Wound, pressure ulcer, and burn guidelines – 3: Guidelines for the diagnosis and treatment of diabetic ulcers and gangrene, second edition
This is the secondary English version of the original Japanese manuscript for the “Wound, pressure ulcer and burn guidelines – 3: Guidelines for the diagnosis and treatment of diabetic ulcers and gangrene published in The Japanese Journal of Dermatology 127(9):1989–2031, 2017. The authors have obtained permission for secondary publication from the Editor of in The Japanese Journal of Dermatology.
Abstract
The Japanese Dermatological Association aimed to prepare a second edition of guidelines for the management of diabetic ulcer/gangrene with emphasis on the diagnosis and treatment of skin symptoms. This new edition serves as a tool to improve the quality of the diagnosis and treatment in each patient and, further, to improve the level of care for such skin conditions. All sections have been updated by collecting documents published since the publication of the first edition. In the antibacterial drug treatment for bacterial infection of ulcers, oral administration was added after consideration. In the treatment of antibacterial drugs for bacterial infection of ulcers, not only infusion but also oral administration was mentioned. In addition, clinical questions (CQs) for imaging tests for diagnosing ischemia of the limbs were newly created. The titles of some CQs were changed to conform to the actual clinical setting. (i) The content has been updated by adding and collecting documents for all sections; (ii) we have additionally included oral antibiotic treatment for bacterial infection of ulcers; (iii) we have added CQs pertaining to imaging tests for diagnosing ischemia of the limbs; and (iv) we have revised the titles of some CQs to conform to the actual clinical setting. In particular, the recommendation levels of dressing materials newly covered by Japanese national health insurance are mentioned. In addition, CQs regarding the initial treatment of electrical (CQ15) and chemical burns (CQ16), and the use of escharotomy (CQ22) have been created.
1 BACKGROUND TO THE DRAFTING OF THE GUIDELINE FOR THE DIAGNOSIS AND TREATMENT OF DIABETIC ULCERS AND GANGRENE
Guidelines are “documents systematically prepared to support medical experts and patients for making appropriate judgments in particular clinical situations.” Guidelines for diabetic ulcers and gangrene have been prepared and advocated abroad. However, foreign countries have a medical system that differs from that in Japan, and a wider variety of medical healthcare professionals may be engaged in the diagnosis and treatment for diabetes than are in Japan. For example, in some countries there are podiatrists, that is, professionals who perform diagnosis and treatment of disorders from the toes to the legs, in addition to orthopedists. The role of the podiatrist varies among countries, but they can also perform surgical procedures of the foot in the USA. Thus, the responsibilities and duties that doctors and other medical professionals should bear may differ between Japan and other countries. It is therefore unreasonable to directly apply overseas guidelines to Japan without taking such differences in medical organization into consideration. In Japan, the number of diabetic patients has increased markedly in recent years and consequently has led to an associated increase in the importance of diagnosis and treatment for complications related to diabetic skin ulcers and gangrene. Our aim was therefore to prepare guidelines for the management of diabetic ulcers/gangrene with emphasis on the diagnosis and treatment of dermatological symptoms. Of course, as diabetic ulcers/gangrene are local symptoms of diabetes, which is a systemic disease, it is not sufficient to focus only on such skin symptoms alone; rather, attention to the diabetes itself and its complications is always necessary. Clearly, it is also essential to manage diabetic patients in cooperation with a medical team dedicated to the diagnosis and treatment of diabetes and its complications. In addition, as factors that delay wound healing are constantly active on diabetic ulcers unlike acute wounds, a suitable approach towards potential exacerbating factors is necessary. For this reason, the present guidelines aim to serve as a tool to improve the quality of diagnosis and treatment for each individual patient, and furthermore to improve the level of care for diabetic ulcers in Japan by systematically presenting evidence-based recommendations for clinical judgments by incorporating these viewpoints.
2 POSITION OF THE GUIDELINES FOR THE DIAGNOSIS AND TREATMENT OF DIABETIC ULCERS AND GANGRENE
The committee for preparing these guidelines (Table 1) consists of members delegated by the Board of Directors of the Japanese Dermatological Association. The committee has met and produced written deliberations several times since October 2008 that consider the opinions of the Scientific Committee and the Board of Directors of the Japanese Dermatological Association, has drafted diagnosis and treatment guidelines,1 and started work on a revised edition in June 2013. These guidelines indicate the current standards for the diagnosis and treatment of various wounds and burns in Japan. However, patients have diverse individual backgrounds, such as differences in their underlying conditions, the extent of their symptoms and their complications. Therefore, physicians who provide diagnosis and treatment should determine a treatment plan for each patient, and the contents of the medical care provided are not required to completely agree with the present guidelines. These guidelines are not relevant for citation in lawsuits.
|
Chairperson: Hironobu Ihn Vice-chairperson: Takao Tachibana |
|
| Wounds in general |
Yuji Inoue Sakae Kaneko Hiroyuki Kanoh Yoichi Shintani Jun Tsujita Minoru Hasegawa Hideki Fujita Seiichiro Motegi Andres James Le Pavoux |
| Pressure ulcers |
Zenzo Isogai Ryokichi Irisawa Masaki Otsuka Takafumi Kadono Monji Koga Kuninori Hirosaki Hiroshi Fujiwara |
| Diabetic ulcers |
Masatoshi Abe Ryuta Ikegami Taiki Isei Hiroshi Kato Eiichi Sakurai Hideaki Tanizaki Takeshi Nakanishi Osamu Yamasaki |
| Connective tissue diseases and vasculitis |
Jun Asai Yoshihide Asano Takayuki Ishii Yohei Iwata Tamihiro Kawakami Masanari Kodera Manabu Fujimoto |
| Leg ulcers/varices |
Takaaki Ito Ryuichi Kukino Yasuko Sarayama Miki Tanioka Takeo Maekawa Hiroshi Yatsushiro |
| Burns |
Masahiro Amano Yoichi Omoto Masakazu Kawaguchi Keisuke Sakai Naotaka Doi Akira Hashimoto Masahiro Hayashi Naoki Madokoro Yuichiro Yoshino |
| Evaluation of evidence-based medicine | Takeshi Kono |
3 MAIN CHANGES IN THE SECOND EDITION
- The content has been updated by adding and collecting documents for all sections.
- We additionally included oral antibiotic treatment for bacterial infection of ulcers.
- We have added clinical questions (CQs) pertaining to imaging tests for diagnosing ischemia of the limbs.
- We have revised the titles of some CQs to conform to the actual clinical setting.
4 SPONSORS AND CONFLICTS OF INTEREST
All expenses required for drafting these guidelines have been borne by the Japanese Dermatological Association, and no aid or financial support has been provided by specific organizations, enterprises, or pharmaceutical companies. Furthermore, in the case that one of the aforementioned committee members participating in the drafting of these guidelines was involved in the development of a specific, relevant drug, that member abstained from determining to what degree the item in question was recommended. Aside from that, each committee member has no conflict of interest to disclose in the drafting of these guidelines.
5 COLLECTION OF EVIDENCE
Databases used: Medline, PubMed, Japana Centra Revuo Medicina Web and Cochrane Database of Systematic Reviews of all evidence-based medicine reviews. References obtained by manual search of each member were also added.
Search period: All searchable studies published between January 1980 and March 2016 were reviewed. Recently published studies of importance were added when considered appropriate.
Adoption criteria: Priority was placed on systematic reviews of randomized controlled trials (RCTs) and papers on individual RCTs. If they were not available, papers on cohort studies and case–control studies were adopted. Although some papers on case series studies were also used as references, published basic research studies were excluded.
6 CRITERIA FOR THE DETERMINATION OF EVIDENCE AND RECOMMENDATION LEVELS
The criteria described below were adopted in the “Guidelines for the Diagnosis and Treatment of Malignant Skin Tumors” edited by the Japanese Dermatological Association and were used as a reference for the evidence levels.
Evidence level classification:
I. Systematic reviews/meta-analysis.
II. One or more RCTs.
III. Non-RCTs (including before/after comparative studies with statistical analysis).
IVa. Analytical epidemiological studies (cohort studies).
IVb. Analytical epidemiological studies (case–control studies/cross-sectional studies).
V. Descriptive studies (case reports and case series studies).
VI. Opinions of special committees and individual experts.
The Minds Handbook for Clinical Practice Guideline Development 2014 was referenced for the recommendation levels.
Classification of recommendation levels and recommendation descriptions:
- Recommended.
- Proposed as one option.
If the recommendation level could not be determined, it was listed as “none,” which includes cases in which a clear recommendation could not be made.
- Treatment I is recommended for patient P (1A) (i.e., strong recommendation, based on strong evidence).
- Treatment I is proposed as an option for patient P (2C) (i.e., weak recommendation based on weak evidence).
- Treatment I is not proposed for patient P (2D) (i.e., weak recommendation based on very weak evidence).
- Treatment I is not proposed for patient P (1B) (i.e., strong recommendation based on moderate evidence).
7 REVIEW BEFORE PUBLICATION
Prior to the publication of these guidelines, the Annual Meetings of the Japanese Dermatological Association from 2012 to 2015 were used to present annual progress in drafting, to solicit opinions from association members, and to make necessary revisions.
8 PLANS FOR UPDATES
The present guidelines are scheduled to be updated in 3–5 years. However, if a partial update becomes necessary, it will be presented on the website of the Japanese Dermatological Association, as appropriate.
9 DEFINITIONS OF TERMINOLOGY
The terminology used in these guidelines was defined as indicated below based on the contents of review papers and textbooks in Japan. In addition, these partially quote the terminology list of the Terminology Committee (Chairman: Takao Tachibana) of the Japanese Society of Pressure Ulcers, and consideration was made for consistency within the guidelines.
Diabetes: Diabetes is caused by sustained, chronic elevation of blood glucose levels above the appropriate range due to insulin deficiency. It causes various tissue and organ disorders (complications), and is generally diagnosed according to the diagnostic criteria of the Japanese Diabetes Society.
Diabetic dermopathy: Skin disorders caused by pathological conditions in diabetic patients.
Peripheral arterial disease (PAD): PAD is a general term for peripheral arterial disorders including arteriosclerosis obliterans (ASO), but is often used synonymously with ASO because of its predominance. Recently, it has been shown to be closely involved not only in leg amputation due to gangrene but also in cardiovascular diseases and associated deaths.
Infection: A state in which bacteria have grown above the stage of colonization, which is a state in which bacteria are present but do not multiply on the ulcer surface, and the proliferative power of bacteria has surpassed the immune capacity of the host, interfering with wound healing.
Topical agents: Drugs used for local treatment through the skin or by application directly to the disease focus on the skin. These are prepared by compounding various active agents with a base.
Hammer toe: Toe deformity caused by impairment of flexion of the metatarsophalangeal joint and extension of interphalangeal joint.
