High-flow via a tracheostomy tube and speaking valve during weaning from mechanical ventilation and tracheostomy
The study was performed at Department of Medicine Solna, Karolinska Institutet, Stockholm, Sweden, Remeo Intensive Care Rehabilitation Center, Stockholm, Sweden, and Medical Centre of Leeuwarden, Leeuwarden, The Netherlands.
Abstract
Background
Weaning from mechanical ventilation and tracheostomy after prolonged intensive care consume enormous resources with optimal management not currently well described. Restoration of respiratory flow via the upper airway is essential and early cuff-deflation using a one-way valve (OWV) is recommended. However, extended OWV use may cause dry airways and thickened secretions which challenge the weaning process. High-flow therapy via the tracheostomy tube (HFT-T) humidifies inspired air and may be connected via an in-line OWV (HFT-T-OWV) alleviating these problems. We aim to provide clinical and experimental data on the safety of HFT-T-OWV along with a practical guide to facilitate clinical use during weaning from mechanical ventilation and tracheostomy.
Methods
Data on adverse events of HFT-T-OWV were retrieved from a quality register for patients treated at an intensive care rehabilitation center between 2019 and 2022. Benchtop experiments were performed to measure maximum pressures and pressure support generated by HFT-T-OWV at 25–60 L/min flow using two different HFT-T adapters (interfaces). In simulated airway obstruction using a standard OWV (not in-line) maximum pressures were measured with oxygen delivered via the side port at 1–3 L/min.
Results
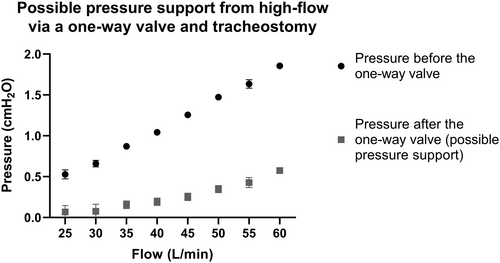
Of 128 tracheostomized patients who underwent weaning attempts, 124 were treated with HFT-T-OWV. The therapy was well tolerated, and no adverse events related to the practice were detected. The main reason for not using HFT-T-OWV was partial upper airway obstruction using a OWV. Benchtop experiments demonstrated HFT-T-OWV maximum pressures <4 cmH2O and pressure support 0–0.6 cmH2O. In contrast, 1–3 L/min supplemental oxygen via a standard OWV caused pressures between 84 and 148 cmH2O during simulated airway obstruction.
Conclusions
Current study clinical data and benchtop experiments indicate that HFT-T-OWV was well tolerated and appeared safe. Pressure support was low, but humidification may enable extended use of a OWV without dry airway mucosa and thickened secretions. Results suggest the treatment could offer advantages to standard OWV use, with or without supplementary oxygen, as well as to HFT-T without a OWV, for weaning from mechanical ventilation and tracheostomy. However, for definitive treatment recommendations, randomized clinical trials are needed.
Editorial Comment
High-flow therapy in tracheostomised patients weaning from mechanical ventilation was well tolerated. The inspired gas humidification and low pressure levels appeared to be advantageous and promising. The treatment recommendations should however be interpreted cautiously until there is highly reliable evidence available to support these.
1 INTRODUCTION
Weaning patients from mechanical ventilation and tracheostomy after prolonged intensive care may be time and resource consuming. A tracheostomy is commonly performed to facilitate mechanical ventilation and aid weaning when this is difficult or prolonged.1, 2 However, a tracheostomy tube with an inflated cuff negatively impacts saliva management and swallowing3, 4 in addition to leaving the patient without a voice.3, 4 By deflating the cuff and using a one-way valve (OWV), also known as a speaking valve, expiratory flow through the upper airway is restored and pharyngeal and laryngeal rehabilitation necessary for tracheostomy weaning4-6 may commence in parallel to weaning from mechanical ventilation.4-6
While heating and humidification of inhaled gas is common practice during mechanical ventilation and continues while using a OWV in-line (in the ventilator circuit),7-10 patients using a OWV off the ventilator risk dry airways as room air will be inhaled through the OWV and tracheostomy tube. The lack of humidification may damage the airway mucosa and render secretions dry and difficult to mobilize with risks of sputum retention and mucus plugs.11, 12 The beneficial effects of the OWV, restoring natural peep, the possibility to cough and mobilize mucus, and use one's voice,5, 13 may be offset by airway dryness. Thus, the time using the OWV must often be limited, or alternative humidification options sought.
