7) | 0.005 |
- Keys: IQR: interquartile range; BMI: Body Mass Index; CCI: Charlson Comorbidity Index; PDE5-i: Phosphodiesterase 5 inhibitor; tT: total testosterone; IPSS: International Prostatic Symptoms Score; IPSS Total: total score; QoL: Quality of Life; IIEF: International Index of Erectile Function; EF: Erectile Function domain; CDDU: dynamic Color Doppler Duplex Ultrasound; PSV: peak systolic velocity; RI: resistance index; ASCVD: Atherosclerotic Cardiovascular Disease score.
- † Clinically significant depression was defined as BDI ≥ 17.
- †† Erectile function severity according to Cappelleri's criteria (defining; normal EF as an IIEF-EF > 26; mild as an IIEF-EF of 26-22 mild-to-moderate as an IIEF-EF of 21-17; moderate as an IIEF-EF of 16-11; and severe ED as an IIEF-EF < 11).
- ††† Pathological penile Doppler parameters considered as i) PSV < 35 cm/sec arteriogenic ED, ii) RI < 0.85 venogenic ED and, iii) PSV < 35 + RI < 0.85 mixed ED.
Table 2 displays both the univariable and multivariable (MVA) logistic regression analyses showing independent associations with arteriogenic ED at baseline. At MVA, a higher ASCVD score (odds ratio: 1.03; 95% confidence interval: 1.01–1.08, p = 0.03) was independently associated with arteriogenic ED at CDDU, after adjusting for severe ED (i.e. IIEF-EF < 11), regular physical activity, BMI, and alcohol consumption > 1 L/week.
| UVA | MVA | |||
|---|---|---|---|---|
| Variable | OR (95% CI) | p-Value | OR (95% CI) | p-Value |
| ASCVD score† | 1.05 (1.02–1.10) | 0.006 | 1.03 (1.01–1.08) | 0.02 |
| Severe ED (IIEF-EF < 11) | 1.18 (0.65–2.13) | 0.6 | 1.11 (0.57–2.13) | 0.2 |
| BMI | 1.02 (0.98–1.06) | 0.4 | 1.01 (0.93–1.11) | 0.8 |
| Regular physical exercise | 0.83 (0.51–1.34) | 0.5 | 0.82 (0.42–1.61) | 0.6 |
| Alcohol ≥ 1L/wk | 1.02 (0.58–1.8) | 0.9 | 0.83 (0.42–1.61) | 0.9 |
- Keys: ASCVD: atherosclerotic cardiovascular disease score; ED: erectile dysfunction; IIEF-EF: International Index of Erectile Function—Erectile Function domain; CCI: Charlson Comorbidity Index; BMI: Body Mass Index.
- † We did not adjust our MVA logistic model for age, smoking, arterial hypertension, diabetes, and total cholesterol as all these parameters are included in the ASCVD score.
- †† Erectile function severity according to Cappelleri's criteria (defining; normal EF as an IIEF-EF > 26; mild as an IIEF-EF of 26-22 mild-to-moderate as an IIEF-EF of 21-17; moderate as an IIEF-EF of 16-11; and severe ED as an IIEF-EF < 11).
Table 3 shows the univariable linear regression analysis (UVA) estimating the association between CDDU parameters (mean PSV and mean RI) with patients’ characteristics, lifestyle habits and baseline ASCVD score. At UVA, patients with higher mean PSV were more likely to be younger (Coeff: −0.44, p < 0.001), to have less comorbid conditions (Coeff: - 3.5, p < 0.01), higher cholesterol levels (Coeff: 0.08, p = 0.02), higher high-density lipoprotein levels (Coeff: 0.39, p < 0.001) and lower ASCVD scores (Coeff: −0.45, p = 0.03). Likewise, patients with higher mean RI were more likely to be younger (Coeff: −0.12, p = 0.01).
