Learnings From the Front Line: Early Implementation Experiences of the Central Queensland Foot Hub Virtual Multidisciplinary Team Model-of-Care
ABSTRACT
Background
The ‘Central Foot Hub’ was operationalised in mid-February 2024 to provide multidisciplinary team (MDT) support from the Royal Brisbane and Women's Hospital (RBWH) to three hospital and health services (HHS) across Central Queensland. This model aimed to enhance diabetes-related foot disease (DFD) care by integrating virtual and local MDTs.
Aim
This study presents early implementation learnings from frontline clinicians involved in the co-design, implementation and refinement of this innovative model-of-care (MOC).
Methods
A preparatory phase involved stakeholder engagement, service mapping and funding allocation to RBWH for recruitment. Site preparedness varied, influencing referral rates. A mixed-methods approach was used to evaluate challenges and successes, with input from local end-users.
Discussion
Key enablers included local champions, collective leadership and integration with existing providers. At Rockhampton Base Hospital, the MDT expanded subsequently improving care coordination. However, challenges such as funding constraints, hybrid health information systems, and technological barriers affected implementation. Discipline-specific insights highlighted the need for structured communication, local workforce expansion and ongoing refinement of MOC.
Conclusion
The Central Foot Hub enhanced access to specialist care and optimised local service delivery for people living with DFD in Central Queensland. Sustainable scale-up will require additional funding, streamlined health information systems and continued collaboration between healthcare providers across HHS.
Summary
- Diabetes related foot disease disproportionately affects Australians living in regional/remote communities.
- Our innovative virtual multidisciplinary model-of-care aims to address this service gap.
- General and discipline-specific barriers were identified during early implementation.
- Addressing these barriers through iterative co-refinement and diverse stakeholder engagement will be required for sustainability.
The ‘Central Foot Hub’ operationalised in mid-February 2024 aimed to provide multidisciplinary (MDT) support from Royal Brisbane and Women's Hospital (RBWH) to three hospital and health services (HHS) covering a vast geographical area across Central Queensland, Australia. Here, we share early implementation learnings from frontline clinicians involved in the co-design, implementation and ongoing refinement of this innovative model-of-care (MOC) (Figure 1).
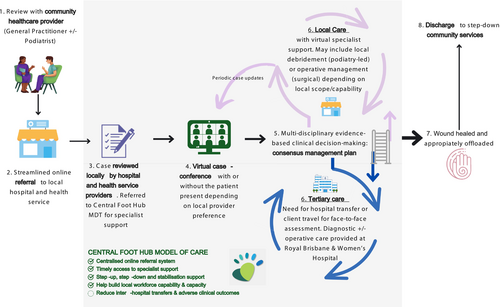
A significant planning period comprising stakeholder and community engagement, service mapping and conceptualisation across HHS partners preceded operationalisation. Funding was initially allocated to the RBWH site for recruitment. Preparedness among partner sites varied, with some reorganising their clinic structures to integrate with the Hub, while others maintained usual operations. Site preparedness correlated with referrals to the Hub.
1 General Learnings
Partner site preparedness was driven by local champions who identified the Hub as an opportunity and spearheaded change and a positive organisational culture. Collective leadership promoted co-development that tailored the virtual MOC to suit local needs.
The Hub connected pre-existing local providers in the DFD care space. This resulted in the creation of an MDT at one of our partner sites at Rockhampton Base Hospital consisting of an orthopaedic surgeon, a dual trained diabetes educator/wound care nurse, podiatrists and an exercise physiologist. The Rockhampton MDT streamlined its clinical workflows and was able to broaden its acute management capacity and geographic reach. This led to a greater need for step-down services in their community.
With rapid scale-up of the Rockhampton MDT, referrals to the Hub began to slow down after an initial peak. Funding shortfalls and unequal resource distribution were identified as key challenges—specifically the need for local co-ordinators to optimise workflows.
Hybrid health information systems created challenges with cross-site coordination. Both hub and partner MDT members agreed electronic integration would improve productivity, reduce administrative workload, positively contribute to patient safety and minimise low-value healthcare. Such infrastructural advancements were also deemed critical for MOC scale-up.
Barriers to virtual MOC adoption included varying levels of health and technology access and literacy among DFD patients. Factors often accompanying complex chronic disease impacted our patients' abilities to engage independently in telehealth consultations with Hub specialists. In response, the Rockhampton MDT introduced basic screening processes to identify patients requiring extra support for whom they facilitated co-consultations between local providers and Hub specialists.