In patients with a tracheostomy, heated and humidified high-flow therapy (HFT) is regularly used during weaning from mechanical ventilation, either via nasal cannula or via the tracheostomy tube (HFT-T) to allow oxygenation and active humidification of inhaled gas.14-17 The use of HFT-T via an in-line OWV (HFT-T-OWV) is becoming more common, though is not yet described in guidelines for management and care for tracheostomies within the ICU.18 Furthermore, the high flow rates may pose a risk when applied through a OWV and clinical data on the use of HFT-T-OWV and potential adverse effects are lacking.
The aim of this study was to investigate adverse events that occurred from the use of HFT-T-OWV in patients weaning from mechanical ventilation and tracheostomy and to, in an experimental setting, measure maximum pressures and pressure support generated by HFT-T-OWV. Finally, we aimed to compare the safety of HFT-T-OWV to the use of a standard OWV in a simulated airway obstruction. A practical guide based on best available evidence was developed to facilitate safe implementation of HFT-T-OWV for patients weaning from mechanical ventilation and tracheostomy.
2 METHODS
The study was conducted at two international sites. Patient clinical data and safety outcomes of HFT-T-OWV as standard care were documented at the Remeo intensive care rehabilitation center in Stockholm, Sweden. Benchtop experiments exploring the impact of HFT-T-OWV and a traditional OWV on artificial airway pressures were performed at the Intensive Care Unit of the Medical Centre of Leeuwarden, Leeuwarden, the Netherlands.
2.1 Clinical study
Patients with a prolonged ICU stay were referred to the Remeo intensive care rehabilitation center in Sweden. Data from all patients with a tracheostomy treated at the center from May 2019 to April 2022 were retrieved retrospectively from a quality register. Adverse events reported to the register included cardiac arrest with initiated heart-lung resuscitation, hypoxia necessitating manual ventilation, tracheal intubation/recannulation, accidental decannulation, pneumothorax, severe bleeding, anaphylaxis and hypoglycemia (<2.2 mmol/L). Information on use of HFT-T-OWV was retrieved from the register and, in cases where HFT-T-OWV was not used, the reason for this was sought from the patient's medical records. HFT was delivered using the Airvo 2 (Fisher and Paykel Healthcare, Auckland, New Zealand) with 30–40 L/min flow, temperatures of 34–37°C and oxygen supplementation to meet the patients' prescribed oxygen saturation. The OWV used was the Passy Muir 007 (Passy Muir, Irvine, California, United States). Tracheostomy tubes used were almost exclusively the Portex Bivona Adult TTS or the Portex Blue Line Ultra Suctionaid (Smiths Medical, Minneapolis, Minnesota, United States) in sizes 7 or 8 mm, both with an inner cannula. The study was approved by the Swedish Ethical Review Authority (Dnr 2020–05246) and informed consent not sought due to the study design.
2.2 Benchtop experiments
Five benchtop experiments were performed to determine (1) the maximum pressure generated by HFT-T-OWV, (2) the pressure required to open the membrane of the Passy Muir 007 OWV, (3) the possible pressure support generated by HFT-T-OWV treatment, (4) the pressure generated if the open system used for HFT-T-OWV should be omitted and (5) possible pressure produced by low-flow oxygen administered via the side port of a standard OWV. All benchtop experiments were undertaken in May–November 2022. Given no patient involvement, ethical approval was not sought.
A Servo U ventilator (Getinge AB, Gothenburg, Sweden) set in High-flow mode was used with a Humidification System F & P 950 and a Ventilator Circuit Kit 950A81 (Fisher and Paykel Healthcare, Auckland, New Zealand). For HFT-T-OWV experiments, the Passy Muir 007 OWV was used. The tracheostomy tube was a size 9 mm cuffed Tracoe Twist Plus REF316 FEN with fenestrations closed (Tracoe medical GmbH, Nieder-Olm, Germany). Pressures were measured by using a PF 300 (IMT Analytics AG, Buchs, Switzerland).
