Graft-Derived CCL2 Increases Graft Injury During Antibody-Mediated Rejection of Cardiac Allografts
Abstract
The pathogenic role of macrophages in antibody-mediated rejection (AMR) remains unclear. Monocyte chemoattractant protein-1 (MCP-1/CCL2) is a potent chemotactic factor for monocytes and macrophages. The current studies used a murine model of AMR to investigate the role of graft-derived CCL2 in AMR and how macrophages may participate in antibody-mediated allograft injury. B6.CCR5−/−/CD8−/− recipients rejected MHC-mismatched WT A/J allografts with high donor-reactive antibody titers and diffuse C4d deposition in the large vessels and myocardial capillaries, features consistent with AMR. In contrast, A/J.CCL2−/− allografts induced low donor-reactive antibody titers and C4d deposition at Day 7 posttransplant. Decreased donor-reactive CD4 T cells producing interferon gamma were induced in response to A/J.CCL2−/− versus WT allografts. Consequently, A/J.CCL2−/− allograft survival was modestly but significantly longer than A/J allografts. Macrophages purified from WT allografts expressed high levels of IL-1β and IL-12p40 and this expression and the numbers of classically activated macrophages were markedly reduced in CCL2-deficient allografts on Day 7. The results indicate that allograft-derived CCL2 plays an important role in directing classically activated macrophages into allografts during AMR and that macrophages are important contributors to the inflammatory environment mediating graft tissue injury in this pathology, suggesting CCL2 as a therapeutic target for AMR.
Abbreviations
-
- AMR
-
- antibody-mediated rejection
-
- CFSE
-
- carboxyfluorescein succinimidyl ester
-
- IFN-γ
-
- interferon gamma
-
- MCF
-
- mean channel fluorescence
-
- MST
-
- median survival time
-
- NK
-
- natural killer
-
- PCR
-
- polymerase chain reaction
-
- TNFα
-
- tumor necrosis factor alpha
Introduction
The detected incidence of antibody-mediated graft rejection in solid organ recipients is increasing. Acute humoral rejection occurs in almost 7% of renal transplant patients and is also prevalent in cardiac and lung graft recipients 1-4. Donor-specific antibodies directly mediate graft tissue injury through binding to graft endothelium, the initial target of the antibodies 5-7. Complement activation following this binding is an important effector function contributing to antibody-mediated tissue injury of allografts by stimulating endothelial cells to produce many inflammatory mediators including adhesion molecules, growth factors, cytokines, and chemokines, that function to provoke leukocyte infiltration and activation within the graft tissue including the typical neutrophil and macrophage infiltration that is observed by histopathologic evaluation of antibody-mediated rejection (AMR) 1, 3, 4, 7-10.
Macrophages are key components of innate immunity that differentiate from circulating monocytes migrating into tissues during inflammatory responses 11-13. Macrophages are stimulated within tissue inflammatory sites to express many functions that contribute to tissue injury including production of tumor necrosis factor alpha (TNFα), IL-1β and IL-6 and chemokines inducing further leukocyte infiltration and activation. However, many cell populations produce these inflammatory mediators during tissue inflammation and the contribution of macrophages to graft tissue injury induced during AMR remains unclear. Monocyte chemoattractant protein-1 (MCP-1/CCL2) is a potent chemotactic factor that directs monocyte and macrophage infiltration into tissue sites of inflammation 14, 15. Protein and gene expression of CCL2 and its receptor CCR2 are up-regulated in allografts during acute cell-mediated rejection in animal models and in clinical transplants 16-20. CCL2 neutralization promotes modest prolongation of cardiac allograft survival in rodent models, suggesting that CCL2 directed monocyte/macrophage graft infiltration might contribute to cell-mediated allograft rejection 21. In support of this, cell-mediated rejection of complete MHC-mismatched cardiac allografts survival was delayed almost 2 weeks in CCL2-deficient versus WT recipients; however, prolonged survival was not observed when CCL2-deficient allografts were transplanted to WT recipients 17. While these latter studies suggest a role for CCL2, particularly recipient-derived CCL2, in T cell–mediated rejection of allografts, the role and impact of graft-derived CCL2 in directing the typical macrophage infiltration observed during AMR remains poorly understood.