Claw toe: Toe deformity due to flexion of the distal interphalangeal joints. Caused by impairment of the extensor aponeurosis.
Charcot's osteoarthropathy: Bone destruction caused by excessive use of a joint due to neuropathic impairment of nociception. Occurs mostly in joints distal to the ankle in diabetes.
Foot corn: Internally developing, localized hyperkeratosis induced by long-standing external stimulation.
Pressure ulcer: External force applied to the body reduces or arrests blood flow to the soft tissue between the bone and the skin surface. If this state persists for a certain period, the tissue sustains irreversible ischemic damage and develops into a pressure ulcer.
Pocket: A wound cavity extending beyond a skin defect. The tissue covering a pocket is called the cover wall or cover lid.
Design: An assessment tool for evaluating pressure ulcers introduced by the Japanese Society of Pressure Ulcers in 2002 consisting of seven items: (i) depth; (ii) exudate; (iii) size; (iv) inflammation/infection; (v) granulation tissue; (vi) necrotic tissue; and (vii) pocket. There are two types: one used for severity classification representing severe and mild using capital and lowercase letters, respectively, and the other used for the evaluation of patient progress by quantifying the healing process to allow monitoring. The latter type exists as the 2002 version and the 2008 revision, DESIGN-R, modified to provide a more accurate rating of severity as well as evaluation of the progression of pressure ulcers.
Bacterial colonization: A state of the mere presence of bacteria on the ulcer surface. The host immune capacity is balanced with the proliferative ability of the bacteria, and the birth and death of the bacteria are in equilibrium.
Contamination: A state in which bacteria are present on the ulcer surface but do not divide or proliferate.
Critical colonization: Conventionally, the microbial environment of the wound was previously classified into infected and aseptic states, but currently the two conditions are considered as existing along a continuum (the concept of bacterial balance). Specifically, infection of wounds is understood as continuous stages of contamination, colonization, and infection, and infection may occur depending on the balance between the bacterial burden on the wound and host resistance. Critical colonization is a stage between colonization and infection, but tilted more to infection with the number of bacteria exceeding that of colonization.
Biofilm: Bacteria that have colonized on the surface of a foreign body or in necrotic tissue may produce polysaccharides on their body surface. These polysaccharides gradually fuse and form a membrane-like structure, which envelops bacteria. This is called a biofilm. Bacteria within a biofilm are protected from most antibiotics and leukocytes, and so infection is likely to persist.
Ankle brachial pressure index (ABI): The value indicated as the ratio between the blood pressure measured in the leg (usually in the posterior tibial or dorsalis pedis artery) and upper arm (lower limb blood pressure/brachial blood pressure). Because it decreases with a decrease in peripheral leg blood pressure due to stenosis or obstruction of leg arteries, it is useful for the diagnosis of PAD. However, caution is needed in dialysis patients with marked sclerotic changes due to calcification of the peripheral arterial wall, as the ABI may be normal or elevated even when PAD is present. According to the Trans-Atlantic Inter-Society Consensus II (TASC II) international guidelines concerning PAD, the ABI is considered normal when it is 0.91 or more and 1.40 or less, and PAD is diagnosed when it is 0.90 or less. The American Diabetes Association (ADA) considers the ABI to be low when it is less than 0.9 and to be high when it is 1.3 or more in diabetic patients. Furthermore, in the 2011 update to the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines, ABI readings of 0.91 to 0.99 are considered borderline, with the normal range at 1.00 to 1.40. In outpatient care for diabetic patients in Japan, an ABI cut-off index that is slightly higher than usual (1.0) has been reported to be appropriate. Conversely, a meta-analysis indicated that normal values are in the range 1.11 to 1.40, while a higher mortality rate and event rate were found not only at values up to 0.9 and above 1.4, but in the range of 0.91 to 1.10 as well. A dedicated device for quick measurement of ABI (ABI/PWV) has become widely adopted, and false-normal values can be discerned by simultaneous measurement of the limb arterial pressures and pulse wave velocity (PWV). This examination can also be performed relatively easily in an outpatient setting without a dedicated device.
Trans-Atlantic Inter-Society Consensus II (TASCII): Guidelines concerning the diagnosis and treatment of PAD that were prepared with the participation of academic societies pertaining to the vasculature in Europe, the USA, Japan, Australia, and South Africa, and have gained international consensus. They include items related to the diagnosis and treatment of PAD complicating diabetic ulcers.
Peripheral arterial occlusive disease (PAOD): PAOD is a general term for PAD in which stenosis or obstruction occurs for some reason in limb arteries, causing circulatory disorders. It includes Buerger's disease and acute arterial obstruction as well as ASO, but it is often used synonymously with ASO or PAD because of their strong predominance.
Arteriosclerosis obliterans (ASO): A disease in which chronic stenosis or obstruction of limb arteries and consequent impairment of the limb blood flow are caused by arteriosclerosis due to dyslipidemia or similar conditions.
Toe brachial pressure index (TBI): The ratio between the toe blood pressure and the blood pressure of the upper arm (toe blood pressure/arm blood pressure). Because calcification is less likely to occur in the toe arteries than in lower leg vessels, the TBI may be less affected by calcification than the ABI. According to the TASC II standards, a TBI of at least 0.7 is normal, while values below are abnormal. Conversely, a TBI cut-off index of 0.6 or below has also been reported to be appropriate.
Transcutaneous oxygen pressure (TcPO2) (measurement): A non-invasive examination performed by using a probe at the skin surface to directly measure the oxygen diffusing from the cutaneous microvasculature in the cutaneous microcirculation. The cutaneous blood flow can be indirectly evaluated by understanding the blood flow and state of oxygenation in the cutaneous microcirculation. This is useful for evaluating the severity of ischemic limbs, predicting outcomes, and determining an incision site. In the TASC II standard, a value under 30 mmHg is diagnosed as critical limb ischemia (CLI). It is often reported that healing can be expected via conservative treatment for ulcerative lesions to ischemic limbs when the TcPO2 value is at least 40 mmHg, but some reports use an outcome predictor value of at least 30 mmHg. The cut-off value at which conservative treatment becomes difficult is often considered 10–20 mmHg. Conversely, it has also been reported that when the affected limb of a patient with a TcPO2 value in the range of 20–40 mmHg inclusive while in a supine position is raised at an angle of 30–45 degrees for 3 min, if the resulting measurement value decreases by less than 10 mmHg from the initial measurement value, there is an 80% cure rate, whereas if the value decreases by more than 10 mmHg, an 80% cure rate cannot be expected. Thus, the cut-off value has not been delineated. In addition, there are multiple reports that it is possible to avoid excessive incisions by determining an appropriate incision site at an ischemic limb by measuring TcPO2 at a number of locations, with a value of at least 20 mmHg indicating that healing can be expected at the incision surface. Conversely, it has also been reported that if the TcPO2 value improves by at least 10 mmHg by inhaling oxygen (100% O2 for 10 min), as long as the initial measurement value is greater than 10 mmHg, healing of the area of resection can be anticipated.
Skin perfusion pressure (SPP): The SPP, measured by the laser Doppler technique, allows the evaluation of the cutaneous microcirculation relatively easily. It is considered to be closely correlated with the toe pressure (TP) and is measurable even in patients in whom the TP cannot be measured (toe amputees or with toe ulcer patients). It is considered useful for detecting severe PAD and for predicting prognoses after surgery for ulcerative lesions and for vascular reconstruction. There is a non-randomized trial indicating that even in cases of CLI, an SPP of at least 30 mmHg indicates that an improvement of 80% can be expected via conservative treatment, while wound treatment is difficult when SPP is below this value.
Meanwhile, although at a lower evidence level, there are multiple reports of an outcome predictor cut-off value of 40 mmHg. In addition, there are a number of reports that measuring SPP before and after vascular reconstruction in a severely ischemic limb is useful for predicting the wound-healing outcome, and the cut-off value is considered at least 30 to 40 mmHg.
Digital subtraction angiography (DSA): Angiography in which images of structures other than the objects of interest can be deleted by digital image processing. The accuracy of the diagnosis can be enhanced by eliminating tissues such as bones.
Computed tomography angiography (CTA): Angiography using computed tomography (CT).
Angiography: The procedure of obtaining X-ray images after injecting a contrast agent into blood vessels.
Magnetic resonance angiography (MRA): Angiography by magnetic resonance imaging (MRI). A contrast agent is often used for examining peripheral arteries.
Fontaine classification: A scale for the functional classification of the collateral circulation in chronic arterial occlusive disease based on information obtained by medical interviews. Consists of stages I–IV. All diabetic ulcers/gangrenes associated with chronic arterial occlusive disease are classified as stage IV.
| Grade | Symptoms |
|---|---|
| Stage I | Asymptomatic, incomplete blood vessel obstruction |
| Stage II | Mild claudication pain in limb |
| Stage IIA | Claudication at a distance >200 m |
| Stage IIB | Claudication at a distance <200 m |
| Stage III | Rest pain, mostly in the feet |
| Stage IV | Necrosis and/or gangrene of the limb |
Critical limb ischemia (CLI): A condition corresponding to Fontaine stage III or IV.
Moist wound healing: A method of maintaining the wound surface in a moist environment. It retains polynuclear leukocytes, macrophages, enzymes, and cell growth factors found in exudates at the wound surface. Such an environment also promotes autolysis, contributes to debridement, and does not interfere with cell migration.
Semmes–Weinstein monofilament test: A testing technique performed by applying a nylon filament to the skin with pressure and examining whether a sensation is perceived. Sensory nerve disorders can be evaluated by semiquantitative measurements of pain and pressure sensation using monofilaments of differing diameters. The 5.07 (10 g weight) monofilament is often used for the diagnosis of diabetic neuropathy.
| Evaluation | Filament/pressure conversion value (g) |
|---|---|
| Normal | 1.65–2.83: green/0.008–0.06 |
| Reduced sensitivity to touch | 3.22–3.62: blue/0.172–0.217 |
| Reduced protective sensation | 3.84–4.31: purple/0.445–2.35 |
| Loss of protective sensation | 4.56–6.65: red/4.19–279.4 |
| No response | No response to 6.65 |
Foot care: A series of actions for the care of one's feet aimed at load relief, pressure reduction, mitigation of pain, and cleaning for the protection of the foot and prevention of wounds.
Debridement: A therapeutic action to clean the wound by removing necrotic tissue, foreign material, senescent cells that no longer react to stimulation by promoters of wound healing such as growth factors, as well as foci of bacterial infection, which are often associated with the above. Methods include: (i) autolytic debridement induced by occlusive dressing; (ii) mechanical debridement (e.g., wet-to-dry dressing, high-pressure washing, hydrotherapy, and ultrasonic washing); (iii) debridement using proteolytic enzymes; and (iv) surgical debridement.