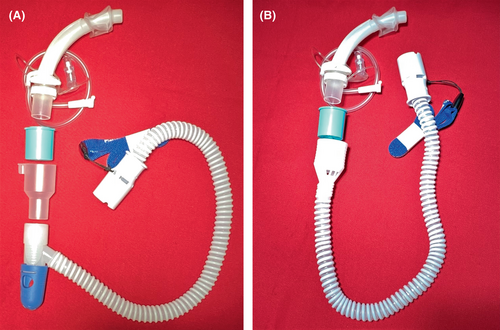
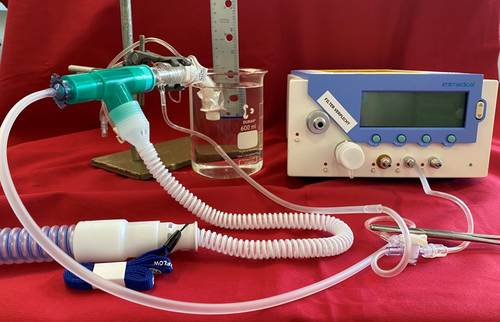
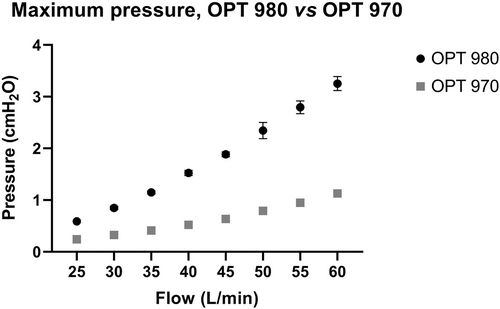
Experiment 1. To provide HFT-T-OWV, an adapter (interface) with side holes is necessary to prevent high pressures. The characteristics of this “open system” depend on the adapter design. The first experiment compared the HFT-T-OWV maximum pressures using the OPT 970 and the OPT 980 adapters (Fisher and Paykel Healthcare, Auckland, New Zealand; Figure 1) which differ considerably in size of the side holes. The total area of the one small and two large holes of the OPT 970 measure 377 mm2, while the six small holes of the OPT 980 measure 66 mm2 in total (personal communication with the manufacturer). The absence of flow through the OWV and tracheostomy tube for maximum pressure measurements was confirmed by keeping the tracheostomy tube tip below the water surface of a filled container (Figure 2). If flow occurred, bubbles would be visible, and the tip of the tube moved deeper under water.19 Pressure was measured after the adapter's side holes, before the OWV. High-flow settings were changed in 5 L/min increments and pressures measured for each flow setting, twice in a sequence from 25 to 60 L/min and twice from 60 to 25 L/min. The PF 300's calibration was checked in each series.
Experiment 2. The Passy Muir 007 OWV has a bias closed design, meaning that the valve is closed when no flow is present. Consequently, pressure is required to open the valve. In a second experiment, this pressure was approximated by calculating the difference in pressure just before the OWV's membrane and inside the tracheostomy tube once flow was initiated. Pressure immediately before the OWV's membrane was measured by the PF 300 set in low-pressure range. The tip of the tracheostomy tube was kept under water and gradually elevated reducing the depth. The pressure inside the tube was approximated by measuring the water depth at which bubbles first appeared at the tube tip, indicating the opening of the OWV. The measurements were performed four times, first with the OPT 980 at flow rates of 50 and 60 L/min and then with the OPT 970 at the same flow rates.
Experiment 3 was performed to determine the resistance of the Passy Muir 007 OWV and possible pressure support generated by HFT-T-OWV. Pressures were measured immediately before and after the OWV with the tip of the tracheostomy tube open, the pressure difference representing the OWV's resistance, and the pressure measured after the OWV approximating the pressure support. High-flow settings were changed and pressures measured in four series as in the first experiment's protocol.
Experiment 4. To investigate the importance of an open system, a fourth experiment was conducted. An oxygen blender was used as high-flow source because it lacks an obstruction alarm, a release valve and a shut-off function for high pressure. The ventilator tubing used fits directly onto the Passy Muir 007 OWV, omitting the adapter making the system closed instead of open. Pressure was measured on the patient side of the OWV with the PF 300 set in the high-pressure range. To simulate airway obstruction, the trachesostomy tube was blocked on the patient's side. Connections were tested for leakage. The planned flow rates were 30, 40, and 50 L/min with a gradual increase from 5 L/min.