We previously observed marked increases in serum levels of donor-reactive antibody induced to complete MHC-disparate heart and kidney allografts in B6.CCR5−/− recipients 22, 23. These dysregulated antibody responses in B6.CCR5−/− recipients appear more quickly and have 15- to 50-fold higher titers than those observed in WT C57BL/6 recipients. The consequence of this increased antibody response is AMR accompanied by intense C4d/C3d deposition in the large vessels and capillaries of the allograft. We further developed this model by generating CCR5−/−/CD8−/− mice to exclude the contribution of CD8 T cells in rejection 24. CCR5−/−/CD8−/− allograft recipients produce high titers of donor-specific antibody that induce expression of CCL2, perforin, FasL, and CCL5 in allografts and intense infiltration of neutrophils and macrophages during the AMR. In the present study, we tested the role of graft-derived CCL2 in AMR by investigating rejection of complete MHC-mismatched A/J.CCL2−/− hearts by B6.CCR5−/−/CD8−/− recipients.
Materials and Methods
Mice
C57BL/6 (B6, H-2b), A/J (H-2a) and DBA/1 (H-2q) mice were obtained from the National Cancer Institute (Frederick, MD). B6.CCR5−/−, B6.CD8−/− and B6.CCL2−/− mice were obtained from the Jackson Laboratory (Bar Harbor, ME). B6.CCR5−/− and B6.CD8−/− mice were crossed to generate B6.CCR5−/−/CD8−/− mice and the B6.CCL2−/− mice were backcrossed to the A/J background for 12 generations. All experiments used 8- to 12-week-old male mice and were approved by the Institutional Animal Care and Use Committee at the Cleveland Clinic.
Cardiac transplantation and recovery
Heterotopic intra-abdominal cardiac transplantation was performed following the method of Corry et al 25. Briefly, the donor aorta and pulmonary artery were anastomosed to the recipient abdominal aorta and inferior vena cava in the peritoneal cavity. Graft survival was monitored daily by abdominal palpation and graft rejection confirmed visually by laparotomy. At the time of cardiac graft recovery, 10 mL of Ringer's solution was flushed into the recipient circulatory system. Graft pieces and recipient spleens were removed and were snap-frozen in liquid nitrogen or placed in media for digestion and analyses of graft-infiltrating cells. Some allograft recipients were given 250 µg of anti-CD154 mAb (MR-1; BioXCell, West Lebanon, NH) or control rat IgG (Sigma–Aldrich, St. Louis, MO) intraperitoneally on Days 0 and 1 posttransplant.
Flow cytometry
Absolute numbers of graft-infiltrating neutrophils, macrophages, dendritic cells and T cells were determined using a modified method of that reported by Afanasyev et al 24, 26, 27. Following digestion of allografts to prepare single cell suspensions, cell aliquots were stained with fluorochrome-conjugated anti-CD45 mAb and cell type-specific antibodies and analyzed by flow cytometry. Total numbers of each leukocyte population were determined by: (the total number of leukocytes counted) × (% of the leukocyte population counted in the CD45+ cells)/100. These data are reported as number of each leukocyte population/mg graft tissue. In some experiments, graft-infiltrating CD45+F4/80+ cells (macrophages) were sorted on a FACSAria II (BD Biosciences, San Jose, CA).
RNA purification and quantitative reverse transcription polymerase chain reaction
Snap-frozen grafts were crushed, homogenized, and RNA was isolated using RNeasy Fibrous Tissue Kits (QIAGEN, Valencia, CA). RNA was isolated from sorted macrophages using RNeasy Kit (QIAGEN). RNA was reverse transcribed using the High-Capacity cDNA Archive Kit (Applied Biosystems, Foster City, CA) and polymerase chain reaction (PCR) was performed using commercially available reagents, probes and a 7500 Fast Real-Time thermocycler (Applied Biosystems). Target gene expression was quantitated using the ΔΔCT method and normalized to Mrpl32 gene expression and naïve A/J heart mRNA was used as the calibrator.
