A helpful approach to organ donation: From end-of-life care to effective organ transplantation
To the Editor
We read with interest the report by Witjes et al regarding the influence of end-of-life care on organ donor potential.1 The report promotes innovation in management of potential organ donors outside the ICU, particularly in patients admitted to the emergency department (ED) with acute devastating brain injury (DBI) and imminent brain death.
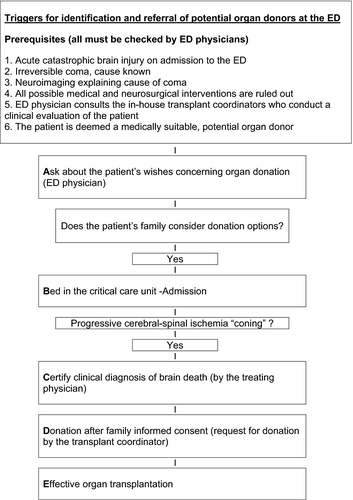
Hospital EDs play a key role in organ donation for transplantation.2-5 Five years ago we implemented a novel approach for organ donation in the ED (Figure 1). This approach is routinely used in patients with acute DBI on admission to the ED. These patients must have clinical evidence of an irreversible cause of coma of known etiology, without confounding circumstances. Our approach comprises five steps. First, these patients are assessed by ED physicians, consultant neurologists and consultant neurosurgeons, and all possible therapeutic interventions are considered. Second, once all possible treatment options have been ruled out, an ED physician consults the in-house transplant coordinators who conduct a clinical bedside evaluation to determine whether the patient is a suitable donor. Third, if the patient is considered suitable for donation, an ED physician explains the grave prognosis to the family and discusses end-of-life decisions, including the patient′s right to organ donation. An ED physician asks relatives directly about the patient's donation wishes and if favourable, the patient is transferred to a bed in a critical care unit (usually an ICU). The availability of a bed in a critical care unit is guaranteed in all these cases. Once the patient is in a critical care unit and following brain herniation, brain death is certified. The diagnosis of brain death is made by the attending physician. The attending physician informs the family of the patient's death and the transplant coordinator later requests consent for donation. Fourth, family informed consent for donation is obtained. Fifth, effective organ transplantation takes place.
From December 1st 2013 to July 31st 2016, 12 patients were admitted to the ED with acute DBI. Our approach was implemented. All patients were assessed by ED physicians, neurologists and neurosurgeons, and all possible therapeutic options were considered but ruled out. All patients were evaluated and accepted as potential organ donors. In accordance with the patients’ families, all patients were admitted to critical care units. All patients evolved to brain death. Eleven (91.7%) died within 72 hours after hospital admission. The patients’ families gave written informed consent for organ donation in all cases. From these 12 brain-dead donors we performed 26 organ transplants (17 kidneys and nine livers). The results achieved in terms of organ donation for transplantation were highly satisfactory, representing 19% of our total pool of actual organ donors and 19% of our global activity of kidney and liver transplants. In our experience, the key to success of the donation process is the close teamwork and collaboration of ED physicians and transplant coordinators as standard practice in the ED. We consider this novel approach could be widely adopted in order to increase the likelihood of organ donation for transplantation.
ACKNOWLEDGMENTS
We thank Ana Manzano for useful comments during the writing up of this paper.
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.