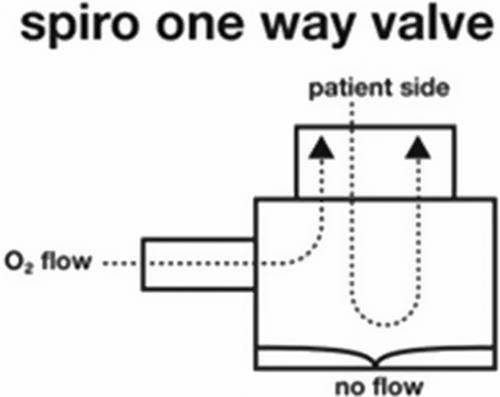
Experiment 5 was performed to determine pressures generated by low-flow oxygen administered to the side port of a standard OWV if the expiratory airflow was to be blocked, as in an airway obstruction. For this experiment, a OWV not designed for in-line use, the Spiro OWV (Atos Medical, Zoetermeer, The Netherlands) was used. This OWV is frequently utilized in weaning and is equipped with a side port for oxygen delivery, located on the patient's side of the membrane (Figure 3). It has a bias open design, implying that leakage may occur before the OWV is closed during exhalation. The side port was connected to a medical oxygen flow meter set to 1, 2, and 3 L/min of oxygen. To simulate airway obstruction, the tracheostomy tube was blocked on the patient's side and pressures measured by the PF 300 set in the high-pressure range. Connections were tested for leakage. Measurements were performed for 10 s after reaching peak pressure.
2.3 Statistics
For analysis of maximum pressure in the first benchtop experiment, a two-way ANOVA was performed followed by Šídák's multiple comparisons test. Data of the second experiment were normally distributed and mean values and standard deviations (SD) are presented. Measurements from the third experiment of pressure support and pressure drop across the Passy Muir 007 OWV were analyzed using one-way ANOVA followed by test for linear trend. All analyses were performed using GraphPad Prism version 9.4.1 for Windows, GraphPad Software, San Diego, California, USA, www.graphpad.com.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
3 RESULTS
3.1 Clinical study
During the three-year study period, 136 patients with tracheostomies were admitted to the Remeo intensive care rehabilitation center in Sweden. Eight patients permanently dependent on mechanical ventilation and not subjected to weaning attempts were excluded from analysis. Characteristics of the 128 included patients are reported in Table 1. Of the 128 patients, 124 (97%) were treated with HFT-T-OWV all or most of their time off the ventilator until decannulation. Nearing the end of the weaning process, HFT-T-OWV was applied day and night, also during sleep. This was well tolerated with no adverse events. Over the three-year period, no death or severe complication could be attributed to the HFT-T-OWV treatment. Of the 124 patients subjected to HFT-T-OWV treatment, 112 (90%) were successfully decannulated within a median time of 31 days.
| Age–mean | 57 (16) |
| Sex–n (%) | |
| Male | 81 (63) |
| Female | 47 (37) |
| Days treated in acute care before transfer to the center (median (range)) | 38 (4–142) |
| Days in ICU before transfer to the center (median (range)) | 29 (4–124) |
| Number of patients with an ICU stay >10 days, n (%) | 125 (98) |
Days with tracheostomy before transfer to the center (median (range))a |
22 (2–127) |
| Admission diagnoses | |
| Neurological–n (%) | 72 (56) |
| Traumatic–n | 28 |
| Hemorrhagic stroke–n | 23 |
| Infectious–n | 13 |
| Other | 8 |
| Infection (excluding neurological infections)–n (%) | 36 (28) |
| Thoracic and vascular–n (%) | 7 (5) |
| Respiratory failure–n (%) | 5 (4) |
| Other–n (%) | 8 (6) |
- a n = 126 due to missing data.
Four (3.2%) of the 124 patients treated with HFT-T-OWV died at the center. Two failed to recover despite prolonged rehabilitation efforts whereby weaning attempts were discontinued and palliative care commenced. Another two deteriorated several weeks after decannulation and subsequently died. One patient who suffered repeated episodes of pneumothorax, was diagnosed with another pneumothorax after HFT-T-OWV was tried using a OPT 970 adapter. No relation to the HFT-T-OWV treatment could be confirmed, however the therapy was not continued. No other adverse events for patients weaned with or without HFT-T-OWV were reported to the register.
Four patients admitted for ventilator and/or tracheostomy weaning were not treated with HFT-T-OWV as one patient died before weaning attempts commenced and three had a partial upper airway obstruction during exhalation when using a OWV. Only one of these patients was successfully decannulated.
3.2 Benchtop experiments
The maximum HFT-T-OWV pressures measured in the first experiment were flow-dependent, higher when using the OPT 980 with smaller side holes compared to the OPT 970 (p < .001) but in all cases <4 cmH2O (Figure 4).
The mean pressure required to open the Passy Muir 007 OWV measured in the second experiment was 0.50 (SD 0.023) cmH2O.