Surgical therapy: Surgical treatment, surgical debridement, and invasive treatments of subcutaneous pockets. The distinction between surgical treatments and surgical debridement is unclear.
Dressing materials: Modern wound dressing materials for creating moist environment for wounds. Conventional gauze is excluded regardless of whether it is sterile.
Occlusive dressing: All dressing methods used to avoid drying of wounds for moist wound healing are called occlusive dressing. This is a collective term for dressings using modern wound dressing materials other than conventional gauze dressing.
Wound dressing materials: Wound dressing materials can be classified into dressing materials (modern dressing materials) and medical materials such as gauze (classic dressing materials). The former are medical materials that provide optimal conditions for wound healing by maintaining a moist environment and must be used selectively depending on the state of the wound and the amount of exudates. Gauze allows drying of the wound and cannot maintain a moist environment if exudate levels are insufficient. Medical materials other than conventional gauze that provide an optimal environment for wound healing by covering the wound and maintaining moisture may generally be called wound dressing materials or dressing materials.
Wound bed preparation: Management of the wound surface environment to promote wound healing. Specifically, it consists of removing necrotic tissue, reducing bacterial load, preventing wound drying, controlling excessive exudates, and treating pockets and wound margins.
Negative pressure wound therapy (NPWT): A type of physical therapy. The wound is maintained in a closed environment, and suction is applied to adjust the target pressure to 125–150 mmHg. This therapy eliminates bacteria and exotoxins released from bacteria, promotes vascularization of granulation tissue, and alleviates edema.
Nutrition support team (NST): The Japan Council for Nutritional Therapy (JCNT) calls nutritional management performed appropriately for individual patients and for the treatment of individual disorders “nutrition support,” and defines a team of several professionals including a physician, nurse, pharmacist, managerial dietician, and clinical laboratory technician as the NST.
Hyperbaric oxygen therapy: A treatment intended to elevate the arterial dissolved oxygen concentration and relieve hypoxia of skin tissue by placing the patient in an environment with an oxygen concentration higher than that at atmospheric pressure.
Callosity: Externally developed, localized hyperkeratosis induced by long-term external stimulation.
Foot bathing: Immersing the leg rather than the whole body in warm water and washing it while warming it.
“Physical therapy”: Treatment performed by applying stimulation to the body using physical means, which include physical energy, such as heat, water, light, ultrashort waves, electricity, ultrasound, vibration, pressure, and traction. Thermotherapy, cryotherapy, hydrotherapy, phototherapy, ultrashort wave therapy, electric stimulation therapy, ultrasound therapy, negative-pressure therapy, hyperbaric oxygen therapy, and traction therapy are variations of physical therapy. These are performed to mitigate pain, promote wound healing, and increase the elasticity of tissues such as muscles and ligaments. “Physical therapy” is used as a general term for all these therapies, and the means for the treatment are conventionally called “physical agents” to avoid confusion.
Lavage: Removing chemical irritants, sources of infection, and foreign material from the skin or wound surface using the pressure lysing effect of a liquid. Lavage may be performed using physiological saline, tap water, or either saline or tap water combined with a surfactant such as soap or detergent. The effect of lavage may be derived from the flow volume or hydraulic pressure.
10 DEFINITION OF CONDITIONS
Of the diabetic skin disorders observed in diabetic patients, chronic or progressive ulcerating or necrotic lesions based on diabetic neuropathy, PAD, or both are defined as diabetic ulcers/gangrene. For these lesions, reversible changes are defined as diabetic ulcers, while necrotized, non-reversible changes as gangrene. As a matter of course, ulcerative or necrotic lesions due to other conditions (collagen disease, leg varices, malignant neoplasms, etc.) are excluded.
11 WOUND HEALING PROCESS IN DIABETES AND ITS OBSTACLES
The wound healing process in the skin can be divided into three periods: (i) inflammation, (ii) cell proliferation, and (iii) maturation/reconstruction. In each of these periods of the wound healing process there are changes to the morphology and the functional expression and inhibition of a variety of cells, and several growth factors and proteases contribute in a complex manner. Understanding these mechanisms is extremely important for selecting repair factors suitable for treatment. In healthy people, this wound healing process advances smoothly, and wounds heal rapidly (acute wounds). In diabetic patients, however, the healing mechanism is inhibited by various inhibitory factors such as neuropathy, peripheral vascular disorders, regional hyperglycemia, and reduced activity of the patient, delaying wound healing (chronic wounds). In diabetes, a hypoxic state occurs readily on the dermal level. Under hypoxic conditions, fibroblast-derived matrix metalloproteinase (MMP)-1 with a collagen-decomposing activity may increase, hampering wound healing.2 Hypoxia promotes infection of lesions, which further delays wound healing.3, 4 Hyperglycemia also affects the osmotic pressure and inhibits granulation in skin ulcers. Moreover, basic research has also disclosed on the genetic level that hyperglycemia is involved in delayed wound healing.5 To address this delay, it is necessary to promote wound healing using appropriate repair factors and by eliminating exacerbating factors. Basic research using model mice has also demonstrated that improving the wound healing mechanism leads to the acceleration of healing in diabetic ulcer models.6-8 In other countries in recent years there have been numerous reports on the utility of cultured skin and platelet-derived growth factor (PDGF), and these are garnering attention as new treatment strategies in Japan as well.9, 10 Furthermore, there have been recent reports on the utility of autologous platelet-rich plasma (PRP), which is attracting attention as it is a relatively simple procedure. In this therapeutic method, platelets are isolated and concentrated from peripheral blood drawn from the patient and then applied to the ulcer, which is believed to promote wound healing through the effects of growth factors present in the PRP.11
However, in the actual treatment for diabetic ulcers, part of the difficulty in healing results not only from poor control of blood glucose levels but also from the involvement of many exacerbating and repairing factors. For this reason, physicians diagnosing and treating diabetic skin ulcers/gangrenes must approach these conditions with a wealth of knowledge about wound healing and a thorough ability to observe dermatological symptoms.
12 APPROACHES TO DAIAGNOSIS AND TREATMENT
Diabetic ulcers/gangrene often derive from peripheral neuropathy, which is a complication of diabetes.9, 10, 12-14 Diabetes is often complicated by hyperlipidemia and by circulatory disorders of the limbs (PAD) resulting from arteriosclerotic stenosis or obstruction of peripheral arteries resulting from hyperlipidemia, and diabetic ulcers/gangrene caused by circulatory insufficiency resulting from PAD accounts for approximately 25% of all cases. Both peripheral neuropathy and PAD are involved in some cases. Moreover, ulcers may be caused or exacerbated by the additional involvement of infection in addition to the above factors.
In diabetic neuropathy, impairment of motor neurons causes atrophy of the muscles they control, leading to toe or foot deformities such as hammer toe and claw toe. In addition, an increase in the bone blood flow due to autonomic neuropathy causes a decrease in bone mass, and if this is combined with a repeated stimulus resulting from continuing to walk without any sensation of pain due to sensory neuropathy, a foot deformity called Charcot's foot (joint) occurs. Because such deformities abnormally increase the pressure exerted at particular sites of the foot, there is an elevated risk of skin disruption leading to ulcers. In addition, patients fail to notice foot corns, trauma, burns, and skin infections due to reduced protective sensation caused by sensory neuropathy, leading to the development and exacerbation of ulcers. PAD itself does not frequently cause ulcers, but once an ulcer develops, it prolongs the healing process and even increases the risk of amputation being required at major joints due to gangrene.15
Because of these diabetic complications, the condition of a diabetic ulcer is often not expected to improve solely through treatment with conventional topical agents for ulcers, and so treatments for complications are frequently required. Because treatments vary depending on the extent of involvement of different complications in the pathogenesis of ulcers, understanding the presence and severity of diabetic neuropathy and PAD is important for not only diagnosis but also the determination of a treatment plan. This approach is also regarded as a basic principle for managing diabetic ulcers/gangrene in many guidelines developed abroad.10, 16, 17
As mentioned in the previous section, the mechanism of wound healing is inhibited by various factors in diabetic ulcers, which represent a chronic wound state. A basic principle for treating chronic wounds is to promptly convert it to an acute wound by eliminating factors that interfere with the mechanism of wound healing, which is also important for treating diabetic ulcers. Indeed, the prevalence of ulcers in diabetic patients is reported to be approximately 15%,18 although it varies among reports. Diabetic patients tend to exhibit decreased in daily living activities due to ulcers and this further exacerbates the diabetes, setting off a downward spiral.
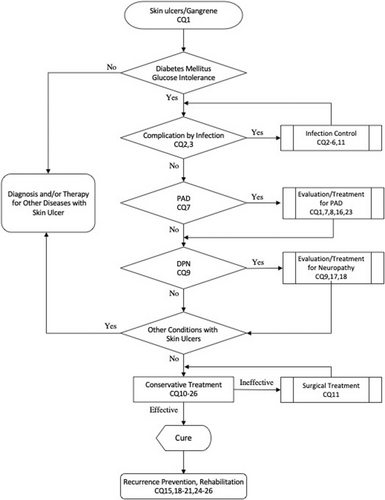
In the present guidelines, the basic concept of managing diabetic ulcers/gangrene is to first diagnose/assess these diabetic complications and then to appropriately combine their treatments with the diagnosis, assessment, and treatment of the ulcer/gangrene itself. An algorithm (Figure 1) and CQs were established based on this concept as signposts for real-life diagnosis and treatment.
