Can intubate, cannot ventilate: A proposed algorithm to handle problems with ventilation and oxygenation after intubation
Abstract
Background and Methods
Few guidelines address how to handle unanticipated ventilatory problems and hypoxemia in a successfully intubated patient. We will refer to this situation as “can intubate–cannot ventilate.” The situation may occur immediately after intubation or later during general anaesthesia. The aim of this paper is to describe an algorithm for handling this situation. In an intubated patient, the airway can be considered a continuum from the ventilator to the alveoli, and the problem is somewhere along this route: Ventilator → Hoses → Filter → Tracheal tube (TT) → Tracheae → Bronchi → Bronchioles → Alveoli. The proposed algorithm is based on clinical experience and has not been externally validated.
Results
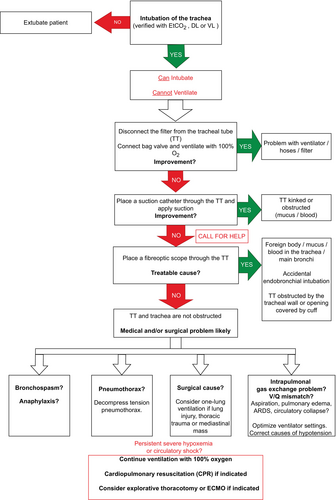
The first critical decision to be made is whether the TT has been placed correctly in the trachea or not. Positive wave-formed capnography is the primary marker for correct intubation. Video and/or direct laryngoscopy can be used for further verification. The patient should be disconnected from the ventilator and manually ventilated with bag-valve and 100% oxygen. An open tube should then be verified by applying a suction catheter through the tube. If these measures do not improve the situation, a fibreoptic scope should be inserted to further assess possible causes of difficult ventilation. If no obvious treatable cause is detected at this point, bronchospasm, anaphylaxis, or pneumothorax should be ruled out or treated. Further handling should focus on optimizing gas exchange in the lungs and considering more advanced treatment options to improve oxygenation and circulation.
Conclusions
We have proposed an algorithm to handle unanticipated problems with ventilation and oxygenation in a patient who has been successfully intubated. Equipment failure and a blocked TT should be ruled out before diagnosing and treating medical or surgical causes of ventilatory problems.
Editorial Comment
This article presents a logical approach to the time-sensitive and critical situation where, for some reason, after intubation, ventilation of the lungs is not succeeding. The authors propose steps for a systematic approach, and recognition of different possible explanations for ventilation not working is informative.
1 INTRODUCTION
There are several guidelines on how to manage the difficult airway, including the “cannot intubate–cannot oxygenate” (CICO) situation.1 However, few guidelines address how to handle unanticipated ventilatory problems and hypoxemia in a successfully intubated patient. We will refer to this situation as “can intubate–cannot ventilate.” The situation may occur immediately after intubation or later during general anaesthesia, during elective procedures or in severely ill patients. It may occur in the operating room (OR), intensive care unit (ICU), in the emergency department (ED) and in the prehospital environment. Like other airway challenges, rapid recognition and immediate handling are keys to success. The severity and most likely cause may vary considerably, depending on the patient and clinical setting. However, troubleshooting and handling can, in our opinion, follow the same principles.
In aviation, space flight and other high-risk industries, algorithms and checklists have been used for decades to lower the risk of adverse events when performing complex tasks. Checklists may also reduce the risk of adverse events during anaesthesia and surgery.2-4 Algorithms have become a standard in airway management and resuscitation, to make us less dependent on memory when handling stressful situations, and to reduce the risk of common “cognitive errors” in decision making.1, 5 The overall aim is to improve clinical performance and teamwork under psychological stress. The main aim of this paper is to propose an algorithm for troubleshooting and handling a “can intubate–cannot ventilate” situation.
