Loss expression of micro ribonucleic acid (miRNA)-200c induces adverse post-surgical prognosis of advanced stage non-small cell lung carcinoma and its potential relationship with ETAR messenger RNA
Abstract
Background
Non-small cell lung cancer (NSCLC) is the leading cause of cancer mortality worldwide. As micro ribonucleic acid (miRNA)-200 and ETAR may play an essential role in the process of epithelial to mesenchymal transition (EMT) simultaneously, the purpose of this study was to detect the expression of miRNA-200c and ETAR messenger (m)RNA and assess their prognostic significance in early stage NSCLC.
Methods
Our study included 78 advanced stage (IIB, IIIA, IIIB) NSCLC patients. All patients were smokers. Using quantitative reverse transcriptase polymerase chain reaction analysis, we detected the expression of miRNA-200c and ETAR mRNA and assessed their correlation by χ2 test. Time to progression was used as the recurrent index and was assessed by univariate and multivariate analysis in the Cox hazard model.
Results
Both miRNA-200c and ETAR mRNA expression are associated with N stage and tumor node metastasis (TNM) stage in a series of advanced NSCLC patients. Among N stage and TNM stage patients, significant differences were found in IIB (P = 0.0126), IIIB (P = 0.0107) and N0 (P = 0.0023) and in N1 + N2 groups (P = 0.0133). Using both univariate and multivariate survival analyses, we found that miRNA-200c (hazard ratio [HR] = 0.352, 95% confidence interval [CI]: 0.187–0.662) and ETAR mRNA (HR = 2.500 95% CI: 1.345–4.647) were independent prognostic factors, independent of TNM stage (HR = 2.414, 95% CI: 1.600–3.642) and differentiation (HR = 1.530, 95% CI: 1.050–2230).
Conclusions
miRNA-200c induces an expedient surgical survival, whereas ETAR mRNA has the reverse prognosis in advanced stage NSCLC patients. A potential relationship exists in that miRNA-200c targets ETAR mRNA during EMT.
Introduction
Accounting for 1.2 million deaths each year, non-small cell lung cancer (NSCLC) is the primary cause of cancer mortality in both sexes, with an overall five-year survival rate of only 10–15%.1 Despite therapeutic advances in recent years, the high mortality of patients with NSCLC has not been substantially reduced, largely because of the potential of invasion, metastasis, and frequent recurrence.2 Another important reason for poor outcomes is that NSCLC is often only detected after it has spread beyond the primary site. If the cancer is diagnosed at an early stage, the five-year survival rate increases to about 50%.3 Therefore, the discovery of biomarkers and their application in conjunction with NSCLC cancer diagnosis, staging, and prognosis, which could help improve early diagnosis and patient care, are extremely urgent.
Micro ribonucleic acids (miRNAs) are small, noncoding RNAs that modulate gene expression post-transcriptionally by interacting with multiple mRNAs and inducing either translation suppression or degradation of mRNA and play essential roles in many physiological and pathological processes, including tumor development.4 Accumulating evidence suggests that miRNAs may be involved in controlling lung cancer development and play critical roles in its pathogenesis.5 Recently, the miR-200 family (including miR-200a, miR-200b, miR-200c, miR-141, and miR-429) has been shown to play an essential role in the process of epithelial to mesenchymal transition (EMT), which is confirmed as the fundamental process of tumor invasion and metastasis.6 Concerning EMT, many studies have revealed the critical role of the endothelin axis (ET-1/ETAR) in tumor invasion and metastasis, and propose the hypothesis that miRNA-200 could inhibit EMT by targeting ETAR messenger (m)RNA.7, 8
In the present study, we investigated the expression of miRNA-200c and ETAR mRNA in 78 NSCLC patients through quantitative reverse transcriptase polymerase chain reaction (RT-PCR) and preliminarily evaluated the correlation between them. Finally, we assessed their relationship with clinic-pathological parameters and prognosis in the prospective clinical setting.
Materials and methods
Patients and specimens
From May 2009 to April 2011, 78 advanced stage NSCLC patients treated by curative surgical resection at the Department of Thoracic Surgery at the Affiliated Hospital of Medical College, Qingdao University, were enrolled in our investigation. All of the patients were smokers before a definite diagnosis was made (they were requested to cease smoking prior to surgery), and had no history of chemotherapy or associated co-morbidities.
