Closing the miscommunication gap: A user guide to developing picture-based communication tools for Aboriginal and Torres Strait Islander peoples in emergency departments
Abstract
Objective
To document an illustration-based methodology for culturally safe communication between Indigenous patients and clinicians in an urban ED.
Methods
We co-designed a pre-ED visual tool to minimise miscommunication when triaging First Nations patients. Our steps included establishing project governance, conducting a literature review, obtaining ethics approval and designing illustrations. We then consulted relevant stakeholders, finalised the resource and contributed to the evidence base and to knowledge exchange.
Results
Co-design is an important principle in reducing miscommunication and ensuring cultural safety in EDs.
Conclusions
Co-design methodologies can guide improvements in culturally safe clinical communication with First Nations patients in EDs.
Introduction
Communication plays a vital role in ensuring patient safety and providing quality healthcare, particularly in high-stress environments such as EDs. When miscommunication occurs, patients can suffer serious adverse health consequences. Aboriginal and Torres Strait Islander patients frequently experience miscommunication when engaging with ED staff, particularly around language use (including Aboriginal English) and diversity of dialects.1 This is further heightened in a COVID-19 environment where ED staff are wearing full personal protective equipment and patients find it hard to hear the clinicians and see their faces.
Research has shown that pictorial guides, such as cartoon illustrations, are an effective strategy for conveying information, and significantly improve patient comprehension and compliance with ED discharge instructions and patient satisfaction.2 However, the use of illustration-based techniques in ED settings is not widespread and those that are available focus on hospital discharge care and instructions.3, 4
In Australia, few illustrative resources have been developed to communicate with Indigenous people seeking healthcare. There is also limited general information to support patients in the ED, and no peer-reviewed evidence describing the methodology used to develop such communication tools.
Thus, our research details both the available literature in this area and our methodology in developing a pre-ED communication tool to support the interests and concerns of Indigenous patients in a metro-urban ED in Melbourne.
Implementing the methodology
Our methodology is premised on both Indigenous and non-Indigenous methods of engagement and research (Fig. 1).
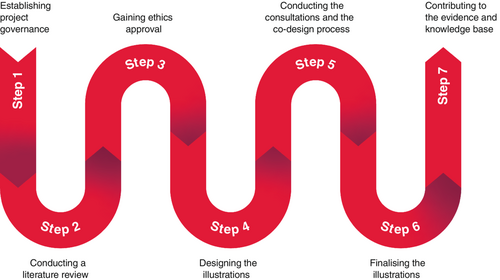
Step 1: establishing project governance
Project governance involves describing and implementing functions and processes that guide a project throughout its life cycle, and defining the structured roles, responsibilities and accountabilities within the project. Successful project governance strategies with First Nations patients must include an awareness of the diversity, rights and interests of the cultural groups represented; of how they want to have their strengths, concerns and priorities addressed; and of how cultural rules and values will be implemented.
Step 2: conducting a literature review
An extensive literature review provides an understanding of the cultural safety needs of First Nations patients in ED environments. After consulting with the project governance group, we chose two content areas – comprehension issues and pain management – identified from ED patient interviews in a previous research project1 as the focus of our communication tools, and reviewed more than 40 publications about them. A further literature review explored the types and usage of available illustration-based tools to ensure that the communication tools we developed are evidence informed.
Step 3: gaining ethics approval
As the research project was hospital-based, ethics approvals were required and needed to be site-specific, which was time-consuming and involved additional costs. This study received ethical approval from the St Vincent's Hospital Melbourne Human Research Ethics Committee (Project ID number: 79182).
Step 4: designing the illustrations
We contracted a professional illustrator to develop the illustrations. As these were to be trialled at a specific ED, the characters needed to be reflective of the hospital's location. Thus, Bunjil, the Wedge-tailed Eagle was chosen as the main character and narrator to ensure cultural local relevance and understanding among the local Koori community.
In addition to providing photos and soundscapes of the ED, we also worked closely with ED staff to develop scripts for the illustrator to ensure the resultant tools clearly explained how the ED operates and what to expect when visiting it.
Step 5: conducting the consultations and the co-design process
We held two online consultations with ED staff to co-develop the content of the illustrations and present the character drafts.
From there, three scripts were developed – the process of being triaged and admitted, the content of communicating levels of pain, and the experience of a parent (as a patient) bringing their children to the ED – which we shared with ED staff to verify their accuracy. Three online workshops were then held to obtain feedback on the drafts from Indigenous community members, ED staff and other hospital service providers. N.B. The authors are unable to share the feedback from workshop participants as the consent forms signed did not include using their words in publications.
Step 6: finalising the illustrations
The feedback was sent to the illustrator who revised the drafts several times before producing final versions of the illustrations (Fig. 2).

Step 7: contributing to the evidence and knowledge base
Knowledge exchange is an important part of implementing this pre-ED communication tool, which can contribute to the evidence base in several ways. There is opportunity, for example, to distribute these illustrations at Victorian Aboriginal community organisations that have referral pathways to hospitals and at local housing corporations.
Conclusion
To improve both the experience and health outcomes of Aboriginal and Torres Strait Islander people presenting at EDs, we need to create culturally safe and effective communication tools. This is best achieved through processes that recognise the essence of family and community relationships and why people present at EDs, and that facilitate this experience with as much dignity and camaraderie as possible. Good communication with Indigenous patients will require ED staff to learn about, understand and respond to cultural protocols. It will also require EDs and hospitals to take responsibility for venturing into intercultural spaces through committed and decisive action to address miscommunication, achieve equity and enhance access to EDs globally.
Acknowledgements
This project received Commonwealth funding and Australasian College for Emergency Medicine support as part of the Australian Government Department of Health Specialist Training Programme. Open access publishing facilitated by The University of Melbourne, as part of the Wiley - The University of Melbourne agreement via the Council of Australian University Librarians.
Author contributions
All authors listed have contributed to the concept and design of this Short Report, and have critically reviewed its content.
Competing interests
None declared.