2 METHODS
After a serious adverse event with postintubation hypoxemia at our institution, we saw the need for a structured approach to handle unanticipated problems with ventilation and oxygenation in a successfully intubated patient. After performing searches in the scientific literature, we did not identify any clinical algorithms that systematically addressed how to handle this situation in general. Westhorpe and Runciman with co-workers have defined frameworks and algorithms for general crisis management in anaesthesia, including one specific for bronchospasm, but these may not be readily applicable.6, 7 The situation may cause confusion on whether the patient has been successfully intubated or not, which may cause stress and disorder. Both a decision to extubate a correctly intubated patient who is hypoxemic, and a decision to follow the proposed algorithm in a patient with oesophageal intubation can further worsen hypoxemia. We saw the need for an algorithm that could aid in differentiating the “can intubate–cannot ventilate” situation from the CICO situation. The proposed algorithm has so far not been externally validated.
When facing ventilatory problems and subsequent hypoxemia after assumed correct intubation, the problem is somewhere along this continuum. We propose a systematic troubleshooting of the airway “from the ventilator to the alveoli”. The first step is to confirm that the tracheal tube (TT) has been placed correctly in the trachea. The next steps aim to verify that this continuum has been established. If the problem is establishing this continuum, follow the algorithm for an unanticipated difficult airway.1
3 RESULTS
The suggested algorithm is presented in Figure 1, and we recommend following the steps described in Sections 3.1, 3.7.
3.1 Verify tracheal tube placement
Capnography is considered the primary marker of correct tracheal intubation.8 Not using capnography after intubation contributed to 74% of deaths or severe cerebral injury in the ICU and ED described in the fourth National Audit Project (NAP4) in 2011.9 However, a normal capnography curve requires a sufficiently inflated cuff, sufficient pulmonary perfusion and sufficient ventilation of alveoli. Thus, an abnormal capnography curve does not rule out correct TT placement if the cuff is leaking, cardiac output is very low, in massive pulmonary embolism, or if severe airway obstruction is present.10, 11 Correct placement of TT can be verified by video laryngoscopy (VL) or direct laryngoscopy (DL) in the absence of normal capnography (or a capnograph). The members of the team can assess VL through a shared screen, as this may ease decision making and team confidence in correct TT placement. Depth of tube placement should be assessed and corrected if endobronchial intubation can be suspected. If a decision on correct TT placement cannot be made, the patient should be extubated and the guidelines for the management of an unanticipated difficult airway should be followed.1
3.2 Disconnect the ventilator, connect the tracheal tube to a bag-valve with 100% oxygen for manual ventilation
Disconnecting the ventilator and manually ventilating the patient with a bag-valve (BV) and 100% oxygen will eliminate any errors related to the ventilator, hoses and filter (points a–c). BV ventilation will also ease ventilation with higher pressures and give the clinician a “hands-on” feeling of whether the patient is difficult to ventilate or not. A cuff leak may be apparent at this point if not detected before. The bag-valve should be connected to capnography if available, to increase clinical information available for the team. If the problem with ventilation and/or oxygenation remains, the problem is located somewhere from within the TT and forwards (Sections 3.3, 3.7).
3.3 Check whether the TT is open or not
Insert a suction catheter through the TT to check if the tube is kinked, compressed or clotted. Application of suctioning may remove any mucus or blood that obstructs the tube. Then retry BV-ventilation. If the insertion of a suction catheter was easy and ventilatory problems sustain, the problem is somewhere between the tip of the TT and the alveoli. Both disconnecting the ventilator, manually BV-ventilating the patient, and opening the tube with a suction catheter are simple procedures with equipment readily available. If the problem is not resolved at this point, call for help if not already done. Further troubleshooting and treatment will most likely require more personnel, more equipment and possibly the use of medications. A systematic troubleshooting up to this point will allow others to quickly understand how far the team has progressed in the algorithm and what the next steps should be.
3.4 Insert a fibreoptic scope through the TT
- The TT has been kinked.
- There is a foreign body, mucus or blood in the TT, trachea or bronchi. In case of massive atelectasis, suction guided by fibreoptic scope may be considered.
- The TT is placed in a main bronchus rather than in the trachea.
- The cuff of the TT is obstructing the tube outlet.