Samples from the 78 advanced NSCLC patients were frozen in liquid nitrogen at the central laboratory of our hospital immediately after surgical resection. Clinical and pathological characteristics advised by the World Health Organization and the Union for International Cancer Control were included in our investigation: gender, age, histology, N stage, tumor node metastasis (TNM) stage, and differentiation. These are listed in Table 1. Written and informed consent was obtained from all patients and the ethical committee of our hospital approved the investigation.
| Variables | Cases | miRNA-200c | P-value | ETAR | P-value | |||
|---|---|---|---|---|---|---|---|---|
|
Negative N (%) |
Positive N (%) |
Negative N (%) |
Positive N (%) |
|||||
| Total | 78 | 39 | 39 | 39 | 39 | |||
| Gender | Male | 61 | 29 | 32 | 0.4106 | 31 | 30 | 0.7839 |
| Female | 17 | 10 | 7 | 8 | 9 | |||
| Age | <60 | 36 | 16 | 20 | 0.3636 | 17 | 19 | 0.6496 |
| ≥60 | 42 | 23 | 19 | 22 | 20 | |||
| Histology | Squamous | 24 | 13 | 11 | 0.4190 | 12 | 12 | 0.9602 |
| Adenocarcinoma | 35 | 19 | 16 | 18 | 17 | |||
| Other | 19 | 7 | 12 | 9 | 10 | |||
| T stage | T1+ T2 | 37 | 15 | 22 | 0.1125 | 18 | 19 | 0.8206 |
| T3 | 41 | 24 | 17 | 21 | 20 | |||
| N stage | N0 | 31 | 15 | 16 | 0.0109 | 19 | 12 | 0.0026 |
| N1+N2 | 47 | 24 | 23 | 20 | 27 | |||
| TNM stage | IIB | 21 | 9 | 12 | 0.0185 | 11 | 10 | 0.0164 |
| IIIA | 32 | 15 | 17 | 19 | 13 | |||
| IIIB | 25 | 15 | 10 | 9 | 16 | |||
| Differentiation | Well | 19 | 10 | 9 | 0.5080 | 11 | 8 | 0.6137 |
| Moderate | 24 | 10 | 14 | 13 | 11 | |||
| Poor | 35 | 19 | 16 | 15 | 20 | |||
- miRNA, micro ribonucleic acid; NSCLC, non-small cell lung cancer; TNM, tumor node metastasis.
Ribonucleic acid (RNA) extraction
Total RNA was isolated using Trizol reagent (Invitrogen, Carlsbad, CA, USA) according to the manufacturer's protocol.9 The concentration and purity of the RNA samples were determined by measuring the optical density in 260/280 nm ratios with a spectrophotometer. Ten nanograms of the total RNA preparations from each sample was reverse-transcribed to cDNA, stored at −80°C until analysis.
Quantitative reverse transcriptase polymerase chain reaction analysis for microRNA-200c and ETAR messenger RNA
Quantitative PCR was performed by monitoring the fluorescence of SYBR Green dye on a StepOne real time PCR system (Life Technologies, Carlsbad, CA, USA) in a total 20-μL reaction volume with cycling conditions of: 95°C for 10 seconds, followed by 40 cycles of 95°C for five seconds, 60°C for 20 seconds, and 72°C for 15 seconds. Applied primer pairs (based on human EMBL sequences) of ETAR mRNA were 5′-TGTTTTGATTTGGGTCTCT-3′ (forward primer) and 5′-AGCAAGCAGATTCGCAGATAAG-3′ (reverse primer). The specific forward and reverse primers of miRNA-200c were designed and synthesized by LC Sciences (Hangzhou, China). The relative expression level of miRNA-200c and ETAR mRNA was normalized by comparison with the glyceraldehyde 3-phosphate dehydrogenase (GAPDH) gene using an appropriate primer, synthesized in the central laboratory of our hospital. Samples were also subjected for separation on 2% agarose gel electrophoresis for ensuring the correct product amplification. All experiments were performed in triplicate.
Statistical analysis
The expressions of miRNA-200c and ETAR mRNA were divided into two groups of “low” (negative) and “high” (positive) according to the median level, and the Chi-square tests were performed to compare miR-200c and ETAR mRNA expression levels with the patients' clinicopathologic features. Cox univariate analysis was performed to compare time to progression (TTP) survival between groups using a log-rank test. The value of the independent prognostic factors was assessed in multivariate analysis using the Cox hazard model. All statistical analyses were performed with the SAS 9.2 software (SAS Institute Inc., Cary, NC, USA) and statistical differences at P < 0.05 were considered to be statistically significant.