Immunohistochemistry
Heart grafts were recovered at designated times posttransplant and cross-sections of the center of the graft paraffin-embedded/methanol and acetic acid fixed or frozen sections were prepared for histology and immunohistochemistry analyses as previously described 24, 28.
Donor-specific antibody detection and quantitation by flow cytometry
Flow cytometry to detect and quantitate donor-specific antibodies in nonrecipient and cardiac graft recipient serum was performed as previously reported 22-24. Briefly, aliquots of donor strain thymocyte suspensions were incubated with serial dilutions of recipient sera taken prior to transplant and at several time points between transplantation and rejection. After 30 min, the cells were washed and suspended in staining buffer (Dulbecco's PBS with 2% FCS/0.2% NaN3) containing FITC-conjugated goat anti-mouse IgG, Fcγ fragment-specific mAb (Jackson Immunoresearch, West Grove, PA). The mean channel fluorescence (MCF) of each dilution of each serum sample was determined and the dilution that returned the MCF to the level observed when A/J thymocytes were stained with a 1:4 dilution of normal WT serum was divided by two and reported as the titer.
Quantitation of donor-reactive CD4 T cells
Priming of donor-specific T cells to interferon gamma (IFN-γ) and IL-4 producing cells was quantified by ELISPOT assays as previously described 24, 27, 28. The total number of spots per well was quantified using an ImmunoSpot Series 2 Analyzer (Cellular Technology Ltd., Shaker Heights, OH).
In vitro proliferation assays
Dendritic cells were purified from spleens of A/J and A/J.CCL2−/− mice using the Mouse CD11c Positive Selection Kit (Stem Cell Technologies, Seattle, WA). Responder T cells were purified from spleens of naïve B6 and B6.CCR5−/−/CD8−/− mice using the Mouse T Cell Enrichment Kit (Stem Cell Technologies). Responder T cells were labeled with carboxyfluorescein succinimidyl ester (CFSE) and cultured 1:1 with the dendritic cells in complete RPMI (RPMI + 10% FBS + 1% L-glutamine) for 96 h. Following culture, cells were recovered and proliferation of responder T cells was determined using flow cytometry.
Statistics
All data were analyzed using GraphPad Prism Pro (GraphPad Software, Inc., San Diego, CA). Kaplan–Meier analysis was performed for graft survival. Log-rank testing was performed to determine differences in survival data and Mann–Whitney nonparametric test was used to determine significance throughout as indicated with p < 0.05 being considered a significant difference between groups.
Results
CCL2-deficient cardiac allografts have prolonged survival and reduced cell infiltration into the allografts
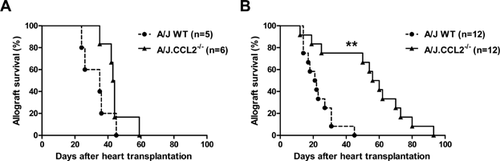
To begin to investigate the role of allograft-derived CCL2/MCP-1 in AMR of complete MHC-mismatched heart allografts, groups of B6.CCR5−/−/CD8−/− mice received heart grafts from WT A/J or CCL2-deficient A/J donors. B6.CCR5−/−/CD8−/− recipients acutely rejected WT A/J allografts within 7–10 days whereas A/J.CCL2−/− allograft survival was modestly but significantly longer (median survival time [MST]: A/J, Day 8 vs. A/J.CCL2−/−, Day 10; p < 0.01; Figure 1A). In contrast, WT C57BL/6 recipients rejected A/J and A/J.CCL2−/− allografts at similar times (Figure 1B). Allografts were recovered from B6.CCR5−/−/CD8−/− recipients on Day 7 posttransplant. Prepared sections stained with hematoxylin and eosin indicated marked increases in the intensity of leukocyte infiltration into A/J grafts when compared to infiltration into A/J.CCL2−/− grafts (Figure 1C).