| Variable | UVA CDDU—mean peak systolic velocity (cm/s) Coeff (SE) |
p-Value | UVA CDDU—mean resistance index Coeff (SE) |
p-Value |
|---|---|---|---|---|
| Age | −0.44 (0.10) | <0.001 | −0.12 (0.05) | 0.01 |
| Physical exercise | 1.17 (2.12) | 0.5 | 0.16 (0.81) | 0.8 |
| BMI | −0.02 (0.16) | 0.8 | 0.03 (0.06) | 0.6 |
| Waist circumference | −0.01 (0.02) | 0.4 | 0.06 (0.01) | 0.6 |
| CCI | −3.5 (1.44) | 0.01 | −1.87 (1.37) | 0.1 |
| High-density lipoprotein | 0.39 (0.11) | <0.001 | −0.02 (0.04) | 0.6 |
| Total cholesterol | 0.08 (0.03) | 0.02 | 0.01 (0.02) | 0.5 |
| ASCVD | −0.45 (0.15) | 0.03 | −0.04 (0.06) | 0.5 |
| tT | 0.34 (0.31) | 0.2 | −0.06 (0.12) | 0.6 |
| BDI | 0.12 (0.17) | 0.4 | 0.12 (0.07) | 0.09 |
- Keys: CDDU: dynamic Color Doppler Duplex Ultrasound; SE: standard error; BMI: Body Mass Index; CCI: Charlson Comorbidity Index; ASCVD: atherosclerotic cardiovascular disease score; tT: total testosterone; BDI: Beck's Inventory for Depression.
Figures 1 graphically display the probability of reporting PSV < 35 cm/s and RI < 0.85 at CDDU at different ASCVD scores (locally weighted scatterplot smoothing curves). The probability of reporting PSV < 35 cm/s at CDDU increases with higher ASCVD scores.
4 DISCUSSION
The latest diagnostic approach for ED in practical settings emphasizes the essential need to obtain a comprehensive patient history that includes lifestyle and recreational habits, which may have a detrimental impact on erectile function.1, 21, 33, 34 This holds even more relevance considering that ED per se may be an alarming bell of overall men's health.20, 21, 35 Moreover, laboratory tests and the use of validated questionnaires may help the physician to better identify the primary aetiology (e.g. primary organic vs. primary psychogenic ED) and to quantify its severity, thus offering a more tailored treatment strategy.1, 27, 36 Thereof, the more simple and clinically reliable investigation at first assessment, the easier and more effective the management work-up of men with ED. In the present study, we found that applying the ASCVD risk score—which is a reliable tool to predict an individual's 10-year risk of major cardiovascular events11, 32 – may be an effective strategy to select those patients with arteriogenic ED at CDDU, therefore potentially further reducing the need for a second level, minimally-invasive diagnostic tool, which has been indicated in ED men non-responders to oral traditional therapies and/or among those needing more in-depth cardiovascular risk estimation.37 In this context, it emerges of clinical importance that the higher the ASCVD scores, the more severe the cavernosal arteriogenic impairment, thus suggesting an even more thoughtful cardiological investigation and risk stratification.7, 38 More in detail, the American College of Cardiology/American Heart Association Task Force on Practice Guidelines highlighted how the initial classification of individuals is based on their estimated risk level, with those having a 10-year ASCVD risk of less than 5% being considered as having low risk, while those falling in the range of 5%–7.5% are regarded as having borderline risk. Individuals with a risk of 7.5%–20% are classified as having intermediate risk, while those with a risk equal to 20% or higher are categorized as high risk. Hence, if an individual is identified as high-risk, statin therapy should be strongly recommended based on risk alone. Conversely, subjects classified as having low risk do not benefit from statin therapy and should instead focus on adopting healthy habits for cardiovascular prevention.39 In this regard, the higher the score the higher the severity of endothelial dysfunction and atherosclerosis; as such, Figure 1 depicts this paradigm (i.e. the higher the ASCVD score the higher the probability of having arteriogenic ED). Overall, epidemiological surveys have shown that ED prevalence has been estimated to be around 19.2% with a proportional increase with advancing age (up to 53.4%) being mostly identified as organic ED.36, 40 Accordingly, although one in nine patients who present with ED in practical settings may exhibit criteria suggestive of primary psychogenic ED, most patients with ED warrant a thorough examination for primary organic ED in the current clinical context.41 As such, most men with organic ED have a vascular aetiology or at least a vascular component fostering their ED.41, 42 In this context, the use of CDDU plays a significant role in the assessment of penile structure and vasculature.43 In addition, CDDU has gained a substantial role to detect patients at higher risk of developing future peripheral vasculopathy and CAD.44, 45 This has been demonstrated over the last decade by correlating the compliance of penile cavernosal arteries and the patency of veno-occlusive mechanisms with the onset of future vascular events.44-46 Therefore, we investigated the role of ASCVD score in a homogenous cohort of men complaining of ED and submitted to CDDU, with the specific aim to test its reliability in identifying patients with arteriogenic and venogenic ED at CDDU. Overall, we found that almost 50% of patients with ED have a pathological CDDU. Moreover, men with pathological CDDU findings were older, had higher BMI, larger waist circumference, a higher baseline mean arterial systolic pressure, higher levels of serum high-density lipoprotein and a greater number of comorbidities at baseline according to CCI scores as compared with those patients with normal parameters at CDDU. Interestingly enough, patients with pathological CDDU depicted higher ASCVD scores compared to those with normal CDDU. Likewise, the ASCVD score emerged to be independently associated with arteriogenic ED at first clinical assessment, after adjusting for BMI, severe ED (IIEF < 11), regular physical activity, and alcohol consumption. Accordingly, patients better scoring at CDDU were more likely to be younger, to exercise more and to have lower ASCVD scores. More in detail, the probability of reporting PSV < 35 cm/s at CDDU increased with higher ASCVD scores further strengthening from a biopathology standpoint the common ground fostering vasculogenic ED and underlying vascular comorbid conditions. As such, the current findings support the notion that the ASCVD risk score is a reliable predictor for detecting patients with true arteriogenic ED in practical settings, potentially justifying or even obviating the routine use of CDDU as a secondary diagnostic tool. Moreover, as vasculogenic ED anticipates the onset of acute CVD in some men, the rigorous detection and stratification of patients with arteriogenic ED would lead to earlier and more effective tailored cardiovascular prevention strategies in this specific sub-group of patients.