13 SUMMARY OF CQS
Table 2 details the CQs and their associated recommendation levels and descriptions.
| Clinical question | Recommendation level | Description of recommendation |
|---|---|---|
| 1. Diagnosis of diabetic ulcers/gangrene | ||
| CQ1: Are the Wagner Grading System and University of Texas Diabetic Wound Classification useful as clinical severity scales to be used for the everyday management of diabetic ulcers/gangrene? |
1C: Wagner Grading System 1B: University of Texas Diabetic Wound Classification |
Evaluating the severity of diabetic ulcers/gangrene primarily using the Wagner Grading System is recommended (1C). Evaluating severity using the University of Texas Diabetic Wound Classification is also recommended (1B). |
| 2. Control of complication by infection | ||
| CQ2: How should bacterial infection of diabetic ulcers be diagnosed? | 1D | To diagnose bacterial infection of diabetic ulcers, we recommend making judgments based on a comprehensive evaluation of clinical findings, blood test results, imaging findings, and results of bacterial cultures (1D). |
| CQ3: Are imaging findings useful for the diagnosis of osteomyelitis? | 1A: Magnetic resonance imaging (MRI), plain radiography, bone scintigraphy, labeled white blood cell scintigraphy | While it is possible to predict osteomyelitis from bone exposure and positive findings in the probe-to-bone test, diagnostic imaging (particularly MRI) is recommended for a more accurate diagnosis (1A). Among other diagnostic imaging modalities, plain radiography (1A), bone scintigraphy (1A), and labeled white blood cell scintigraphy (1A) are recommended. |
| CQ4: What topical agents are useful for controlling bacterial infection of diabetic ulcers? |
1A: Cadexomer iodine, silver sulfadiazine, povidone iodine sugar 1C: Povidone iodine gel 1D: Iodoform, iodine ointment 2A: Ointments containing antibiotics (we propose not using them) |
The use of cadexomer iodine, silver sulfadiazine, and povidone iodine sugar is recommended (1A), as is the use of povidone iodine gel (1C), iodoform (1D), and iodine ointment (1D), for controlling bacterial infection of mild diabetic ulcers (1A). We propose that ointments containing antibiotics not be used (2A), as sufficient grounds for their use have not been established. |
| CQ5: Is systemic administration of an antibacterial drug useful for the control of local acute infection of diabetic ulcers? | 1A: Amoxicillin/clavulanate, ampicillin/sulbactam, imipenem, ofloxacin, clindamycin, cefazolin, cephatolexin, cephalexin, daptomycin, vancomycin + ceftazidime, piperacillin/tazobactam, moxifloxacin, linezolid | Systemic administration of antibacterial drugs such as amoxicillin/clavulanate (1A), ampicillin/sulbactam (1A), imipenem (1A), ofloxacin (1A), clindamycin (1A), cefazolin (1A), cephatolexin (1A), cephalexin (1A), daptomycin (1A), vancomycin+ceftazidime (1A), piperacillin/tazobactam (1A), moxifloxacin (1A), or linezolid (1A) is recommended for infected moderate to severe diabetic foot ulcers. |
| CQ6: How long should systemic administration of antibacterial drugs be continued for the treatment of osteomyelitis? |
1A: At least 2–4 weeks of antibacterial drug administration after removal of infected bone 1D: At least 6 weeks of antibacterial drug administration if elimination of infected bone was insufficient |
For osteomyelitis associated with diabetic foot infection, we recommend administering antibacterial drugs for at least 2–4 weeks after removal of infected bone (1A). If the elimination of infected bone was insufficient, at least 6 weeks administration of antibacterial drugs is recommended (1D). |
| 3. Severe ischemia/peripheral arterial disease (PAD) | ||
| CQ7: How should limb ischemia be diagnosed during the initial outpatient examination? |
1A: Subjective and objective findings, medical interview regarding smoking history 1C: Ankle brachial pressure index (ABI), toe brachial pressure index (TBI), skin perfusion pressure (SPP), transcutaneous oxygen tension (TcPO2) measurement |
When evaluating ischemic symptoms of the extremities during outpatient diagnosis and treatment, we recommend measuring the ABI (1C), TBI (1C), SPP (1C), and TcPO2 (1C). In addition, we recommend palpation to confirm a weakened or absent peripheral arterial pulse, and a decrease in skin temperature (1A), as well as a detailed inquiry into the patient's smoking history and the presence of subjective symptoms such as numbness and coldness (1A). |
| CQ8: What imaging tests are useful for a detailed investigation when limb ischemia is suspected during the initial outpatient examination? | 1A: Ultrasonography, computed tomography angiography (CTA), magnetic resonance angiography (MRA) | For imaging tests evaluating limb ischemia during the initial outpatient examination, we recommend minimally invasive tests such as Ultrasonography (1A) CTA and (1A) MRA. In order to improve the diagnosis rate, it is preferable to combine these as appropriate, but since there are relatively few facilities that can perform all the above tests, whether to perform them should be considered based on the patient's condition. |
| 4. Neuropathy/foot deformation | ||
| CQ9: What examinations are useful for the diagnosis of diabetic peripheral neuropathy? |
1A: Monofilament method 1C: Tuning fork method, Achilles tendon reflex |
A sensory examination using the Semmes–Weinstein monofilament test (1A), testing the sensation of vibrations using the tuning fork method (1C), and the Achilles tendon reflex test (1C) are useful for the clinical diagnosis of peripheral neuropathy due to diabetes, and all are recommended. To improve the diagnosis rate, these are preferably combined, as appropriate. |
| 5. Ulcer treatment | ||
| CQ10: How long should the observation period be for evaluating the usefulness of conservative treatment in diabetic ulcer patients? | 1C | We recommend evaluating the usefulness of conservative treatment for diabetic ulcers in the chronic phase within a maximum of 4 weeks and to compare it with other treatments when appropriate. However, it is desirable to examine diabetic ulcers in the acute period at least once a week. |
| CQ11: Is surgical debridement useful for removing necrotic tissue from a diabetic ulcer? | 1A | If the patient's overall condition permits it, we recommend performing surgical debridement as the initial debridement to remove necrotic tissue and crust adhering to the ulcer, and keratinized material in and around the ulcer to control infection. However, if there is underlying peripheral arterial disease (PAD), there are cases when symptomatic improvement cannot be anticipated from surgical debridement, but rather increased severity of ulcers/gangrene can be expected. Therefore, surgical debridement should be performed carefully at the peripheral areas of the limbs, including limb amputations particularly when exhibiting osteomyelitis. |
| CQ12: What topical agents should be used for diabetic ulcers with no signs of infection? |
<Wounds with appropriate to deficient exudates> 1A: Trafermin, prostaglandin E1, tretinoin tocopherol <Wounds with excessive exudates or marked edema> 1A: Bucladesine sodium |
As topical agents for diabetic ulcers, we recommend using trafermin (1A), prostaglandin E1 (1A), or tretinoin tocopherol (1A) for wounds with appropriate or deficient exudates. The use of bucladesine sodium (1A) is recommended for wounds with excessive exudates or marked edema. |
| CQ13: What dressing materials should be used for diabetic ulcers with no signs of infection? |
<Wounds with appropriate to deficient exudates> 1A: Hydrocolloids 1B: Hydrogels, polyurethane foam <Wounds with excessive exudates or marked edema> 1C: Alginate dressings 2C: Hydrofiber® |
For wounds with appropriate/deficient exudates, we recommend using hydrocolloids (1A), hydrogels (1B), or polyurethane foam (1B). For wounds with excessive effusion or marked edema, we recommend the use of calcium sodium alginate dressings (1C). In addition, we propose the use of Hydrofiber® (2C) for wounds with excessive effusion or marked edema. |
| CQ14: Is negative-pressure wound therapy (NPWT) useful for the treatment of diabetic ulcers? | 1A | We recommend performing NPWT for diabetic ulcers. If these are infected, cautious observation is required |
| CQ15: Are weight-bearing orthoses useful for the treatment and prevention of diabetic ulcers? |
1A: Treatment 1A: Prevention |
We recommend using weight-bearing orthoses to resolve ulcers occurring due to compression by dispersing pressure. Because they are also considered effective for preventing compression, their use is recommended. |
| CQ16: What drugs are useful for the treatment of diabetic ulcers due to vascular disorders? |
1A: Dalteparin 1C: Argatroban, Lipo-PGE1, PGE1 1D: Sarpogrelate hydrochloride, cilostazol, beraprost sodium |
Among antithrombotic drugs, we recommend administering dalteparin (1A), argatroban (1C), sarpogrelate hydrochloride (1D), or cilostazol (1D). Among vasodilators, we recommend administering PGE1 (1C), Lipo-PGE1 (1C), or beraprost sodium (1D). |
| CQ17: What drugs are useful for the treatment of diabetic ulcers due to neuropathy? |
1A: Lipo-PGE1 1C: PGE1, beraprost sodium 1D: Dalteparin |
We recommend administering the vasodilator Lipo-PGE1 (1A), PGE1 (1C), or beraprost sodium (1C). We recommend administering the antithrombotic drug dalteparin (1D). |
| CQ18: What drugs are useful against diabetic neuropathy? |
<Painful diabetic neuropathy> 1A: Amitriptyline hydrochloride, duloxetine, gabapentin, pregabalin, mexiletine 1B: Nortriptyline <Diabetic neuropathy> 2A: Epalrestat |
For painful diabetic neuropathy, we recommend administering amitriptyline hydrochloride (1A), or nortriptyline (1B), tricyclic antidepressants: duloxetine (1A), a serotonin noradrenaline reuptake inhibitor (SNRI); gabapentin (1A) or pregabalin (1A), Ca channel alpha2delta ligands; or mexiletine (1A), an antiarrhythmic agent. For diabetic neuropathy in general, we propose the administration of epalrestat (2A) as an option. |
| CQ19: Is glycemic control useful for improving the cure rate of diabetic ulcers? | 1C | Blood sugar control is recommended as it reduces local factors inhibiting wound healing and leads to improvement in the mechanism of wound healing. |
| CQ20: Does improving the nutritional status of diabetic patients promote the healing of diabetic ulcers? | 1B | Improving the nutritional status under the guidance of a specialist in nutrition is recommended. |
| CQ21: Can hemodialysis cause diabetic ulcers or act as a factor delaying healing? | 1C | We recommend managing diabetic patients undergoing dialysis therapy with attention to the possibility that hemodialysis can affect the development of skin ulcers and delay their healing. |
| 6. Selection of other treatment methods and preventing recurrence | ||
| CQ22: Is hyperbaric oxygen therapy useful for the treatment of diabetic ulcers? | 1A | Hyperbaric oxygen therapy is recommended for the treatment of diabetic ulcers. However, not many facilities or institutions are equipped for this treatment. |
| CQ23: Is low-density lipoprotein (LDL) apheresis useful for the treatment of diabetic ulcers? | 1C | LDL apheresis is recommended, because it can be expected to produce a therapeutic effect in diabetic ulcers complicated by major vascular disease. |
| CQ24: Can the occurrence and exacerbation of diabetic ulcers be prevented by treating tinea pedis or toenail tinea unguium? | 1A | Treatment for tinea pedis or toenail tinea unguium is recommended to prevent the occurrence and exacerbation of diabetic ulcers. |
| CQ25: Is treatment for calluses or foot corns useful for preventing diabetic ulcers? | 1A | We recommend taking appropriate measures such as shaving to prevent calluses and foot corns in diabetic patients. |
| CQ26: Is patient education (including whole-body and foot bathing) useful for the treatment of ulcers in diabetics? | Patient education (self-learning) through diabetes classes is useful as part of the treatment and is recommended. | |
13.1 Diagnosis of diabetic ulcers/gangrene
13.1.1 CQ1: Are the Wagner Grading System and University of Texas Diabetic Wound Classification useful as clinical severity scales to be used for the everyday management of diabetic ulcers/gangrene?
Description of recommendation: Evaluating the severity of diabetic ulcers/gangrene primarily using the Wagner Grading System is recommended [1C]. Evaluating severity using the University of Texas Diabetic Wound Classification is also recommended [1B].