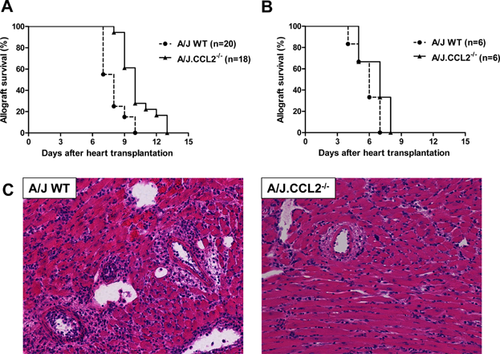
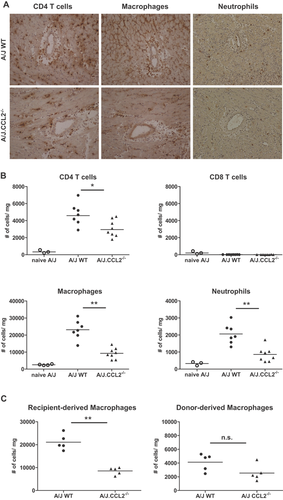
Immunohistochemical staining of allograft sections revealed marked increases in CD4 T cell, macrophage and neutrophil infiltration into A/J versus A/J.CCL2−/− allografts (Figure 2A). Numbers of allograft-infiltrating leukocyte populations were directly quantified on Day 7 posttransplant by flow cytometry analyses. Consistent with the histological analyses, the numbers of allograft-infiltrating CD4 T cells, macrophages and neutrophils were significantly decreased in A/J.CCL2−/− versus the A/J allografts (Figure 2B). The CD45+ cells in the WT A/J and A/J.CCL2−/− cardiac allografts were stained with antibodies to detect Kk+ and Kk− cells in the F4/80+ population. The numbers of donor-derived, Kk+ macrophages were similar in the WT and CCL2-deficient allografts whereas the number of recipient-derived, Kk− macrophages was reduced almost 2.5-fold in the CCCL2-deficient versus WT allografts (Figure 2C). Equivalent results were observed staining the cells with F4/80 and anti-I-Ab and there was no difference in the level of MHC Class II expression on the recipient-derived macrophages infiltrating WT A/J and A/J.CCL2−/− cardiac allografts (data not shown).
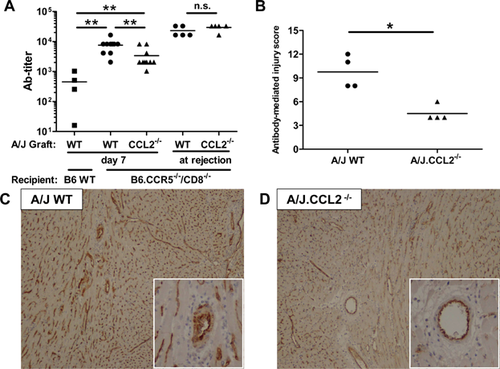
CCL2-deficient cardiac allografts induce decreased donor-reactive antibody responses
Our previous studies had indicated the induction of high levels of donor-reactive antibody in B6.CCR5−/− recipients of complete MHC-mismatched cardiac and renal allografts 22, 23. To evaluate donor-reactive antibody production in B6.CCR5−/−/CD8−/− recipients of WT A/J versus A/J.CCL2−/− allografts, serum was collected from groups of recipients on Day 7 posttransplant and donor-reactive IgG antibody titers compared (Figure 3A). In contrast to the low donor-reactive titers observed in WT C57BL/6 recipients of A/J heart allografts, high titers of donor-reactive IgG were observed in B6.CCR5−/−/CD8−/− recipients of A/J allografts, but these titers were significantly decreased in A/J.CCL2−/− allograft recipients. When compared at the time of allograft rejection, however, serum titers of donor-reactive IgG were virtually identical in B6.CCR5−/−/CD8−/− recipients of WT A/J or A/J.CCL2−/− allografts. Consistent with the antibody titer analysis, A/J allografts recovered from CCR5−/−/CD8−/− recipients on Day 7 posttransplant had intense C4d deposition in the large vessels and myocardial capillaries and this deposition was decreased in A/J.CCL2−/− allografts (Figure 3C and D). When stained sections from four allografts in each group were evaluated for C4d diffuseness and intensity and for endothelial cell swelling in arteries, capillaries and veins, established pathological features of AMR of heart grafts 29, in a blinded manner, the level of injury was markedly and significantly decreased in the CCL2-deficient cardiac allografts (Figure 3B).
