Bovine Pericardium Diaphragm Repair of Diaphragmatic Hernia After LVAD Explantation and Heart Transplantation
American Journal of Transplantation Images in Transplantation – Continuing Medical Education (CME)
Each month, the American Journal of Transplantation will feature Images in Transplantation, a journal-based CME activity, chosen to educate participants on current developments in the science and imaging of transplantation. Participants can earn 1 AMA PRA Category 1 Credit™ per article at their own pace. This month's feature article is titled: “Bovine Pericardium Diaphragm Repair of Diaphragmatic Hernia After VAD Explantation and Heart Transplantation.”
Accreditation and Designation Statement
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of Blackwell Futura Media Services, the American Society of Transplant Surgeons and the American Society of Transplantation. Blackwell Futura Media Services is accredited by the ACCME to provide continuing medical education for physicians. Blackwell Futura Media Services designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Statement of Need
Currently, the use of left ventricular assist devices (LVADS) for patients with advanced heart failure is growing to represent almost 30% of the heart transplant patient population. LVAD utilization will likely increase in the future as the number of critically ill patients waiting for an organ increases. The insertion and subsequent removal of these devices after a transplant procedure can lead to increasing rates of postsurgical complications such as postoperative bleeding, persistent pleural effusions and diaphragmatic hernia, which can present acute or insidious in nature. Therefore, it is important for clinicians to understand the anatomy involved when inserting these devices and how to recognize the possible surgical complications of a diaphragmatic hernia.
Purpose of Activity
To gain greater understanding of the technical aspects and possible complications of LVAD procedures to improve competence, prevent complications and ultimately improve patient outcomes with respect to diaphragmatic hernias.
Identification of Practice Gap
Many diaphragmatic hernias can be prevented by proper repair of the diaphragm during/after transplantation. Furthermore, the signs and symptoms of these hernias may not be readily apparent to clinicians at the time of transplant surgery.
Learning Objectives
Upon completion of this educational activity, participants will be able to:
- Identify and recognize the potential for complications in post-LVAD insertion, due to the creation of a diaphragmatic defect.
- Understand the anatomy involved in the insertion and removal of LVADs and how this relates to possible complications.
- Describe the possible symptoms of a diaphragmatic hernia such that all clinicians who care for transplant patients are able to recognize and evaluate the patient.
- Understand the need for prompt recognition of diaphragmatic hernias and the need for surgical correction to prevent further complications.
- Understand the risk of diaphragmatic hernia if repair of the diaphragm is not performed at the time of transplant.
Target Audience
This activity has been designed to meet the educational needs of physicians and surgeons in the field of transplantation, particularly cardiothoracic surgeons.
Disclosures
No commercial support has been accepted related to the development or publication of this activity. Blackwell Futura Media Services has reviewed all disclosures and resolved or managed all identified conflicts of interest, as applicable.
Editor-in-Chief
Allan D. Kirk, MD, PhD, FACS, has no relevant financial relationships to disclose.
Editors
Sandy Feng, MD, PhD, has no relevant financial relationships to disclose.
Douglas W. Hanto, MD, PhD, has no relevant financial relationships to disclose.
Authors
Kevin B. Ricci, BSE, Vincent C. Daniel, MD, Chittor Sai-Sudhakar, MD, and Robert Higgins, MD, have no relevant financial relationships to disclose.
ASTS Staff
Mina Behari, Director of Education, has no relevant financial relationships to disclose.
This manuscript underwent peer review in line with the standards of editorial integrity and publication ethics maintained by the American Journal of Transplantation. The peer reviewers have no relevant financial relationships to disclose. The peer review process for the American Journal of Transplantation is blinded. As such, the identities of the reviewers are not disclosed in line with the standard accepted practices of medical journal peer review.
Instructions on Receiving CME Credit
This activity is designed to be completed within an hour. Physicians should claim only those credits that reflect the time actually spent in the activity. This activity will be available for CME credit for twelve months following its publication date. At that time, it will be reviewed and potentially updated and extended for an additional twelve months.
Follow these steps to participate, answer the questions and claim your CME credit:
- Log on to https://www.wileyhealthlearning.com/ajt
- Read the learning objectives, target audience, and activity disclosures.
- Read the article in print or online format.
- Reflect on the article.
- Access the CME Exam, and choose the best answer to each question.
- Complete the required evaluation and print your CME certificate.