- The tube outlet is wedged against the tracheal wall. This problem may be more prevalent in tubes without Murphy's eye.
- The TT or the trachea has been compressed, for instance, due to a mediastinal mass.12
A fibreoptic assessment will confirm whether the TT is open and correctly placed in the trachea, although this may require the ventilations to be paused unless a closed system is used. If an emergent change of tube is indicated in the presence of hypoxemia or difficulties intubating the patient in the first place, an airway exchange catheter should be considered. If no problems have been uncovered so far, the cause is most likely in the lung or thoracic cavity (Sections 3.5, 3.7) and any failures related to the equipment should have been ruled out. Reconnection to the ventilator can be considered at this time, as this will provide capnography and clarify what inspiratory pressures are needed to ventilate the patient sufficiently.
3.5 Rule out or treat bronchospasm
The “mindset” of the airway as a continuum will now place attention on the bronchus. Bronchospasm is an important differential diagnosis in the handling of ventilatory problems after intubation, with an estimated incidence of 1.3–1.7 of 1000 patients receiving general anaesthesia.13, 14 Classical signs include the need for high inspiratory pressure, a prolonged expiratory phase, hypoxemia, rising end-tidal CO2 (EtCO2) and the development of hypercapnia.7, 15 Smoking, obesity and obstructive pulmonary disease have been shown to substantially increase the risk of bronchospasm.13, 16 Bronchospasm may be an isolated phenomenon during induction, or it can be part of an anaphylactic reaction, most often due to antibiotics or neuromuscular blocking agents.17 Anaphylaxis may present with one or more of bronchospasm, skin rash, hypotension and/or tachycardia.15, 17, 18 Perioperative anaphylaxis has an estimated incidence of 1 in 10,000 anaesthesias, so bronchospasm will in most cases have a different cause than anaphylaxis.17 Bronchospasm can be considered at several steps, although it is more readily diagnosed and treated after equipment failure and physical obstructions in the tube or trachea have been excluded. The treatment of acute bronchospasm depends on the severity and whether an anaphylactic reaction is present. The different treatment options for bronchospasm are beyond the scope of this paper.
3.6 Rule out or treat pneumothorax
Pneumothorax (PT) may be caused by surgery, preoperative thoracic injury, or procedures such as the placement of a central line. Unilateral chest rise and absence of respiratory sounds on stethoscopy during ventilation may be suggestive of PT. The risk of spontaneous PT is higher in patients with underlying lung disease.19 A feared complication in a patient with PT receiving positive pressure ventilation is the development of tension PT, which may cause hypotension or cardiac arrest. This may be erroneously diagnosed as anaphylaxis. The use of ultrasound to assess the presence or absence of “lung sliding” bilaterally is a non-invasive method to rapidly diagnose PT.20 If rapidly available, a chest x-ray can be considered, although it may not exclude PT. Tension PT should be treated with immediate needle chest decompression, followed by open thoracostomy and/or insertion of a chest drain.21 In the lack of sufficient improvement, one-lung ventilation of the non-affected side may theoretically improve oxygenation in severely hypoxemic patients, although we found no reports on this strategy published in the literature.
3.7 Identify and treat problems with intrapulmonary gas-exchange
If the possible causes described in Sections 3.1, 3.6 have been excluded and/or treated, the problem may be some type of ventilation/perfusion (V/Q) mismatch or other cause of impairment in intrapulmonary gas exchange. This will be more likely in a critically ill or injured patient, compared to an otherwise healthy patient scheduled for an elective procedure. Depending on the clinical setting, ultrasound protocols may be helpful in identifying causes of acute respiratory or circulatory failure and should be a mandatory part of training.22, 23 High inspiratory pressures may impede venous return and contribute to circulatory failure. Optimization of ventilator settings, deepening of anaesthesia, gastric decompression, neuromuscular blockade (if not already provided) and putting the patient emergently in the prone position are measures that can be considered. Gastric decompression may be particularly relevant in children who have been ventilated by mask. If circulatory failure is present, it should be actively treated to maximize oxygen delivery to tissues. Blood gases should be assessed when this is feasible. The application of extracorporeal membrane oxygenation (ECMO) may be an option if oxygen saturation is possible to keep above a critical level until ECMO has been established.15 In patients with major thoracic trauma or recent thoracic surgery, emergent thoracotomy may be considered to identify and treat reversible causes of severe respiratory or circulatory failure.24, 25 Describing more advanced diagnostic assessments and treatment options for oxygenation failure is beyond the scope of this paper.