Recommendation level:
[1C] Wagner Grading System.
[1B] University of Texas Diabetic Wound Classification.
- Concerning the Wagner Grading System (Table 3), there is one cohort study19 and so the evidence level is IVa and the recommendation level is 1C. It is considered an important grading method as it has been widely used and has gained international consensus. Furthermore, it has served as a standard for the development of new severity classifications. There is a non-randomized comparative study and a cohort study20, 21 examining the University of Texas Diabetic Wound Classification (Table 4), and so the evidence level is III–IVa and the recommendation level is 1B. In addition, while it is more likely to reflect the actual severity than the Wagner Grading System, it has a large number of evaluation items and is relatively complex.
- The Wagner Grading System19 indicated in Table 3 classifies diabetic ulcers/gangrene into five grades according to the depth of ulcer and the presence of osteomyelitis and gangrene. Because it is simple and easy to understand, it is widely used primarily in Western countries, but its validity in diabetic patients in Japan has not been evaluated. In addition, the presence and severity of complication by PAD are not included in the evaluation criteria of the Wagner Grading System. Therefore, when using this system, it is necessary to evaluate the severity by taking into consideration the condition of the ulcer, state of peripheral angiopathy or neuropathy, and the patient's general condition including complications.
- The University of Texas Diabetic Wound Classification20 indicated in Table 4 classifies diabetic ulcers of the leg into four grades according to their depth in underlying tissues, and subclassifies each grade into four stages according to the presence of infection and ischemia. The modified version21 simplifies the subclassification with infection and ischemia. Because this system includes the states of infection and ischemia as evaluation criteria, it is more likely to reflect the actual severity than the Wagner Grading System. However, as it has a large number of evaluation items and is somewhat complex, it may be somewhat inconvenient for use at outpatient clinics.
- As clinical severity scales for diabetes, a number of new criteria have been proposed including S(AD)SAD,22 SINBAD,23 PEDIS,24 and DUSS,25 but none has gained international consensus. In addition, as all these classifications are criteria for evaluating severity including the patient's general condition, they are insufficient as evaluation criteria strictly for the state of the ulcer surface itself. These therefore impede their use as standards for selecting localized treatments for ulcers such as topical agents.
- In the evaluation of ulcers for their management, the Japanese Society of Pressure Ulcers has proposed the DESIGN assessment tool, consisting of the depth, exudates, size, inflammation/infection, granulation tissue, necrotic tissue, and pocket.26 As an evaluation method of the local state of diabetic ulcers, it is possible to use tracking of ulcer progress using DESIGN as a standard for selecting localized treatments, and can be additionally used as appropriate.
- There have also been reports on a risk classification by the International Working Group on the Diabetic Foot (IWGDF), which incorporates neurological findings for diabetic foot lesions,27 and the Kobe classification incorporating the presence of infection.28
| Grade 0 | After ulcer healing or prior to ulcer occurrence |
| Grade 1 | Superficial ulcer: extends through all layers of skin but does not extend subcutaneously |
| Grade 2 | Ulcer reaching tendon or muscle but not bone, with no abscess formation found |
| Grade 3 | Ulcer extending deeper with cellulitis or abscess; osteomyelitis often occurs as well |
| Grade 4 | Limited (forefoot) gangrene |
| Grade 5 | Gangrene of a large portion (at least 2/3) of the foot |
| Grade | ||||
|---|---|---|---|---|
| 0 | I | II | III | |
| A | Pre- or postulcerative lesion completely epithelialized | Superficial wound, not in-volving tendon, capsule, or bone | Wound penetrating to tendon or capsule | Wound penetrating to bone or joint |
| B | Pre- or postulcerative lesion, completely epithelialized with infection | Superficial wound, not in-volving tendon, capsule, or bone with infection | Wound penetrating to tendon or capsule with infection | Wound penetrating to bone or joint with infection |
| C | Pre- or postulcerative lesion, completely epithelialized with ischemia | Superficial wound. not in-volving tendon, capsule, or bone with ischemia | Wound penetrating to tendon or capsule with ischemia | Wound penetrating to bone or joint with ischemia |
| D | Pre- or postulcerative lesion, completely epithelialized with infection and ischemia | Superficial wound, not in-volving tendon, capsule, or bone with infection and ischemia | Wound penetrating to tendon or capsule with infection and ischemia | Wound penetrating to bone or joint with infection and ischemia |
13.2 Control of complication by infection
13.2.1 CQ2: How should bacterial infection of diabetic ulcers be diagnosed?
Description of recommendation: To diagnose bacterial infection of diabetic ulcers, we recommend making judgments based on a comprehensive evaluation of clinical findings, blood test results, imaging findings, and results of bacterial cultures.
Recommendation level: 1D.
- To diagnose infection of diabetic ulcers, it is essential to make judgments based on a comprehensive evaluation of clinical findings, blood test results, imaging findings, and results of bacterial cultures. Relevant reports are limited to expert opinions, and so the evidence level is VI and the recommendation level is 1D.
- Although there are two clinical comparative studies concerning the diagnosis of infection of diabetic ulcers and bacterial cultures,29, 30 these are not reports on the diagnosis of infections in general.
- For the general diagnosis of infections, the key is whether there are findings indicating inflammation such as reddening around the ulcer, swelling, pus discharge, exudates, odor, a local hot sensation, and tenderness. Patients may lack subjective symptoms because of neuropathy. In addition, while inflammatory findings in blood tests (white blood cell count, C-reactive protein [CRP], erythrocyte sedimentation rate) are useful, an increase in white blood cells or a CRP-positive result may not be observed despite the presence of deep infection.31
- The severity grading scales for diabetic foot infections according to the Infectious Disease Society of America (IDSA) and the International Working Group on the Diabetic Foot (IWGDF) base their classifications on the range and depth of local infection and the presence of systemic symptoms, as indicated in Table 5, and are useful as these have been reportedly correlated with clinical outcomes.32
- An ulcer depth of at least 3 mm together with an inflammatory response (CRP of 3.2 mg/dL or blood sedimentation rate of at least 60 mm/h) has a high sensitivity for diagnosing early-stage osteomyelitis.33
- Plain radiography may reveal no bone changes in early stages of osteomyelitis, but plain radiography, CT, and MRI are useful for the evaluation of deep soft tissue infections and osteomyelitis, and they present gas images in gas gangrene, therefore patients should be referred to medical facilities capable of CT or MRI when deemed necessary.
- Bacterial cultures of samples from infected wounds and susceptibility testing are necessary for appropriate antibiotic therapy. Samples may be obtained by swabbing, curettage, aspiration, or biopsy, but samples from deeper tissues are more reliable.30, 34 The most important pathogenic microorganisms are primarily aerobic Gram-positive cocci such as Staphylococcus aureus (S. aureus) and β-hemolytic streptococci, but Gram-negative or anaerobic bacteria also frequently cause infection and these species are often detected simultaneously35-37 Samples for bacterial cultures should ideally be collected after debridement, and cultures for both aerobic and anaerobic species should be performed when possible.38, 39 During this process, it is important to understand the concept of bacterial balance, including colonization, contamination, and critical colonization, which represent states of the host and the bacteria at an infected wound. In addition, antibiotics are generally ineffective against bacteria contained in a biofilm.
| IDSA | IWGDF | Symptoms |
|---|---|---|
| No infection | 1 | Ulcer with no pus or inflammation |
| Mild symptoms | 2 | Erythema/cellulitis within 2 cm of the ulcer periphery extending to the skin and shallow subcutaneous tissue without systemic symptoms |
| Moderate symptoms | 3 | Erythema/cellulitis exceeding 2 cm of the ulcer periphery, with inflammation spreading to deep subcutaneous tissue, gangrene, muscles, bones, and joints |
| Severe symptoms | 4 | Systemic symptoms (fever, tachycardia, hypotension, confusion, nausea, erythrocyte proliferation, acidosis, hyperglycemia, azotemia |
- Abbreviations: IDSA, Infectious Disease Society of America; IWGDF, International Working Group on the Diabetic Foot.
13.2.2 CQ3: Are imaging findings useful for the diagnosis of osteomyelitis?
Description of recommendation: While it is possible to predict osteomyelitis from bone exposure and positive findings in the probe-to-bone test, diagnostic imaging (particularly magnetic resonance imaging [MRI]) is recommended for a more accurate diagnosis (1A). Among other diagnostic imaging modalities, plain radiography (1A), bone scintigraphy (1A), and labeled white blood cell scintigraphy (1A) are recommended.
Recommendation level: [1A] MRI, plain radiography, bone scintigraphy, labeled white blood cell scintigraphy.
- There are three meta-analyses concerning the diagnosis of osteomyelitis.40-42 Among imaging examinations, MRI is the most reliable modality; its evidence level is I and its recommendation level is 1A. However, MRI cannot be performed as a routine examination at all medical facilities as those that can perform the procedure are limited. In addition, plain radiography, bone scintigraphy, and labeled white blood cell scintigraphy also exhibit comparatively high diagnostic sensitivity and specificity, and so their evidence level is I and their recommendation level is 1A.
- Osteomyelitis can also be diagnosed based on clinical findings. For example, bone exposure and a positive probe-to-bone test (the tip of the probe hits the bone at the ulcer floor) can be used for diagnosis.43, 44
- Bone exposure and a positive probe-to-bone test for the diagnosis of osteomyelitis have a diagnostic sensitivity of 60% and a specificity of 91%.40, 41 Among imaging modalities, MRI, plain radiography, bone scintigraphy, and labeled white blood cell scintigraphy have been evaluated, and their sensitivity and specificity were 90% and 79%, 54% and 68%, 81% and 28%, and 74% and 68%, respectively.40, 41
- The meta-analysis on fluorodeoxyglucose (FDG)-positron emission tomography (PET) for diabetic osteomyelitis has a somewhat low number of analyses, but the diagnostic sensitivity was 74% and the specificity was 91%, and it is considered useful in conjunction with another imaging modality such as MRI.42 However, it is not covered by the Japanese National Health Insurance program. In general, caution is needed in cases of hyperglycemia as there may be evidence of non-specific accumulations.
- A definitive diagnosis of osteomyelitis can be made by bone biopsy, but the examination is invasive and may spread the infection.
13.2.3 CQ4: What topical agents are useful for controlling bacterial infection of diabetic ulcers?
Description of recommendation: The use of cadexomer iodine, silver sulfadiazine, and povidone iodine sugar is recommended (1A), as is the use of povidone iodine gel (1C), iodoform (1D), and iodine ointment (1D), for controlling bacterial infection of mild diabetic ulcers (1A). We propose that ointments containing antibiotics should not be used (2A), as sufficient grounds for their use have not been established.
Recommendation level:
[1A] Cadexomer iodine, silver sulfadiazine, povidone iodine sugar.
[1C] Povidone iodine gel.