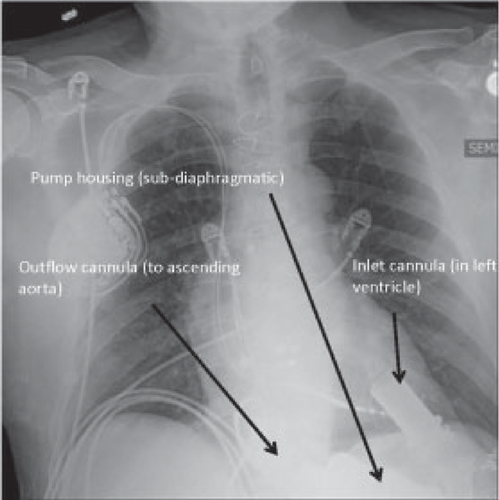
A 60-year-old male underwent a successful orthotropic heart transplant secondary to ischemic heart failure at our institution. He was bridged with a Heartmate II left ventricular assist device (LVAD) for a period of 2 years prior to an organ becoming available (Figure 1).
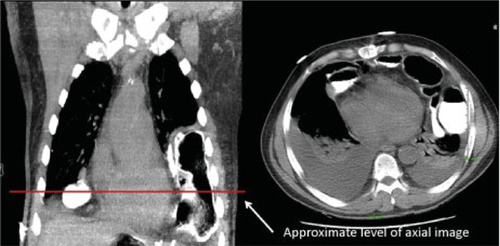
The patient had an uneventful removal of the LVAD, orthotopic heart transplant and postoperative recovery. He was discharged home 12 days following his operation. He returned 1 month later for a scheduled, outpatient endomyocardial biopsy complaining of shortness of breath, increased fatigue and intermittent epigastric abdominal pain. Subsequent fluoroscopy during his biopsy was concerning for possible abdominal contents in his chest. A computed tomography (CT) scan confirmed the presence of a large diaphragmatic hernia with multiple loops of bowel in his thoracic cavity (Figure 2).
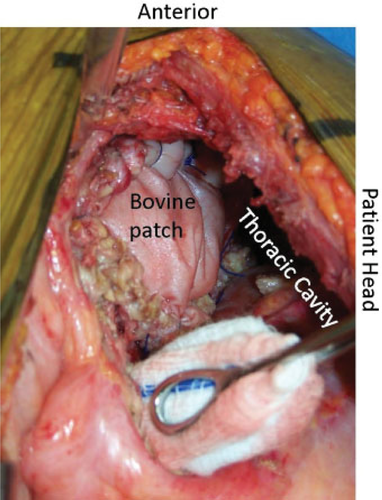
He was taken to the operating room for reduction of his abdominal contents and repair of his diaphragmatic defect. A seventh intercostal space left thoracotomy was performed and provided adequate exposure of the hernia and facilitated the reduction of the contents. At the time of transplantation, the diaphragmatic defect had been reapproximated with 0 monofilament absorbable sutures. After reduction of the hernia, it was evident that the sutures had pulled through the diaphragmatic tissue to cause a single 5 × 3 cm defect. Given the failure of the previous repair, the defect was closed using a bovine pericardium patch (Figure 3). Postoperative hospital course was unremarkable. The patient was discharged on regular diet, with no lingering symptoms on postoperative day 8.
-
K. B. Ricci1,*, V. C. Daniel2, C. Sai-Sudhakar1 and R. Higgins1
-
1. Division of Cardiac Surgery; 2. Division of Thoracic Surgery, Wexner Medical Center, The Ohio State University, Columbus, OH
-
*Corresponding author: Kevin B. Ricci, [email protected]
Questions
- Current surgical implantation of FDA-approved LVADs requires implantation through which body cavities or structures?
- Thoracic cavity alone
- Thoracic cavity and diaphragm
- Peritoneum
- Peritoneum and thoracic cavity
- Symptoms of trans-diaphragmatic hernia include:
- Abdominal pain, shortness of breath, fatigue, leukocytosis
- Shortness of breath and fatigue only
- Abdominal pain only
- Leukocytosis only
- The optimum approach to repair diaphragmatic defects after explantation of the LVAD for heart transplantation requires which of the following?
- No repair
- Primary repair of diaphragm
- Repair of diaphragm using synthetic patch material
- Repair of diaphragm using biological bovine pericardial material
- Which of the following is a benefit of repairing diaphragmatic defects at the time of heart transplantation in patients with LVADs?
- Decreased rate of herniation
- Increased rate of readmission
- Longer length of hospital stay
- Increased risk of bowel incarceration
- Decreased length of time to diagnosis of diaphragmatic hernia
To complete this activity and earn credit, please go to https://www.wileyhealthlearning.com/ajt