4 DISCUSSION
We have proposed a short algorithm on how to handle unanticipated problems with ventilation and oxygenation in a patient who has been successfully intubated. The algorithm will help the treatment team to identify the most likely cause and handle the situation in a logical and structural manner, treating or ruling out problems as the algorithm is followed. It is important to rule out equipment failure, including obstructed TT, before treating the patient with medications or more invasive measures described in Sections 3.5, 3.7. The simple approach proposed is both a strength and a weakness of the algorithm. It does not and cannot solve all possible problems with ventilation and oxygenation in an intubated patient but may rapidly uncover the most likely problems. When feasible, communication with the surgeon should be initiated to clarify whether the surgical procedure should be performed after the problems have been resolved or surgery should be postponed. If ventilatory problems or hypoxemia may be related to an underlying surgical condition, the surgeon should be called immediately.
It is crucial to apply the algorithm only when correct tracheal intubation has been verified. Sufficient doubt of whether the TT is correctly placed is an exclusion criteria for applying the algorithm. To remove a correctly placed TT, or to not remove an incorrectly placed TT, will further worsen hypoxemia and psychological stress. In this situation, the use of VL can help the entire team to decide whether the TT is placed correctly or not. A wrong decision to extubate will worsen the situation, but if neither capnography nor VL can confirm correct TT placement, the patient should be extubated. The proposed algorithm shares similarities with the DOPES acronym and a proposed algorithm to handle post intubation hypoxemia described at the “Life in the fast lane” blog site.26 DOPES is an acronym for: D—displacement, O—obstruction, P—patient, E—equipment and S—stacked breaths (bronchospasm and ventilator settings). Although easy to remember, the acronym itself does not include a prioritization of measures that can be rapidly applied when facing a “can intubate–cannot ventilate” situation. Implementation of the algorithm will require an educational program that should be part of departmental training in airway management. We believe the classical “when in doubt–take it out” mindset for tracheal intubation may be a barrier to implementation, which will require emphasis on decision making when verifying tube placement.
The main weaknesses of the algorithm are the lack of external validation, lack of a systematic literature search, and scientific grading of the strength of recommendations. New algorithms in airway management should ideally be followed by a scientific study or quality improvement program (QIP). A randomized trial may not be feasible, but the incidence and the degree of success handling the types of situations can be followed in cohort studies or QIP. Chassin and co-workers have proposed “accountability measures” to address processes of care in QIPs, including measures that the intervention (actually) is provided and that there are few other intervening processes between the intervention and any improved outcome.27 To what degree each step of the algorithm is followed, and the immediate results of any intervention given at each step can be explanatory variables and outcomes in a scientific study or QIP. Applying a Delphi method may be considered to further develop such algorithms.
5 CONCLUSIONS
We have proposed an algorithm to handle unanticipated problems with ventilation and oxygenation in a patient who has been successfully intubated. The airway of an intubated patient is a continuum from the ventilator to the alveoli, and the problem is somewhere along this route. Equipment failure and a blocked TT should be ruled out before diagnosing and providing potent treatment options for bronchospasm, anaphylaxis, pneumothorax or problems with intrapulmonary gas exchange.
AUTHOR CONTRIBUTIONS
KF and TN: Conceptualization. Methodology. Writing - Original Draft. Writing - Review & Editing. Visualization. Project administration. Resources. MS, BG and SEG: Conceptualization. Writing - Original Draft. Writing - Review & Editing. Visualization.
FUNDING INFORMATION
No funding provided.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.