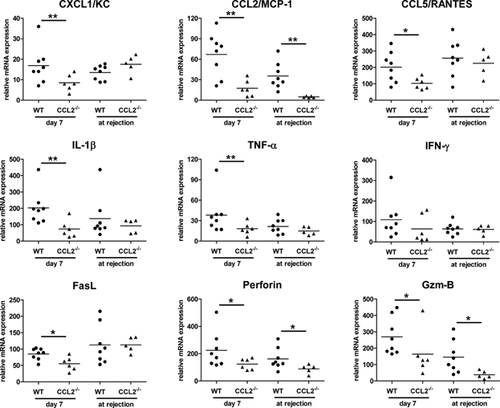
Intragraft cytokine and chemokine mRNA expression in cardiac allografts
To investigate potential factors underlying antibody-mediated injury of A/J and A/J.CCL2−/− allografts, grafts were recovered from B6.CCR5−/−/CD8−/− recipients on Day 7 posttransplant and expression levels of mRNA encoding inflammatory mediators were compared (Figure 4). There was no difference in the expression of IFN-γ in A/J and A/J.CCL2−/− allografts on Day 7 posttransplant but expression of the neutrophil chemoattractant CXCL1 and the proinflammatory cytokines TNFα and IL-1β were significantly reduced in the CCL2-deficient allografts. Furthermore, the expression levels of CCL5, FasL and perforin mRNA were significantly increased in WT A/J versus A/J.CCL2−/− allografts, suggesting the induced expression of these genes was mediated by donor-reactive antibody and/or CD4 T cells induced in the B6.CCR5−/−/CD8−/− recipients during allograft rejection. When the expression of these genes was assessed in rejected A/J and A/J.CCL2−/− allografts, only expression of CCL2, perforin, and granzyme B were significantly decreased in A/J.CCL2−/− allografts versus WT A/J allografts.
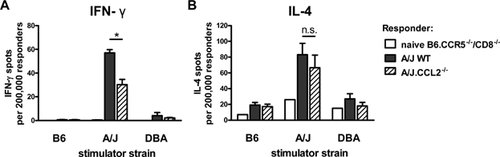
Allograft CCL2 deficiency decreases the development of donor-reactive CD4 T cells producing IFN-γ
To assess the impact of absent graft-derived CCL2 on the priming of donor-reactive T cells in B6.CCR5−/−/CD8−/− recipients, A/J or A/J.CCL2−/− cardiac allograft recipient spleen cell suspensions were prepared on Day 7 posttransplant and numbers of donor-reactive CD4 T cells producing IFN-γ and IL-4 were enumerated by ELISPOT assay (Figure 5). WT A/J cardiac allografts induced higher frequencies of donor-reactive CD4 T cells producing IFN-γ than did A/J.CCL2−/− allografts (p < 0.05). However, there was no significant difference in the numbers of donor-reactive CD4 T cells producing IL-4 induced in B6.CCR5−/−/CD8−/− recipients of A/J and A/J.CCL2−/− allografts.