[1D] Iodoform, iodine ointment.
[2A] Ointments containing antibiotics (we propose not using them).
- There are two RCTs concerning the use of external antibacterial drugs for bacterial infection of diabetic ulcers.45, 46 These trials indicated the efficacy of saccharose45 and cadexomer iodine,46 and so the evidence level for cadexomer iodine is II and the recommendation level is 1A.
- Although there are no reports concerning silver sulfadiazine or povidone iodine sugar, their recommendation level for the treatment of pressure ulcers, a similar chronic skin wound, is comparable to that of cadexomer iodine.
- There are two RCTs on infection management with ointments containing antibiotics,47, 48 and so the evidence level is II. However, neither of them indicated an advantage to antibiotic ointments. Moreover, for deep, chronic pressure ulcers, their use often extends for a prolonged period, and so there may be a high likelihood of microbial substitution. Thus, the recommendation level is 2A.
- Povidone iodine gel, iodoform, iodine ointments, and similar agents are not recommended as there are few reports on these agents available, but their recommendation level for treating pressure ulcers is 1C or 1D, and their use for the treatment of diabetic ulcers cannot be ruled out.
- Cadexomer iodine produces its bactericidal effect by slowly releasing iodine.50 Dextrin polymer absorbs not only exudates but also bacteria,49-51 therefore, while it is useful for the treatment of wounds with a large amount of exudates or pus, old polymer beads must be completely washed off during dressing changes, and thus should not be used for pockets that are difficult to wash away old beads.52 If used for wounds deficient in exudates, it may cause drying of the wound surface, delaying wound healing. In a stage with well-developed granulation tissue, iodine may damage the tissue. In addition, caution is needed with respect to iodine allergies.52
- Silver sulfadiazine produces an infection-controlling effect on the wound surface due to the antibacterial action of the silver on cell membranes and cell walls.53, 54 It also suppresses the formation of biofilm by Staphylococcus aureus (S. aureus), including methicillin-resistant S. aureus (MRSA).55 Moreover, as an emulsion base is used, it exerts a cleaning effect on the wound surface by softening/lysing necrotic tissue. When exudate volumes are high, caution is needed as it may cause edema at the wound surface.52 In addition, its efficacy decreases when used concomitantly with povidone iodine, and its concomitant use with other drugs, particularly external enzyme preparations, should be avoided.52
- Povidone iodine sugar produces an infection-controlling effect due to the antibacterial effect of iodine.56 Sucrose inhibits the growth of bacteria and suppresses the formation of biofilms by S. aureus, including MRSA.57 Sucrose alleviates edema of the wound surface due to its water-absorbing properties and exerts an excellent granulation-promoting effect by stimulating collagen synthesis by fibroblasts.58 However, caution is required similarly to cadexomer iodine.
13.2.4 CQ5: Is systemic administration of an antibacterial drug useful for the control of local acute infection of diabetic ulcers?
Description of recommendation: Systemic administration of antibacterial drugs such as amoxicillin/clavulanate (1A), ampicillin/sulbactam (1A), imipenem (1A), ofloxacin (1A), clindamycin (1A), cefazolin (1A), cephatolexin (1A), cephalexin (1A), daptomycin (1A), vancomycin+ceftazidime (1A), piperacillin/tazobactam (1A), moxifloxacin (1A), or linezolid (1A) is recommended for infected moderate to severe diabetic foot ulcers.
Recommendation level: 1A.
- There are 19 RCTs concerning infected diabetic ulcers and systemic administration of antibacterial drugs,59-77 and so the evidence level is II and the recommendation level for each is 1A. While there are differences in effect, a certain level of efficacy has been demonstrated for these agents, so antibacterial drug administration is a necessity.
- Antibacterial agents shown to have efficacy are ampicillin/sulbactam, imipenem, cefazolin, cephatolexin, ceftriaxone + metronidazole (intravenous administration), daptomycin, vancomycin + ceftazidime, piperacillin/tazobactam (not covered by the Japanese National Health Insurance for infected skin and soft tissue), linezolid, piperacillin clindamycin, entrapenem, and tigecycline, and for oral use are amoxicillin/clavulanate, ofloxacin, clindamycin, cephalexin, moxifloxacin, and ticarcillin/clavulanate. Piperacillin clindamycin, entrapenem, tigecycline, and ticarcillin/clavulanate are not sold in Japan.
- The period of administration is recommended to be 1–2 weeks for mild infections and 2 weeks or longer for severe infections.78
- According to a bacteriological study of 454 cases of diabetic foot infection,79 48.9% contained only aerobic bacteria, 1.3% contained only anaerobic bacteria, and 43.8% yielded a mixed culture of anaerobic and aerobic bacteria. In addition, 16.2% of cases contained a single bacteria species, 20.4% contained two species, 19.7% contained three species, 13.3% contained four species, and 30.4% contained at least five species, and so it was common for there to be numerous species detected. Since mixed infections by gram-positive bacteria, gram-negative bacteria, and anaerobic bacteria are common, it is necessary to administer a broad spectrum of antibacterial agents.
13.2.5 CQ6: How long should systemic administration of antibacterial drugs be continued for the treatment of osteomyelitis?
Description of recommendation: For osteomyelitis associated with diabetic foot infection, we recommend administering antibacterial drugs for at least 2–4 weeks after removal of infected bone (1A). If the elimination of infected bone was insufficient, at least 6 weeks administration of antibacterial drugs is recommended (1D).
Recommendation level:
[1A] At least 2–4 weeks of antibacterial drug administration after removal of infected bone.
[1D] At least 6 weeks of antibacterial drug administration if elimination of infected bone was insufficient.
- There are three RCTs concerning diabetic foot infection (including osteomyelitis) and systemic administration of antibacterial drugs,62, 69, 70 thus the evidence level is II and the recommendation level is 1A. Ampicillin/sulbactam, imipenem, piperacillin/tazobactam, linezolid, tigecycline, and ertapenem have been shown to be effective, and the mean treatment period for osteomyelitis has been reported to be 19–21 days. In addition, antibacterial drugs are generally administrated for 2–4 weeks after removal of infected bones for osteomyelitis80-82 and this approximate period is considered the minimum for the administration of antibiotics.
- If infected bones cannot be sufficiently removed, the administration of antibacterial drugs for at least 6 weeks is considered necessary.83 The evidence level is VI, but as it is a commonly used treatment and it is considered necessary to prevent a progression to sepsis, the recommendation level is 1D.
- In diabetic ulcers, in which the immune function and regenerative ability of the skin are compromised, exacerbation of osteomyelitis may lead to a severe outcome, therefore it is necessary to administer antibacterial drugs at least over a period necessary for the treatment of osteomyelitis in general.
13.3 Severe ischemia/peripheral arterial disease
13.3.1 CQ7: How should limb ischemia be diagnosed during the initial outpatient examination?
Description of recommendation: When evaluating ischemic symptoms of extremities during outpatient diagnosis and treatment, we recommend measuring the ankle brachial pressure index (ABI) (1C), the toe brachial pressure index (TBI) (1C), the skin perfusion pressure (SPP) (1C), and the transcutaneous oxygen tension (TcPO2) (1C). In addition, we recommend palpation to confirm a weakened or absent peripheral arterial pulse, and a decrease in skin temperature (1A), as well as a detailed inquiry into the patient's smoking history and the presence of subjective symptoms such as numbness and coldness (1A).
Recommendation level:
[1A] Subjective and objective findings, medical interview regarding smoking history.
[1C] ABI, TBI, SPP, TcPO2 measurement.
- There is one systematic review reporting that subjective and objective symptoms are useful for the diagnosis of ischemia due to complications by PAD,84 and so the evidence level is I and the recommendation level is 1A. However, the subjects were not restricted to diabetic patients in this review. Nevertheless, diabetes is the underlying disease for PAD in a large fraction of cases,85, 86 and as there is a broad, international consensus that clinical symptoms are useful for the diagnosis of ischemia, it is recommended by many guidelines.17, 87
- There is one systematic review comparing the causes of PAD in high-income countries with mid-/low-income countries, showing that exacerbating factors common to each country are hypertension, hyperlipidemia, diabetes, and smoking,88 and so the evidence level is I and the presence of a history of smoking has a recommendation level of 1A. There are also analytic studies citing biological sex, hypertension,89 and length of time with diabetes90 as risk factors for PAD in diabetes.
- There is one small-scale meta-analysis on the utility of ABI measurement for PAD,91 and so the evidence level is I. However, its subjects were not limited to diabetes patients. Meanwhile, there is one case series study92 and three analytic immunological studies93-95 evaluating the utility of ABI measurements for PAD in the initial diagnosis and treatment of diabetes patients and diabetic skin ulcers, and so the evidence level is IVa and the recommendation level is 1C. The measurement technique in this testing method is relatively simple and can be easily implemented in the outpatient setting. Its utility has been established as a non-invasive testing method for PAD, and it is recommended in protocols and guidelines in both Japan and abroad.
- There are three analytic studies on the utility of TBI measurement in diabetic patients, including two that investigated a relationship with the PAD measurement values,96-98 and so the evidence level is IVa and the recommendation level is 1C. In addition, there is one systematic review investigating the utility of TBI measurement for PAD, although its subjects were not limited to diabetes patients.99 This paper noted that TBI measurements alone had a diagnostic sensitivity of 45 to 100% and a specificity of 16%–100%, and that there is a future need for TBI value standardization and accurate, large-scale research.
- There is one case-control study finding SPP indicating its utility for detecting severe PAD in diabetes/dialysis patients,100 and so the evidence level is IVb and the recommendation level is 1C.
- There is an analytic epidemiological study finding that in diabetes and dialysis patients with advanced arteriosclerosis, TcPO2 can be measured even when an evaluation using ABI is difficult, enabling evaluation of CLI,101 and so the evidence level is IVb and the recommendation level is 1C.
- Diabetic ulcers are often complicated by PAD, particularly peripheral arterial obstructive disease (PAOD), or in other words a condition that used to be called arteriosclerosis obliterans (ASO).87 As ischemia progresses, subjective symptoms such as numbness, pain, a cold sensation, and intermittent claudication appear in addition to signs including weakening or disappearance of peripheral arterial pulse, a decrease in the skin temperature, and changes in skin color, eventually leading to refractory ulcers or gangrene. In such cases, ulcers often occur at multiple sites at the ends of the toes and fingers or between the toes.102 It is possible to diagnose leg ischemia by detecting these symptoms through a medical interview, visual examination, and palpation. Conversely, the likelihood of PAD is lower with multiple normal clinical findings than with a single normal clinical finding.84 By the Fontaine Classification used for functional assessment of PAD (or PAOD), diabetic ulcers correspond to grade IV when accompanied by chronic arterial occlusive disease and consequently correspond to CLI.