2 Discipline-Specific Learnings
2.1 Podiatry
Handover and information sharing between partner sites was critical, with frequent requests for updates requiring structured communication. Escalation of deteriorating patients to vascular teams via the Hub also increased due to relationship building. The collaborative model was effective at HHS with established podiatry teams; however, regions with limited access to local podiatry support provide an additional challenge and remain an area for growth.
2.2 Endocrinology
Delays in health-seeking behaviours eventuated in complicated diabetes presentations. Financial, food and housing insecurity were also common. Streamlining DFD care to local providers with whom patients could build rapport and seek assistance from to co-ordinate their care provided opportunities for multiple frequent interactions where small interventions could be delivered. This encouraged the patient to remain engaged, motivated and adopt recommendations and self-management strategies. This relationship building with the local diabetes educators and general practitioners was crucial for delivery of specialist diabetes interventions through the Hub.
2.3 Vascular Surgery
Delays currently exist in the referral, review and intervention of patients with vascular disease from regional/rural areas, often resulting in emergent presentations [1] This MOC allowed for a more efficient pathway for triaging vascular referrals and identifying high-risk patients, leading to earlier intervention and improved clinical outcomes. Enhanced communication between partner sites allowed continued expert wound care and permitting patients to stay local improved adherence with follow-up—both significant contributors to reducing morbidity. The success of this approach is heavily weighted on the interest and expertise available at the partner sites. Therefore, further upskilling and allocation of resources are required to allow its continuation.
2.4 Orthopaedics
Improved access to vascular, endocrinology and psychology prompted the streamlining of pathways for patients with DFD. All patients with high-risk/deteriorating DFD were seen in the local MDT clinic by orthopaedics, podiatry and a diabetes educator, with local advice from our infectious diseases team. Input from the tertiary team was invaluable when planning both conservative and surgical management, from simple digit amputations to complex Charcot reconstructions. Optimised glucose control and vascular supply ensured wounds healed in a timely manner. Patients, where possible, were managed in clinic and community using the Hospital in the Home MOC, with semi-elective admissions occupying fewer bed days and keeping patients' care near to home. A victim of our own success, however, these clinics are now overflowing with a huge workload with no added funding distributed regionally.
2.5 Diabetes Educator
The merging of local and virtual MDT provided our local high-risk foot patients living with diabetes a more holistic approach to care and reduced the need for travel to a major tertiary centre. Historically, this cohort has had limited access to endocrine and psychological support. For a diabetes educator, the opportunity to work collaboratively with the Hub provided professional support and development for our local workforce. However, this amazing service and relationships came with increasing workload and time constraints. Two of our biggest challenges now are the sharing of communication between HHS and recruiting to our local workforce to deal with the rapidly increasing referrals.
2.6 Psychology
It is widely acknowledged that the DFD population has higher rates of depression, anxiety and cognitive impairment, which can lead to poor outcomes [2]. The aim of Hub psychology was the assessment of mood, cognition and behaviour, which informed brief intervention and recommendations [3]. Initial feedback from local sites was that psychologist involvement provided a deeper insight into the patient's beliefs and perceived barriers, which allowed for tailored communication and appropriate referrals to local services. Support was also provided to upskill clinicians in managing emotional distress, and this resulted in fewer referrals to psychology for normative distress.
3 Conclusion
We identified a number of general and discipline-specific enablers and barriers. Ongoing co-refinement through diverse stakeholder inputs, mixed-methods [4-6] evaluations and strong partnerships between healthcare providers, researchers and governments will support the sustainability of our MOC.
Author Contributions
Shanal Kumar: conceptualization, writing – original draft, supervision, resources. Amy Walker: writing – original draft, writing – review and editing. Caitlin Leech: writing – original draft, writing – review and editing. Emma Powell: writing – original draft, writing – review and editing. Ruth Varrall: writing – original draft, writing – review and editing. Siobhan Ramsay: writing – original draft, writing – review and editing. Rebecca Searle: writing – original draft, writing – review and editing. Sarah Jensen: writing – review and editing, supervision.
Acknowledgements
Open access publishing facilitated by The University of Queensland, as part of the Wiley - The University of Queensland agreement via the Council of Australian University Librarians.
Open Research
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.