Results
The expression of miRNA-200c and ETAR mRNA and their correlation with clinical parameters
Each patient was followed up every two months after surgery, with the longest follow up period being 40 months. Sixty-one men and 17 women were selected for inclusion in our investigation, with a mean age of 61.4 years (range 45–77 years). Using PCR analysis in clinicopathological variables, both N stage and TNM stage were associated with miRNA-200c and ETAR mRNA (Table 1). In light of this connection, we then analyzed the expression of miRNA-200c and ETAR mRNA in each group, according to the clinical parameters of TNM stage and N stage. We found significant differences between the TNM (IIB: P = 0.0126; IIIB: P = 0.0107) and N stage groups (N0: P = 0.0023; N1 + N2: P = 0.0133) (Table 2).
| Variables | χ2 | P-value |
|---|---|---|
| Gender | 5.7664 | 0.0163 |
| Age | 3.7116 | 0.0540 |
| Histology | 0.2834 | 0.8679 |
| T stage | 0.6627 | 0.4156 |
| N stage | 0.5227 | 0.4679 |
| TNM stage | 19.1572 | <0.0001 |
| Differentiation | 6.3969 | 0.0408 |
| miRNA-200c | 11.3813 | 0.0007 |
| ETAR mRNA | 8.9450 | 0.0028 |
| Combination | 23.7647 | <0.0001 |
- mRNA, messenger ribonucleic acid; miRNA, micro RNA; TNM, tumor node metastasis.
The survival significance of clinicopathological variables in non-small cell lung cancer
The mean TTP of all patients was 21 months (range 1–40 months). Using univariate analysis, our data indicated that the survival rates had a high correlation with gender (P = 0.0163), TNM stage (P < 0.0001), differentiation (P = 0.0408), miRNA-200c (P = 0.0007), and ETAR mRNA (P = 0.0208). We found that individuals with an elevated miRNA-200c had a mean TTP of 26.5 months, while the mean TTP was 16.3 months in those without an elevated miRNA-200c (Fig 1). Conversely, the mean TTP of individuals with positive ETAR mRNA expression was 16.8 months, while negative ETAR mRNA expression was 25.2 months (Fig 2). As shown in Figure 3, significant differences were found in TTP between miRNA-200c positive/ETAR mRNA negative and miRNA-200c negative/ETAR mRNA positive patients, with a mean TTP of 27.5 and 13.5 months, respectively. We combined miRNA-200c and ETAR mRNA as a new parameter and found these had a better survival rate than any of the other clinicopathological factors in our investigation (χ2 = 23.7647, P < 0.0001) (Table 3). Multivariate analysis of all of the factors influencing TTP using a Cox regression model revealed that miRNA-200c and ETAR mRNA expression were independent prognostic factors (hazard ratio [HR] = 0.352, 95% confidence interval [CI]: 0.187–0.662; HR = 2.500 95% CI: 1.345–4.647), independent of TNM stage (HR = 2.414, 95% CI: 1.600–3.642), and differentiation (HR = 1.530, 95% CI: 1.050–2230).
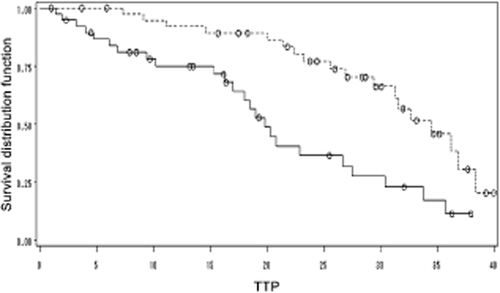
Postsurgical survival curve according to micro ribonucleic acid (miRNA)-200c (continuous line indicates negative miRNA-200c expression; discontinuous line indicates positive miRNA-200c expression). STRATA:  , miRNA200C = 0;
, miRNA200C = 0;  , censored miRNA200C = 0;
, censored miRNA200C = 0;  , miRNA200C = 1;
, miRNA200C = 1;  , censored miRNA200C = 1.
, censored miRNA200C = 1.