- Patients may be asymptomatic in early stages of PAD due to compensation for ischemia. In diabetic patients, there may be no marked symptoms due to reduced motor abilities caused by complications such as neuropathy and cardiac disease.103 Moreover, the appearance of subjective symptoms of PAD may be delayed by hypoesthesia due to neuropathy. Therefore, for the diagnosis of PAD, we propose assessing blood flow using objective tests in addition to observing subjective and objective symptoms.
- The ABI, the ratio between the systolic blood pressures at the ankle and upper arm, and the TBI, the ratio between the systolic blood pressures at the toe and upper arm, are objective evaluations of peripheral arterial blood flow for the diagnosis of limb ischemia.
- The measurement technique for the ABI is relatively simple and can be performed easily in the outpatient setting. A large number of clinical studies have been conducted on the measurement of the ABI for the diagnosis and treatment of PAD, and its usefulness has been nearly completely established. In diabetic patients as well, the usefulness of the ABI has been evaluated by clinical studies, but many have aimed to clarify its relationship with the severity of coronary artery disease and vital prognosis. However, as diabetes is the underlying disease in many PAD patients, the ABI has been recommended as a standard non-invasive test for diabetic ulcers by foreign guidelines based on its established utility for diagnosing PAD in diabetic patients.17, 87, 104, 105 In Japan, there was a large cross-sectional study in which the ABI was measured in 3906 outpatients with diabetes,93 reporting that the ABI was reduced in 7.6% of the patients but that only 24.4% of that number had been diagnosed with PAD before its measurement, thus suggesting the usefulness of the ABI for screening (see the terminology list for details about normal values). However, the ABI is prone to being affected by vascular calcification, and so even if PAD is present, there are often cases when a high or a normal-appearing value is yielded. There is an analytic epidemiological study of 2080 type 2 diabetes outpatients in China indicating that when studying the incidence of PAD at high ABI values (>1.3) and normal values (>0.9, ≥1.3), the former had a higher odds ratio (6.97).106
- The TBI is known as a leg circulation evaluation method that is resistant to being affected by calcification.107 Transatlantic inter-society consensus (TASC) II recommends a protocol of investigating the presence of PAD by measuring the TBI when the ABI exceeds 1.40.104 It is a non-invasive procedure, which not all medical institutions are able to perform.
- The SPP and TcPO2 are methods for evaluating the skin microcirculation. There is an analytic epidemiological study that showed the SPP is strongly correlated with the toe pressure (TP) regardless of the presence of diabetes and is measurable in some patients in whom TP measurement is impossible (those with toe amputation and toe ulcers).108 There is a report that studied the efficacy of measuring the ABI and SPP values in ischemic limbs.100 Although a significant difference was not found between patients at Fontaine stages II to IV, the SPP value was clearly lower in patients at Fontaine stage IV compared to stages II and III, and so it was useful for detecting severe PAD in diabetes/dialysis patients. There is also an analytic epidemiological study of 96 asymptomatic CLI patients in which the risk of subsequent intermittent claudication and tissue loss was greater when the SPP in the opposite leg was less than 40 mmHg during the initial examination, suggesting that SPP measurements are useful for determining the prognosis.109 This is a non-invasive test that can evaluate the sole of the foot and the toes as well as the periphery of ulcers, and its utility has achieved a broad consensus. There are high hopes for a future dissemination of the testing devices.
- TcPO2 is a non-invasive test that is useful for evaluating the severity of an ischemic limb. According to TASC II, a TcPO2 of below 30 mmHg is considered CLI. Conversely, there is also the view that it is appropriate to diagnose CLI when the ankle joint pressure is less than 60 mmHg, the supine TcPO2 is less than 10 mmHg, and the TcPO2 in a hanging position is less than 45 mmHg.110 Starting in April 2016, it became possible to calculate one TcPO2 test every 3 months as the Japanese National Health Insurance includes coverage for patients with suspected CLI in order to determine a treatment plan or treatment effects for vascular reconstruction or amputation of the ischemic limb.
13.3.2 CQ8: What imaging tests are useful for a detailed investigation when limb ischemia is suspected during the initial outpatient examination?
Description of recommendation: For imaging tests evaluating limb ischemia during the initial outpatient examination, we recommend minimally invasive tests such as ultrasonography (1A), computed tomography angiography (CTA) (1A), magnetic resonance angiography (MRA), and similar procedures. To improve the diagnosis rate, it is preferable to combine these as appropriate, but since there are relatively few facilities that can perform all the above tests, whether to perform them should be considered based on the patient's condition.
Recommendation level:
[1A] Ultrasonography, CTA, MRA.
- There are three systematic reviews investigating the diagnostic accuracy of imaging tests for PAD.111-113 The evidence level is I and the recommendation level is 1A. Contrast-enhanced MRA has the highest reliability among the imaging tests, and CTA and ultrasound testing exhibit relatively high diagnostic sensitivity and specificity. In addition, the accuracy of DSA has been compared to contrast-enhanced MRA112 and to CTA,113 and so the accuracy of the latter two has been noted. However, the subjects in either case were not limited to PAD in diabetes patients. Meanwhile, there are three analytic epidemiological studies regarding PAD with an underlying condition of diabetes stating that contrast-enhanced MRA was superior in visualizing peripheral vasculature compared to DSA.114-116 Furthermore, there is one systematic review comparing the two tests,117 but it states that contrast-enhanced MRA cannot be considered the first choice for diagnosis, and that DSA should be equally taken into consideration depending on the patient.
- The detection rate for at least 50% stenosis and occlusion in the legs has been investigated for contrast enhanced MRA, CTA, and ultrasound testing. Their respective diagnostic sensitivities were 95%, 97%, and 91%, and their respective specificities were 91%, 88%, and 96%. MRA had the greatest frequency of adverse effects, but they were mostly mild. On the other hand, despite their low frequency, the highest fraction of severe adverse effects was seen in angiography.111
- If subjective and objective findings or abnormal ABI/TBI values are found in tests on initial outpatient examination, diagnostic imaging is performed to ascertain the sites and degree of angiopathy to determine a treatment plan and whether or not vascular reconstruction surgery is indicated.118
- Ultrasound testing is highly useful as it is simple and minimally invasive, can be performed repeatedly, and can evaluate the state of blood flow. However, it has the drawbacks that it requires technical skill, it cannot obtain findings for an entire leg, and it is difficult to evaluate the vascular lumen when calcification is advanced. There is one analytic epidemiological study stating that ultrasound testing is useful for evaluating vascular condition in the peripheral vasculature of the foot when it cannot be sufficiently visualized using digital subtraction angiography (DSA) or contrast-enhanced MRA.119
- CTA can be performed rapidly and minimally invasively, and has superior spatial resolution to MRA.120 There is one case-control study indicating that the detection rate for PAD was increased by combining the use of ABI and CTA.121 Instead, there are cases when it is not possible to view the vascular lumen, such as when calcification is advanced or a stent has been placed. It also involves a larger dose of radiation and contrast agent compared to DSA, and CTA using an iodine-based contrast agent cannot be performed in patients with an iodine sensitivity. In addition, caution is required for patients with renal disorders as the contrast agent can cause deterioration of renal function.
- MRA is minimally invasive and is useful in evaluating the range from major vessels to peripheral vasculature. Conversely, MRA may overestimate the extent of stenosis and may be influenced by artificial replacements. Caution is also required for renal disorder patients as the gadolinium contrast agent can cause nephrogenic systemic fibrosis.122 With progress in imaging methodologies in recent years, nearly identical results were reportedly obtained using non-contrast-enhanced MRA with the quiescent-interval single-shot (QISS) method compared to contrast-enhanced MRA.123
- Angiography of lesions provides the best resolution and is suitable for morphological observations. Recent years have also seen the spread of digital subtraction angiography (DSA), which obtains a clearer image. DSA is excellent for evaluating the inside of stents and is useful in evaluating hemodynamics. However, what is obtained is an image solely of the vascular lumen, it is slightly more invasive to patients due to catheter insertion, and it cannot be used with patients with hypersensitivity. Currently, rather than just diagnosis, it is often implemented in cases when vascular reconstruction surgery is considered.
- In the workflow for diagnostic imaging for suspected limb ischemia, ultrasound testing is performed and then CTA or (contrast enhanced) MRA is selected, after which DSA is performed if vascular reconstruction surgery is being considered. However, there are only limited facilities that can perform these tests, and so there are cases when their implementation should be considered cautiously depending on the patient's condition. It is difficult to equally/uniformly select a testing method, and so we propose increasing diagnostic accuracy by combining the use of multiple testing modalities.
13.4 Neuropathy/foot deformation
13.4.1 CQ9: What examinations are useful for the diagnosis of diabetic peripheral neuropathy?
Description of recommendation: A sensory examination using the Semmes–Weinstein monofilament test (1A), testing the sensation of vibrations using the tuning fork method (1C), and the Achilles tendon reflex test (1C) are useful for the clinical diagnosis of peripheral neuropathy due to diabetes, and are all recommended. To improve the diagnosis rate, these are preferably combined, as appropriate.
Recommendation level:
[1A] Monofilament method.
[1C] Tuning fork method, Achilles tendon reflex.
- There is one meta-analysis concerning the monofilament test124 and so the evidence level is I. The test is recognized to be useful and so the recommendation level is 1A. However, it cannot be performed at all facilities, as they are often not equipped with the testing equipment. There are two case reports on testing vibration sensation using a tuning fork, and so the evidence level is IVb and the recommendation level is 1C. The results of these reports were comparable with those of the monofilament test,125 and the diagnostic accuracy was comparable when the monofilament test was performed alone or in combination with other tests.126 Concerning the Achilles tendon reflex test, there is one cohort study127 and one case–control study,128 and so the evidence level is IVa and the recommendation level is 1C. This test can be performed easily and is widely adopted.
- In diabetic peripheral neuropathy, depression of tactile sensation is noted from an early stage, but approximately half of neuropathy patients do not notice the disorder129 and the diagnosis often cannot be made using clinical symptoms alone.130 To avoid overlooking signs of neuropathy, it is necessary to perform a combination of multiple tests to detect neuropathy and to use their findings to make comprehensive judgments rather than relying on a single examination. Combining multiple tests results in a diagnostic sensitivity for neuropathy of at least 87%.131
- The monofilament test is a simple test of tactile sensation using a 5.07 monofilament, with which a pressure of 10 g can be applied. If the patient is insensible to this stimulation, the likelihood of severe neuropathy is high. Aside from those described earlier, this test has been the subject of four cohort studies127, 132-134 and one each of a case–control study,135 cross-sectional study,130 and meta-analysis,124 all of which reported its usefulness.
- There is a case-control study on a disposable pocket-sized device for testing vibration sensation,136 which was reported to be equivalent to the monofilament test and significantly superior to the tuning fork method in detecting diabetic peripheral neuropathy. However, it is not sold in Japan.