In the third experiment, the possibility to provide pressure support by HFT-T-OWV was explored. Due to the results of the first experiment, only the OPT 980 adapter was investigated. Pressure was reduced after the Passy Muir 007 OWV with a flow-dependent positive linear trend (p < .001). According to the experiments, pressure support by HFT-T-OWV was between 0 and 0.6 cmH2O (Figure 5).
In the fourth experiment, conducted to illuminate the importance of the open system for HFT-T-OWV, the adapter was omitted, and an oxygen blender flow source connected directly to the Passy Muir 007 OWV. Pressure very quickly rose above 500 cmH2O at 5 L/min, the firmly attached connections came off and the chamber of the active humidifier started cracking. Repeated attempts gave similar results, and the experiment was not completed.
In the fifth experiment, using the Spiro OWV, the maximum pressure on the patient's side of the OWV was measured with 1, 2, and 3 L/min of oxygen delivered via the side port. Pressure rapidly increased to 84, 119, and 148 cm H2O, respectively. When reaching maximum pressure at each set flow, the OWV membrane leaked at the center attachment. At 3 L/min, the membrane deformed and bulged through the grid, and the experiment was stopped. No statistics were applied to these data.
4 DISCUSSION
In this study, we present clinical data that support safe use and high tolerance of HFT-T-OWV in patients weaning from mechanical ventilation and tracheostomy. No adverse events, considered related to the therapy, were reported. Benchtop experiments detected no high pressures using appropriate equipment though the results emphasize the importance of the open system adapter. Furthermore, HFT-T-OWV may provide a safer alternative than a standard OWV when supplemental oxygen is necessary, reducing the risk of very high pressures in case of an airway obstruction. Although pressure support generated by HFT-T-OWV was confirmed to be low, the ability to provide continuous active humidification allowing for extended OWV use with improved safety, argues for the advantages of HFT-T-OWV for patients weaning from mechanical ventilation and tracheostomy.
Adverse events were rare in the present clinical study, and none of these were assessed to be directly attributed to the use of HFT-T-OWV. The treatment was routinely applied for extensive periods of time for the vast majority of patients, including for 24 h/day towards the end of the weaning process. Patient acceptance of treatment was high and in only three cases could the therapy not be applied as a OWV could not be used. Mortality was low in line with previous research data from the center,20 and causes of deaths were not considered related to HFT-T-OWV treatment. The one incident of pneumothorax in a patient with repeated pneumothoraxes was deemed unlikely to be related to the HFT-T-OWV treatment, a conclusion supported by the benchtop experiments where maximum pressures were <2 cmH2O using the OPT 970 adapter. The limited number of patients and the retrospective design of the study did not allow for comparisons of outcome between treatment groups. However, the safety of HFT-T-OWV treatment is congruent with research performed at the Prince Charles Hospital ICU in Brisbane, Australia21 where 25 consecutive patients using HFT-T-OWV with flow settings of 30–60 L/min were treated successfully with no adverse events reported.21
The goal of HFT-T-OWV is to provide adequate humidification combined with the positive effects of a OWV. Before a OWV is applied, the tracheostomy tube cuff must be deflated to allow complete exhalation through the upper airway. This may permit room air to be inspired through the upper airway in addition to through the tracheostomy.6 The fraction of inspired room air depends on the resistance to inhalation through the upper airway outside the tracheostomy tube compared to through the OWV and tracheostomy tube. As room air may also enter through side holes of the adapter, the size of the side holes and the HFT-T flow setting will be additional important determinants. Flow rates of 30 L/min of heated and humidified air have been shown to enhance mucociliary transport and reduce the number of suctioning procedures in patients with a tracheostomy,11 and in the present clinical study, flow rates of 30–40 L/min were used with satisfactory results. For maximum humidification, flow settings should match the patient's peak inspiratory flow, however, these were not reported to the quality register.