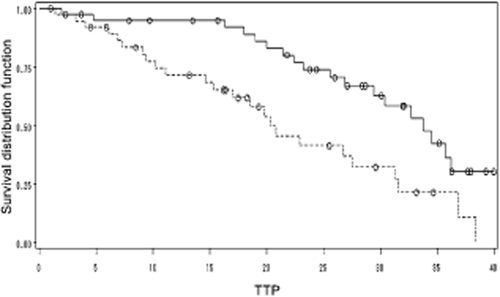
Postsurgical survival curve according to ETAR messenger ribonucleic acid (mRNA) (continuous line indicates negative ETAR mRNA expression; discontinuous indicates positive ETAR mRNA expression). STRATA:  , ETARmRNA = 0;
, ETARmRNA = 0;  , censored ETARmRNA = 0;
, censored ETARmRNA = 0;  , ETARmRNA = 1;
, ETARmRNA = 1;  , censored ETARmRNA = 1.
, censored ETARmRNA = 1.
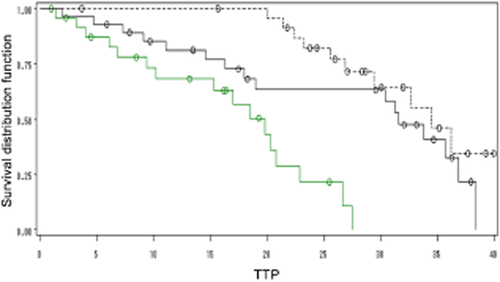
Postsurgical survival curve according to the combination of micro ribonucleic acid (miRNA)-200c and ETAR messenger (m)RNA (green solid line: miRNA-200c negative and ETAR mRNA positive; black dotted line: miRNA-200c positive and ETAR mRNA negative). STRATA:  , combination = 1;
, combination = 1;  , censored combination = 1;
, censored combination = 1;  , combination = 2;
, combination = 2;  , censored combination = 2;
, censored combination = 2;  , combination = 3;
, combination = 3;  , censored combination = 3.
, censored combination = 3.
| χ2 | P-value | HR | 95% CI | |
|---|---|---|---|---|
| TNM stage | 17.6385 | <0.0001 | 2.414 | 1.600–3.642 |
| Differentiation | 4.9031 | 0.0268 | 1.530 | 1.050–2.230 |
| miRNA-200c | 10.4924 | 0.0012 | 0.352 | 0.187–0.662 |
| ETAR mRNA | 8.3881 | 0.0038 | 2.500 | 1.345–4.647 |
- mRNA, messenger ribonucleic acid; miRNA, micro RNA; NSCLC, non-small cell lung cancer; TNM, tumor node metastasis.
Discussion
NSCLC, a tumor type with high metastatic potential and the leading cause of cancer death represents a great challenge to clinicians and basic scientists to determine the molecular markers associated with progression and prognosis.10, 11 Our present study firstly detects the expression of miR-200c and ETAR mRNA and reveals their correlation in a series of NSCLC patients (all of whom were smokers). We then evaluated the prognosis and prognostic significance of TTP in advanced stage NSCLC patients.
We found a highly significantly correlation between the expression of miRNA-200c and ETAR mRNA in carcinoma tissue, determining that both miRNA-200c and ETAR are associated with TNM stage and N stage, similar results to previous studies.
The process of EMT is linked with dramatic changes in cellular morphology, the downregulation of E-cadherin, and the upregulation of vimentin and N-cadherin, leading to migratory and invasive capabilities.12, 13 EMT requires transcriptional reprogramming to suppress E-cadherin expression via specific transcription factors, such as Snail, Slug, FOXC2, Twist, ZEB1, and ZEB2, as shown in Figure 4.14 In initial reports, transfection of miR-200c reduced cancer cell migration and invasion, indicating a potential inhibitory role in malignant tumor progression.15 Allgayer et al. found that miRNA-200c is significantly associated with differentiation and lymphatic metastasis and the loss of miR-200c expression induces an aggressive, invasive, and chemoresistant phenotype in NSCLC.16 More recently, a study suggested a role of miRNA-200 as a suppressor of EMT by directly targeting the transcriptional repressors ZEB1 and ZEB2 leading to the upregulation of E-cadherin, enhancing migration and invasion during cancer progression.17 miRNAs modulate gene expression post-transcriptionally by interacting with multiple mRNAs and induce either translation suppression or degradation of mRNA. The ET axis, in particular ET-1, is an initiator of EMT in the lung, where it helps to transform alveolar type II cells, activating the ETA-receptor, leading to the upregulation of TGF-β and promoting the invasion and metastasis of lung carcinoma cells.18 In invasive behavior, integrins and the integrin-linked kinase activated by ET-1 play an additional modifying role.19 On the basis of our statistical data with the intense correlation and consistency between miRNA-200c and ETAR mRNA, we speculate that ETAR is one of the targeting genes of miRNA-200c and further confirmed the central role of miR-200c in the regulation of the epithelial versus mesenchymal phenotype and in the malignant progression of lung cancer cells acting on the endothelin axis. Although the underlying biological mechanism is unclear, the direct or indirect link existing between miRNA-200c and ETAR mRNA could be a new research orientation.