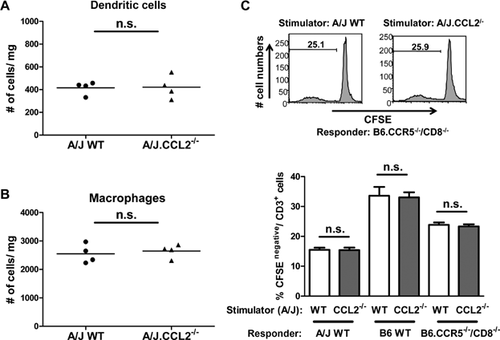
No detectable difference in dendritic cell and macrophage numbers or dendritic cell allostimulatory function in WT A/J and A/J.CCL2−/− hearts
The possibility of differences in the numbers and/or functions of alloantigen-presenting cell populations in the hearts of WT A/J versus A/J.CCL2−/− mice was considered as a potential underlying mechanism for the decreased donor-reactive antibody and CD4 T cell responses observed in B6.CCR5−/−/CD8−/− recipients of the A/J.CCL2−/− heart allografts. Hearts were recovered from naïve WT A/J and A/J.CCL2−/− mice, digested and stained with dendritic cell and macrophage-specific antibodies. Flow cytometry analyses of anti-CD45, anti-I-Ek and anti-CD11c mAb stained cells indicated no difference in the number of dendritic cells in the hearts of A/J and A/J.CCL2−/− (Figure 6A). Similarly, there was no difference in the number of CD45+F4/80+ macrophages in the A/J and A/J.CCL2−/− hearts. To investigate potential differences in the function of dendritic cells as alloantigen-presenting cells, dendritic cells purified from A/J or A/J.CCL2−/− spleens and CFSE-labeled T cells purified from naïve WT C57BL/6 or B6.CCR5−/−/CD8−/− mice were co-cultured for 96 h. There was no difference in the proliferation of CD3+ cells stimulated during culture of A/J and A/J.MCP-1−/− dendritic cells (Figure 6B).
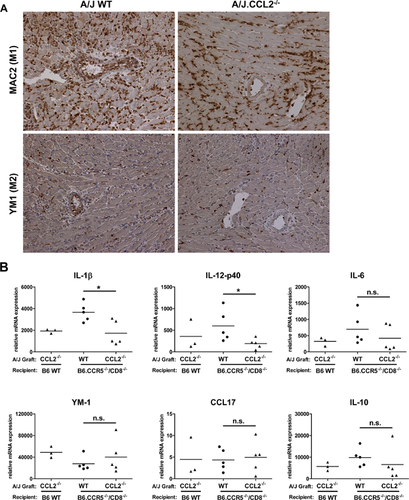
CCL2 deficiency reduces the number of macrophages expressing classically activated phenotypic markers
To investigate whether allograft CCL2 deficiency impacted the phenotype of graft-infiltrating macrophages, cardiac allografts were recovered from B6.CCR5−/−/CD8−/− recipients on Day 7 posttransplant and prepared sections were stained for immunohistochemical analysis using anti-MAC2 and anti-YM1 antibodies to detect classically activated and M2 macrophages, respectively (Figure 7A). WT A/J allografts showed intense infiltration of classically activated macrophages compared to A/J.CCL2−/− allografts. In contrast, there was no apparent difference in M2 macrophages in A/J and A/J.CCL2−/− allografts. To complement the histological analyses, graft-infiltrating macrophages were isolated by cell sorting of digested allografts on Day 7 posttransplant and mRNA expression of classically activated and M2 functional markers in the sorted macrophages was quantified by quantitative reverse transcription PCR (qRT-PCR) (Figure 7B). Consistent with the histology analyses, macrophages infiltrating A/J allografts expressed higher levels of IL-1β and IL-12 p40 (classically activated macrophage functional markers) compared to those infiltrating A/J.CCL2−/− allografts. In contrast, there was no difference in expression of YM1 and CCL17 (M2 phenotypic markers) and IL-10 (regulatory macrophage function) genes between macrophages infiltrating A/J and A/J.CCL2−/− allografts.
Increased efficacy of co-stimulation blockade in promoting the long-term survival of CCL2-deficient versus WT cardiac allografts
The decreased early injury observed in CCL2-deficient versus WT cardiac allografts in B6.CCR5−/−/CD8−/− recipients suggested that administration of co-stimulatory blockade might be more effective in promoting better outcome of the CCL2-deficient allografts during AMR. WT C57BL/6 and B6.CCR5−/−/CD8−/− allograft recipients were treated with 250 µg of anti-CD154 mAb on Days 0 and 1 posttransplant and survival of the allografts was monitored. While anti-CD154 mAb extended survival of WT A/J and A/J.CCL2−/− cardiac allografts in WT C57BL/6 recipients, there was no significant difference in survival between the two allograft groups (MST: WT A/J allografts, Day 35 vs. A/J.CCL2−/− allografts, Day 43.5, p = 0.183; Figure 8A), indicating no greater efficacy of the co-stimulatory blockade in prolonging CCL2-deficient allograft survival during cell-mediated rejection. In contrast, peri-transplant administration of anti-CD154 mAb was much more effective in prolonging survival of A/J.CCL2−/− versus WT allografts to AMR in B6.CCR5−/−/CD8−/− recipients (MST: WT A/J, Day 21.5 vs. A/J.CCL2−/−, Day 58, p < 0.01; Figure 8B).