A low, but potentially beneficial, CPAP effect has been found for HFT nasal cannula.22 In comparison, the HFT-T CPAP effect is modest, while still helpful during the weaning process.17, 19 The present study's benchtop experiments confirmed no or very little pressure support by HFT-T-OWV. Pressure drop across the OWV occur for two reasons, first to open the Passy Muir 007 OWV membrane and second,23, 24 because of its flow-dependent resistance.23, 24 Therefore, restoring physiological PEEP by OWV use is likely more important for lung recruitment, as found in clinical studies using lung impedance,7, 8 than providing pressure support by HFT-T-OWV. Furthermore, early cuff deflation and OWV use for restoration of airflow through the upper airway are advocated to be crucial components in laryngeal and pharyngeal rehabilitation.5 OWV use is preferable to capping the tracheostomy tube as it can be started earlier, when the patient is still on the ventilator, and there is a reduced need to downsize the tracheostomy tube. The risk of dry airway mucosa is eliminated when the OWV is combined with the active humidification of HFT-T, removing time-restriction of OWV use. However, select patients, for example with excessive dynamic airway collapse or other forms of central airway obstruction, may benefit from CPAP generated by HFT via nasal cannula in addition to the PEEP provided by the upper airways and capping of the tracheostomy tube.25, 26
Upper airway obstruction restricting exhalation is the greatest risk when using a OWV. Airway patency needs to be thoroughly assessed before OWV use4, 6, 27-29 and staff must be appropriately trained as the tracheostomy cuff must be deflated before applying the OWV.4, 6, 27-29 The clinical study was undertaken at an intensive care rehabilitation center where patient evaluation and treatment were performed by an experienced interprofessional team (medical, nursing and allied health) trained in OWV use. Congruent with previous literature, this likely contributed to the lack of adverse events related to the HFT-T-OWV treatment.30 The safety of HFT-T with or without a OWV in-line depends on the open system adapter. This was confirmed in the fourth benchtop experiment, where high pressures were observed when the adapter was omitted. Furthermore, if HFT-T is used without an in-line OWV, backflow of mucus may block adapter side holes of smaller size, compromising the open system. Here, the bias closed Passy Muir 007 OWV provide additional safety, preventing backflow of mucus into the tracheostomy tube, and thus the risk of obstruction of the valve or adapter side holes.
The choice of HFT source may influence the risk of high pressures, as demonstrated in the fourth experiment where an oxygen blender, not equipped with pressure release valves nor pressure/occlusion alarms delivered HFT. Furthermore, standard ventilator tubing were used without an adapter for HFT-T. No adverse events considered related to the HFT-T-OWV treatment were reported in the current clinical study, where a stand-alone HFT source with tubing that cannot fit the OWV without an open system adapter was used, demonstrating the importance of appropriate equipment for safety.
Administering oxygen via HFT-T-OWV may be a safer alternative than via the side port of a standard OWV. As demonstrated in the fifth benchtop experiment, the bias open design of the Spiro OWV did not prevent the very high pressures when simulating airway obstruction. The driving pressure for an oxygen flow meter is typically very high, with no safety valves or pressure alarms between the flow meter and the patient, explaining why such high pressures could be obtained. Clinically, erroneous use of OWV have been reported to cause detrimental effects.31, 32 In addition to the benefits of humidifying the airway mucosa, HFT-T-OWV may present a safer alternative to low flow oxygen via the side port of a standard OWV. We argue that HFT-T-OWV may be the safest treatment option for patients suitable for OWV use during weaning from mechanical ventilation and tracheostomy.
The present study has several strengths. The clinical data and the benchtop experiments are congruent and support the safety of the treatment. The Clinical Guidance provided below, may also help to ensure safe practice. However, clinical data were collected from only one center. Including multiple sites may have provided different, more varied results and a larger sample size, a necessity to detect uncommon adverse events. Moreover, although the register was checked regularly for completeness and accuracy, the possibility to address integrity of data-collection retrospectively was limited. Though it is unlikely that emergencies such as accidental decannulation or intubation/recannulation would not be registered, brief episodes of manual ventilation because of desaturation, for example in connection to mobilization of secretions, might not have been considered severe or life threatening and thus not registered.
4.1 Clinical guidance
Based on current evidence, expert opinion, and the authors' clinical experience, the following advice is proposed to facilitate safe implementation of HFT-T-OWV into clinical practice for patients weaning from mechanical ventilation and tracheostomy. It should be noted that this is not an endorsed clinical practice guideline. Complete information for guideline development is lacking, and there are no large randomized clinical trials to evaluate the practice.
4.1.1 Safety considerations before start of treatment
- If the patient is not awake and alert,33 a thorough assessment of upper airway patency must be conducted4, 5, 34 (Table 2).
- The cuff of the tracheostomy tube must be fully deflated before the start of OWV treatment9, 10 since all exhaled air must pass the upper airway.
- An adapter (interface designed with appropriately sized side holes) intended for HFT-T must be used to prevent high pressure.