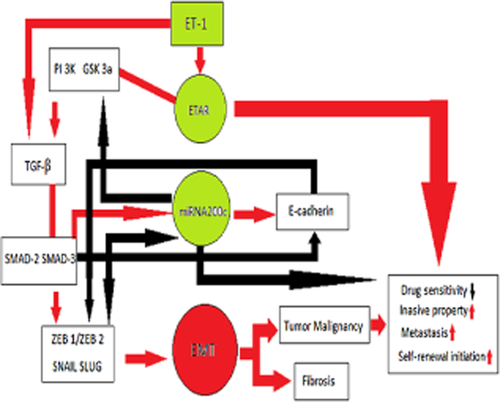
Signaling network of endothelin axis (ET) and micro ribonucleic acid (miRNA)-200, the ET axis can be influenced by miRNA-200c on different pathways (red arrows: induction of pathway; black arrows: blockade of pathway).
Finally, we used TTP as the post-surgical prognosis index to evaluate the prognostic significance of miRNA-200c, ETAR, and clinical parameters.20 Cox multivariate survival analysis revealed that both miRNA-200c and ETAR mRNA are independent predictors: the elevated expression of miRNA-200c predicted a strong survival after surgery, while ETAR mRNA was just the opposite. In addition to miRNA-200c and ETAR mRNA, we also found that the clinical parameters of TNM stage have significant independent prognosis in our series, similar to the results of previous studies. Among the independent predictors, TNM stage was the most powerful predictor. Multiple studies have revealed that the endothelin system seems to be involved in the regulation of cell proliferation, angiogenesis, bone metabolism, pain control, and tumor invasion and is related to the poor prognosis of NSCLC.21
Although the extent to which miRNA-200c expression could enhance survival in NSCLC patients is unclear, our data indicate that a loss of expression of miRNA-200c predicts poor survival, regardless of other independent predictors. There is currently no direct evidence from previous research or formal clinical trials to guide treatment decisions for individual patients on the basis of miRNA-200c expression, but this study provides a new direction for future basic and clinical research of ETAR antagonist-based treatment strategies.22, 23 In view of the clinical data, ETAR antagonists in patients with cancer are encouraging. Future prospective investigations should be undertaken to determine the efficacy of miR-200c with the ETAR antagonist, which may accelerate the process of the endothelin antagonist as a first-line drug applied in a clinical setting. A combination of TNM stage, age, miRNA-200c, and ETAR mRNA expression may be used to classify patients as having a low, intermediate or high risk of death. A new direction for the treatment of NSCLC patients by inhibiting molecular marker expression should be applied in future clinical trials.24, 25
Several limitations present in our study must be acknowledged. First, as a prospective study, the evaluation of clinical response and TTP is often imprecise. Second, our study uses the data of a single-center small series and there may be a bias toward advanced NSCLC. Therefore, a larger study is necessary to validate our results.
Conclusion
In summary, our investigation revealed that a high expression of miRNA-200c predicts an advantageous post-surgical survival, while overexpression of ETAR mRNA induces a poor prognosis in advanced stage NSCLC. A potential relationship exists in that miRNA-200c targets ETAR mRNA during EMT. As clinicians, we can evaluate prognoses and enhance the quality of life of NSCLC patients by detecting and inhibiting miRNA-200c expression in the clinical setting. A novel research direction is emerging for basic scientists in that the miRNA family modulates the EMT process by targeting the endothelin system.
Acknowledgments
This study is supported by grants from Shandong Tackle Key Problems in Science and Technology (2010GSF10245); the Shandong Excellent Young Scientist Research Award Fund Project (BS2010YY013); and the Shandong Natural Science Fund (Y2008C48).
Disclosure
No authors report any conflict of interest.