Discussion
AMR is accompanied by the infiltration of neutrophils, macrophages, T cells and natural killer (NK) cells into the allografts. Studies of AMR in clinical transplantation report the presence of monocytes/macrophages in peritubular and glomerular capillaries in kidney grafts and in endomyocardial biopsies from heart grafts as a key diagnostic feature of AMR that correlates well with the presence of serum donor-specific antibodies and C4d deposition in the graft 10, 30. A recent update of the International Society for Heart & Lung Transplantation classification indicated CD68+ cells in biopsies among the key pathologic criteria for diagnosis of AMR in heart grafts 3. Despite recognition of macrophages in allografts during antibody-mediated injury, the role of macrophages in contributing to the inflammation and tissue injury during this pathology remains poorly understood.
The role of macrophages in contributing to graft tissue injury during acute cellular rejection of allografts has been investigated using many different approaches, including macrophage deletion by various strategies that may not always target only macrophages 11, 31, 32. CCL2 is produced by many cell types following inflammatory stimulation including endothelial and epithelial cells, vascular smooth muscle cells, fibroblasts and many leukocyte populations cells and is a key chemoattractant regulating the infiltration of monocytes/macrophages into inflammatory tissue sites 14, 15. On this basis, several studies have investigated the impact of CCL2- or its receptor CCR2-deficiency in cell-mediated rejection of islet or heart allografts 16-18. In this study, we investigated the potential role of the CCL2–CCR2 axis in a mouse model of AMR in order to gain insights into the contribution of macrophages to the inflammation and tissue injury developing during this rejection. This model utilizes mice deficient in both CD8 T cells and the expression of CCR5 as recipients of complete MHC-mismatched heart allograft donors with a targeted gene deletion in the monocyte/macrophage chemoattractant CCL2. CCR5 is expressed on many populations of CD4+FoxP3+ T regulatory cells, including those that regulate responses to infection, tumors and autoantigens 33-35. Our previous studies had demonstrated that CCR5−/− recipients have dysregulated antibody responses to heart and renal allografts and that the increased donor-specific antibody mediates rejection of the renal allografts 22, 23. The additional absence of CD8 T cells in B6.CCR5−/−/CD8−/− recipients obviates the contribution of these T cells to allograft injury 24. As shown in the current studies complete MHC-mismatched cardiac allograft rejection in B6.CCR5−/−/CD8−/− recipients is characterized by high production of donor-reactive antibody and intense C4d deposition in the myocardial capillaries accompanied by intense macrophage infiltration, characteristic histopathologic features of AMR. The macrophages in these allografts are primarily recipient-derived, of the classically activated phenotype, and express high levels of proinflammatory genes, indicating a key contribution of these leukocytes to the inflammation in the allograft during AMR. Such classically activated macrophages differentiate when exposed to IFNγ in concert with TNFα and produce IL-1, IL-6, IL-12 and IL-23, potent proinflammatory cytokines that can induce inflammation and tissue injury 11, 12, 36. M2, or alternatively activated, macrophages develop in response to IL-4 produced by T cells or granulocytes and may be involved in injury repair 11, 12, 36. Low and equivalent numbers of the M2 phenotype macrophages were observed in both WT and CCL2-deficient allografts at the time the WT grafts were being rejected.