- Equipment intended for heated, humidified HFT should be used, either as a stand-alone unit or a ventilator set in high-flow mode equipped with pressure release valve and occlusion alarm.
| Recommendation | Rationale |
|---|---|
| Multidisciplinary team including speech pathology evaluation is recommended for upper airway assessment.4-6, 28-30 | Appropriately trained staff are able to notice issues with upper airway patency and can conduct an instrumental assessment when needed. |
| With cuff fully deflated, assess for adequate airflow via the upper airway during exhalation. Check for signs of stridor or an audible difference between inhalation and exhalation during momentary finger occlusion or OWV trial.6 Tracheostomy tube manometry is a safe and reliable alternative to finger occlusion test.24, 27, 33, 36 Use of cervical auscultation with a stethoscope is advantageous. | Safe use of a OWV requires sufficient tracheal space around the tracheostomy tube to allow full exhalation via the upper airway, past the deflated cuff.27 Airway obstruction or limited space around the tracheostomy tube cause risk for air-trapping, CO2 retention and/or breath-stacking.6 |
| Assess ability to manage upper airway secretions.4, 5, 34 Monitor closely for excessive saliva/secretion pooling in the larynx/pharynx; wet/gurgly voice, “wet” cough. | Abundant saliva/secretion pooling in the larynx and pharynx, above the cuff, may be a negative indicator for OWV use. However, restoring airflow through the upper airway with a OWV is essential for laryngeal and pharyngeal rehabilitation and to improve coughing and swallowing.4, 5, 13 |
| Assess larynx and pharynx for adequate voicing, coughing and swallowing.5, 6, 28 | If inadequate voicing or coughing is noted, and/or pooled saliva/secretions is observed, possible laryngeal dysfunction and/or dysphagia should be assessed.4, 6, 28, 34 |
| Limit OWV use to short periods of time if ability to manage saliva and upper airway secretions is poor. It is preferred to use HFT-T with the cuff deflated,18 however, for patients who cannot manage their saliva/secretions, HFT-T without a OWV may be continued with the cuff inflated. | A OWV improves swallowing and secretion clearance,5, 13 and should be considered also for patients with poor pharyngeal and laryngeal function. Periods of OWV use may be successively prolonged for laryngeal and pharyngeal rehabilitation to target early successful decannulation. |
| Assessment via Flexible Endoscopic Evaluation of Swallowing (FEES) is recommended.4-6, 30, 34 | Assessment of laryngeal and pharyngeal sensory and motor function is invaluable in the diagnostics of an adequate cough and swallow for saliva/secretion management as well as for oral intake of food and drink. A thorough FEES assessment also provides a foundation for individualized and evidence-based rehabilitation of the larynx and pharynx.4-6, 30 |
4.1.2 Initiating therapy, attachments, and settings
- Before deflating the cuff, remove secretions from the mouth, tracheal cannula35 and sub-glottic port (if available) by suctioning.
-
Adequately explain the procedure to the patient including
- - change in airflow (return of normal expiratory airflow through the upper airway).
- -
risk for secretions in upper airway/throat that need to be coughed up and out, or swallowed.
Rationale:
- ○ Patients may experience coughing or discomfort during the initial cuff deflations, it is important that they are aware of this to reduce anxiety or stress.
- ○ Patients should try to cough up and swallow secretions as a step to normalize swallowing function.
-
For patients weaning from mechanical ventilation, consider cuff deflation while the patient is still on the ventilator and preparing for a period of HFT-T-OWV off the ventilator.
Rationale:
- ○ The positive airway pressure will cause upward airflow past the deflated cuff and pooled saliva/secretions above the cuff will be moved up into the pharynx and oral cavity, reducing the risk of aspiration.
- Assess upper airway patency. Momentary finger occlusion6, 24 offers a first impression.6, 24 Tracheostomy tube manometry is a safe and reliable alternative.24, 33, 36
-
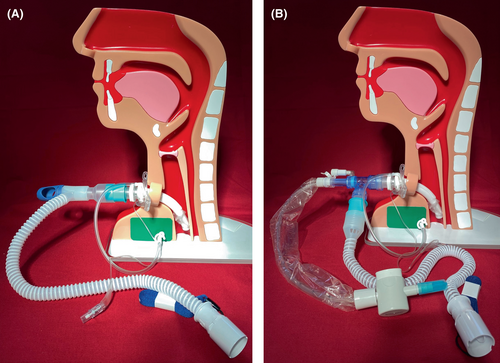
- Attaching HFT to the OWV and tracheostomy tube (Figure 6)
-
No specific type of tracheostomy tube is needed as most can fit a OWV.