Despite to the best of our knowledge, this is the first study to apply the ASCVD score as a potential tool to identify patients with arteriogenic ED as well as patients with a high risk of developing CVD in the real-life setting, our study is certainly not devoid of limitations. First, although current analyses have been conducted in a homogeneous, same-ethnicity cohort of men seeking first medical help for new-onset ED, this was a single centre-based cross-sectional study, raising the possibility of selection biases; consequently, this may possibly impact the generalisability of our results. Thereof, wider cohort studies across different institutions and populations are needed to validate our findings. Second, our study did not prospectively include follow-up over time with a control group of healthy men without ED at baseline. Third, being CDDU an operator-dependent diagnostic test, the inter-agreement variability might have affected the actual interpretation of current findings; however, all diagnostic procedures were performed by a group of highly experienced physicians, each with more than 100 procedures already done at the time of patient assessment. Fourth, notwithstanding ASCVD is intended to provide guidance for healthcare professionals in the United States, the ASCVD risk calculator might not be suitable to address the risk of future CVD events in the currently considered study population. Despite this limitation, healthcare professionals may certainly implement the ASCVD as a starting point throughout the management work-up to estimate CVD risk even among white-European patients. Of clinical relevance, ASCVD accuracy may be reduced in our study population, and additional factors, such as family history and lifestyle factors, should be comprehensively considered when assessing an individual's CVD risk. Ultimately, it is up to the healthcare professional to use their clinical judgment and expertise to determine the best approach to assessing and managing CVD risk in their patients, considering the individuals’ unique medical history, risk factors, and preferences. As a last limitation, while a power analysis is an important statistical tool for assessing the reliability of study results, the absence of a power analysis does not necessarily preclude concerns about the validity of the study findings. As a whole, we consider that our results may allow a more reliable tailoring of those patients who eventually need a CDDU done over their ED diagnostic work-up in the everyday clinical practice.
5 CONCLUSION
The ASCVD risk score can be considered an effective and reliable tool to identify patients with true arteriogenic ED in everyday clinical practice. As vasculogenic ED may precede by some years the onset of acute CVD, the rigorous identification of patients with the deficient cavernosal arterial flow would definitely lead to implement earlier and more effective cardiovascular prevention strategies among men with ED.
AUTHOR CONTRIBUTIONS
Conception and design: Alessandro Bertini, Edoardo Pozzi, Paolo Capogrosso, and Andrea Salonia
Acquisition of data: Alessandro Bertini, Edoardo Pozzi, Giuseppe Fallara, Luigi Candela, Antonio Costa Federico Belladelli, Francesco Lanzaro, Simone Cilio, Christian Corsini, and Alessia D'arma
Analysis and interpretation of data: Paolo Capogrosso, Andrea Salonia, Edoardo Pozzi, and Giuseppe Fallara
Drafting the article: Edoardo Pozzi, Alessandro Bertini, Andrea Salonia, and Paolo Capogrosso
Revision for intellectual content: Andrea Salonia, Paolo Capogrosso, and Francesco Montorsi
Final approval of the completed article: Andrea Salonia and Francesco Montorsi
Open Research
DATA AVAILABILITY STATEMENT
Research data are not shared.