We reasoned that the absence of CCL2 within the allograft should decrease monocyte/macrophage infiltration into allografts during AMR. This prediction was supported as CCL2-deficient allografts had significantly reduced recipient-derived macrophage infiltration as well other components of inflammation within the allografts. This decreased inflammation was most likely due to the threefold to fourfold decreases in donor-specific antibody titers observed in B6.CCR5−/−/CD8−/− recipients of the CCL2-deficient cardiac allografts at the time the WT allografts were rejected. Consequently, the survival of CCL2−/− A/J allografts was modestly but significantly longer than that of A/J WT allografts. However, 3–4 days later donor-specific antibody titers in B6.CCR5−/−/CD8−/− recipients of the CCL2-deficient cardiac allografts achieved the levels observed in recipients of rejecting WT allografts and the CCL2−/− allografts were rejected. These results suggest that a threshold level of donor-specific antibody is required to provoke the high levels of inflammation leading to rejection of the cardiac allografts. The decreased inflammation in the CCL2-deficient cardiac allografts also increased the efficacy of CD154-mediated co-stimulatory blockade in promoting enhanced survival of the allografts in the AMR but not the cell-mediated rejection model.
At or near the time of WT allograft failure, there is high expression of FasL, perforin, granzyme B and CCL5 in the grafts and these were significantly decreased in the CCL2-deficient allografts at that time. We had previously reported that graft expression of CCL5, FasL and perforin was associated with AMR of single MHC Class I disparate heart allografts 24. This expression was observed during AMR of the allografts in the B6.CCR5−/−/CD8−/− recipients as well as in allografts in RAG-1−/− recipients following transfer of donor-reactive serum. The source of this expression remains unclear but both cytolytic CD8 T cells and NK cells express these functions during viral infections. Recent studies by Hidalgo et al 37, 38 have indicated the expression of NK cell-derived genes during AMR in clinical renal grafts. Studies to test the presence and activities of NK cells in cardiac and renal allografts in the C57BL/6.CCR5−/−/CD8−/− recipient model of AMR are ongoing.
The decreased antibody titers induced in response to CCL2-deficient allografts on Day 7 posttransplant were accompanied by decreased priming of donor-reactive CD4 T cells producing IFN-γ. We considered the possibility that CCL2-deficient hearts had fewer resident dendritic cells or macrophages that accounted for the decreased alloimmune response. However, ex vivo analysis indicated that the number of interstitial macrophages and dendritic cells and the alloantigen stimulatory function of dendritic cells were equivalent in WT A/J and CCL2-deficient hearts. Although not directly tested, it seems unlikely that CCL2-deficient dendritic cells have defects in trafficking out of the graft and into the recipient spleen as donor-reactive T cell priming was induced and similar levels of donor-reactive CD4 T cells producing IL-4 were induced in response to WT and CCL2-deficient allografts. Furthermore, the donor-reactive antibody response is initiated through alloantigen presentation on recipient-derived antigen-presenting cells, including B cells. Potential mechanisms underlying the delay in achieving optimal titers of donor-reactive antibody include the impact of the decreased early inflammation within the allograft on the antibody response and the potential role of allograft-derived dendritic cell production of CCL2 during the alloimmune response. Several recent studies have indicated that early graft inflammation impacts the production of donor-reactive antibody 39, 40, and the decreased inflammation observed in the CCL2-deficient allografts would be consistent with this observation. Another potential mechanism underlying the decreased alloimmune response to CCL2-deficient grafts is that dendritic cell-derived CCL2 provides further enhancement for activation of T cells and accounts for the lower priming of IFN-γ producing CD4 T cells observed. These results are consistent with those of others indicating that dendritic cell production of CCL2 promotes antigen-reactive CD4 T cell differentiation to IFN-γ producing cells 41, 42.
Overall, the current studies demonstrate that allograft-derived CCL2 plays an important role in the magnitude of the alloimmune response elicited, in directing macrophage and other inflammatory cells into the allografts and in the development of donor-reactive antibody and vascular rejection. The intense macrophage infiltration that is observed during AMR is comprised of classically activated macrophages and these macrophages strongly contribute to the inflammation during this rejection. These results implicate CCL2 as a potential therapeutic target for AMR.
Acknowledgments
We thank the staff of the Cleveland Clinic Biological Resources Unit for excellent care of the animals used in this study. The authors thank Nina Dvorina for help with immunohistochemical staining and Anna Valujskikh and members of the Fairchild and Valujskikh lab for helpful comments during the course of this work. This work was supported by grants from the NIH (RO1 AI40459 and PO1 AI087586) to RLF.
Disclosure
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.