- ○ Fenestrated tubes are not necessary nor preferred.
- ○ If a tracheostomy tube inner cannula is used, it can be left in place. With certain tracheostomy brands, the inner cannula is necessary to fit the OWV.
-
The OWV should be designed for in-line use.
- ○ Adapters for HFT-T do not fit a standard OWV not designed for in-line use.
- ○ Adapters with larger side holes may require a 15 M/22F connector to fit an in-line OWV (Figure 6A).
-
A high-flow adapter with side holes must be used.
-
The equipment used to provide HFT should be intended for this purpose and correctly connected.
- ○ A stand-alone HFT device can be used. These devices may be designed with tubes that do not fit a tracheostomy tube or a OWV without the adapter, reducing the risk to erroneously apply HFT-T without an adapter.
- ○ A ventilator with a pressure release valve and obstruction or pressure alarm may be used set in high-flow mode. Note that ventilator tubing (with no side holes) may fit directly onto the tracheostomy tube and/or OWV without an adapter potentially resulting in high pressures. Applying an open system adapter and checking connections carefully is mandatory.
- A closed suction system can be used and left in place (Figure 6B).
-
- HFT-T-OWV settings
-
Settings for optimal humidification of inhaled air will vary between patients and need to be adjusted accordingly. Ventilator readings of peak inspiratory flow rates may be used to guide initial flow settings. To avoid inhalation of room air and to achieve maximum humidification, flow rates of 40–60 L/min are usually required.
- ○ In general, higher flow rates are better tolerated by patients when applied through a tracheostomy tube than via a nasal cannula.37
- ○ Later in the weaning process patients may achieve adequate humidification with lower flow rates (30–40 L/min).
-
Initial temperature should be set to 37°C.
- ○ Temperature may be adjusted to as low as 32°C if perceived too warm (usually due to the leakage) but humidification will then be reduced.
-
- Supplementary oxygen and nebulized medications
-
Initial oxygen setting (FiO2) may be guided by ventilator settings.
- ○ A decrease in patient oxygen saturation after switching to HFT-T or HFT-T-OWV may be caused by too low flow rate (decreased FiO2 due to inhalation of room air). In this case, flow should be increased before adjusting FiO2 settings.
- ○ Note that if a separate HFT-T equipment is used with oxygen supplemented at a set flow rate, increasing the HFT-T flow may decrease FiO2. If a stable FiO2 is desired, oxygen flow must be adjusted proportionally to HFT-T flow.
-
During nebulization of medication, HFT-T-OWV treatment should be temporarily suspended.
- ○ The OWV may become sticky as a result of nebulized medication and must be removed in advance to avoid malfunctioning.
- ○ Local guidelines regarding nebulization of medication during HFT may be present. For complete administration and to prevent contamination of the environment,38, 39 treatment may be temporarily suspended during nebulization of medication.
-
- Cleaning and care of equipment
- The HFT system should be cleaned and maintained according to the manufacturer's instructions.
- The OWV needs to be rinsed in soapy water daily and left to dry in room air
5 CONCLUSIONS
Current study clinical data and benchtop experiments indicate that HFT-T-OWV was well tolerated and appeared safe during weaning from mechanical ventilation and tracheostomy. Though pressure support by HFT-T-OWV was low, humidification could enable extended OWV use without dry airway mucosa and thickened secretions. The treatment may offer advantages to HFT-T without the in-line OWV as well as to a standard OWV, with or without supplementary oxygen, and potentially facilitate early, safe and efficient weaning from mechanical ventilation and tracheostomy. However, further research including larger patient populations and interventional trials are recommended for establishing definitive treatment recommendations.
AUTHOR CONTRIBUTION
Conception and study design: Eva Sundman, Anna-Liisa Sutt, Peter Egbers and Liza Bergström. Data collection: Peter Egbers, Liza Bergström, Eva Sundman and Jenny Petersson. Data analysis: Eva Sundman, Peter Egbers, Jenny Petersson and Liza Bergström. Drafting, editing and final review of manuscript: all authors.
FUNDING INFORMATION
The study was financed by departmental funding at The Remeo Intensive Care Rehabilitation Center, Stockholm, Sweden and the Intensive Care Unit of the Medical Centre of Leeuwarden, Leeuwarden, The Netherlands.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