- There is a systematic review on corneal confocal microscopy as a non-invasive method useful for the early diagnosis of diabetic peripheral neuropathy,137 but it can only be performed at an extremely limited number of facilities in Japan.
- There is a meta-analysis regarding an adhesive sticker applied to the sole of the foot that changes color as a result of perspiration, indicating it is useful for screening for diabetic peripheral neuropathy,138 with a reported sensitivity of 86% and specificity of 65%. However, it is not sold in Japan.
- Electrophysiological tests have greater variance in results depending on the level of skill achieved with the examination technique compared to the monofilament test, tuning fork method, and Achilles tendon reflex, take a longer amount of time, and can only be performed at a limited number of facilities and so are not widely adopted. In cases of diabetic peripheral neuropathy where a diagnosis was not possible or in cases that exhibit atypical clinical symptoms, electrophysiological tests and consultation with a neurologist can be considered.131 In Japan, medical devices are sold that relatively easily measure the sural nerve conduction velocity and action potential amplitude for early detection and monitoring the progress of diabetic peripheral neuropathy.139
- Neuropathy observed in most diabetic patients is primarily symmetrical polyneuropathy that progresses chronically due to hyperglycemia and is called distal symmetric polyneuropathy (DPN).140 For the management of patients with diabetic ulcer, it is necessary to diagnose the presence and severity of neuropathy. However, there is no symptom or examination specific to diabetic neuropathy, and while some diagnostic criteria have been proposed, none has gained an international consensus. Diagnostic criteria for DPN have been proposed in Japan by the Diabetic Neuropathy Study Group,141 and are based on vibration sensation testing using a C128 tuning fork and the bilateral Achilles tendon reflex in addition to subjective symptoms. In addition, a clinical staging classification142 has been proposed that, in addition to these diagnostic criteria, takes into consideration reduced surface sensation, orthostatic hypotension, dyshidrosis, and stubborn constipation/diarrhea, as well as reduced strength or atrophy of the legs.
13.5 Ulcer treatment
13.5.1 CQ10: How long should the observation period be for evaluating the usefulness of conservative treatment in diabetic ulcer patients?
Description of recommendation: We recommend evaluating the usefulness of conservative treatment for diabetic ulcers in the chronic phase within a maximum of 4 weeks and to compare it with other treatments when appropriate. However, it is desirable to examine diabetic ulcers in the acute period at least once a week.
Recommendation level: 1C.
- Even when administering conservative treatment while observing the course of a diabetic ulcer that has transitioned to the chronic period from the acute period, it is necessary to evaluate the effects of the treatment at appropriate times and its superiority or inferiority compared with other treatments. However, changing treatments one after the other in a short period may lead to errors in judgment, and the usefulness of each treatment must be evaluated based on observation over a sufficient period. There are two analytic epidemiological studies evaluating the treatment assessment intervals in this period,143, 144 and so their evidence levels are IVa and IVb, respectively, and their recommendation level is 1C.
- According to these studies, another treatment should be considered unless the ulcer area is observed to decrease to 40% or less of its initial size after at least 4 weeks. This interval is considered appropriate in the actual clinical setting from the realities of treatment plans and frequency of hospital visits in patients in the chronic period. Except for special cases, it is expected that the period of observing the progress of diabetic ulcers would not be longer than this in the actual clinical setting. However, as symptoms may change from moment to moment in the acute period of a diabetic ulcer when there is progressive exacerbation and when there is localized infection, treatment by frequent hospital visits or hospitalization is necessary.145 Because evaluating the utility of treatment is necessary on each of these occasions, examination at least once a week is desirable in such situations.
- Because frequent examination naturally leads to early detection of exacerbation of the lesion, foot care is important, including periodic checking of foot deformities, skin ulcers, nail plate deformities, sensibility, ischemia, and footwear.
- In treating diabetic ulcers, it is important to chronologically evaluate and record the patient's clinical history, history of ulcers, sites of their occurrence, condition of the wound surface (size, color, infection, exudates, and necrotic materials), and treatments. In diabetic patients, it is important to regularly examine their skin even if there is no ulcer for early detection, should one occur.
- When treating diabetic ulcers, these may be favorably controlled by scoring the condition of the wound surface and making observations over time.146-149
13.5.2 CQ11: Is surgical debridement useful for removing necrotic tissue from a diabetic ulcer?
Description of recommendation: If the patient's overall condition permits it, we recommend performing surgical debridement as the initial debridement to remove necrotic tissue and crust adhering to the ulcer, and keratinized material in and around the ulcer to control infection. However, if there is underlying PAD, there are cases when symptomatic improvement cannot be anticipated from surgical debridement, but rather increased severity of ulcers/gangrene can be expected. Therefore, surgical debridement should be performed carefully at the peripheral areas of the limbs, including limb amputations particularly when exhibiting osteomyelitis.
Recommendation level: 1A.
- There are two systematic reviews studying surgical debridement for removing necrotic tissue,150, 151 and so the evidence level is I and the recommendation level is 1A. However, although a statistically significant difference has not been found compared to other debridement methods, surgical debridement is prompt, convenient, and most desirable as the initial debridement to be performed in the initial stages with tightly adhering necrotic tissue. In addition, the international consensus is that, for wound bed preparation, surgical debridement should be performed in combination with other debriding methods as appropriate for maintenance debridement in routine clinical practice.17, 38, 152, 153
- If there are clear signs of infection, and if infection is causing necrotizing soft tissue infection such as necrotizing fasciitis or sepsis, emergency surgical debridement is essential to save the patient, and amputation may be inevitable in some cases.
- The objective of debridement is to prevent inhibition of wound recovery by removing necrotic tissue that provides a medium for bacterial infection and inhibits granulation tissue proliferation or epidermal regeneration, tissues that have already developed bacterial infection, and hyperkeratotic tissue interfering with epidermal regeneration. It is also necessary to determine the wound depth accurately.147, 154, 155 Debridement can be divided according to its objective into initial debridement performed early to remove adhering necrotic tissue, and maintenance debridement performed during daily medical care for wound bed preparation to maintain the wound bed in a favorable condition for recovery.147 Depending on the method used, it is classified into surgical or sharp debridement using a scalpel or surgical scissors, respectively, to perform an invasive procedure,156 and mechanical, autolytic, enzymatic, and biological (chemical [antiseptic]) debridement that does not involve invasive techniques.38
- Maintenance debridement performed after necrotic tissue or keratotic tissue has been reduced by initial debridement is often carried out by a combination of surgical and non-invasive methods.
- Among non-invasive methods, there is one RCT157 and two cohort studies158, 159 concerning autolytic debridement using hydrogel, which has been suggested to be significantly more effective than conventional procedures including wet-to-dry dressing, which is a method for mechanical debridement using gauze and physiological saline.
- As for biological debridement, a maggot therapy has been described using aseptically cultured maggots.160, 161 This method has the advantage of being relatively low in invasiveness to the patient.
- Regarding enzymatic debridement using enzyme preparations or polysaccharide beads, there is one RCT evaluating the debriding effect of bromelain on chronic ulcers,162 but its effectiveness against diabetic ulcers has not been established.
- If there is ischemia due to circulatory impairment of peripheral arteries such as PAD, invasive operations could enlarge the area of necrosis or gangrene, and so surgical debridement of the limb peripheries was conventionally contraindicated in ischemic patients. Therefore, surgical debridement should be performed carefully in patients with PAD, and the state of blood flow to the peripheral skin must be assessed before its implementation (see CQ7 for the assessment methods).
- If a large amount or area of tissue is removed by surgical debridement, the procedure is highly invasive to the patient and postoperative exacerbation of the patient's general condition is possible.161 Preoperative evaluation is necessary for the patient's general condition including the presence of anemia, hypoproteinemia, and bleeding diathesis, and for medication history including antiplatelet drugs and anticoagulants, which may affect clotting ability. Guidelines concerning cardiovascular disorders recommend continuation of these medications for minor operations in which bleeding is highly controllable.163 Guidelines concerning cerebral infarction also state that “continuation of oral” warfarin therapy is “desirable” and that antiplatelet therapy “may be continued”.164, 165 However, as these medications can be suspended in some patients, it is desirable to first consult the attending physician and manage the patients individually. In addition, if anticoagulants cannot be suspended, a debridement procedure may also be restricted within the area of necrotic tissue causing no bleeding (which results in little stress including pain to the body during the procedure), although this method is insufficient as surgical debridement.
- There is one retrospective cohort study on prognosis following conservative treatment and toe amputation for osteomyelitis complicating diabetic foot lesion. This study reported that there was no significant difference in hospitalization or treatment period for the group that received only conservative treatment and the group that underwent toe amputation.166
- It has been reported that for diabetic skin ulcers with exposed bone, exposing the marrow using a bone curette and covering with an occlusive dressing promoted wound healing.167
13.5.3 CQ12: What topical agents should be used for diabetic ulcers with no signs of infection?
Description of recommendation: As topical agents for diabetic ulcers, we recommend using trafermin (1A), prostaglandin E1 (1A), or tretinoin tocopherol (1A) for wounds with appropriate or deficient exudates. The use of bucladesine sodium (1A) is recommended for wounds with excessive exudates or marked edema.
Recommendation level:
Wounds with appropriate to deficient exudates: [1A] Trafermin, prostaglandin E1, tretinoin tocopherol.
Wounds with excessive exudates or marked edema: [1A] Bucladesine sodium.
- There are two RCTs on trafermin (basic fibroblast growth factor: bFGF),168, 169 and so the evidence level is II. However, there are only case reports concerning PGE1, bucladesine sodium, and tretinoin tocopherol,170-173 and so the evidence level is V. Nevertheless, as the recommendation levels of these three preparations are comparable with that of trafermin in guidelines concerning pressure ulcers, which are similar chronic wounds of the skin, their recommendation levels were also determined to be 1A identical to that of trafermin. There are even fewer reports regarding lysozyme chloride, aluminum chlorohydroxy allantoinate (alcloxa), povidone iodine sugar, and similar agents, and so these are not recommended. Still, their use for diabetic ulcers is not ruled out.
- Trafermin promotes wound healing due to its angiogenesis and granulation-promoting effects.174 Despite a strong wound healing effect, it is difficult to maintain a moist environment at the wound with trafermin alone as only a spray type preparation is available, so its use with other topical agents or dressing materials is recommended.175 Moreover, as it is marketed as a spray type preparation and as its effectiveness depends largely on its concentration, it is necessary to ensure patients sufficiently understand its method of use when it is administered to those with diabetic ulcers for outpatient treatment. Moreover, the concomitant use of an ointment with an oleaginous base such as petrolatum is necessary to maintain a moist wound environment. As hypertrophic scars have rarely been reported in recent years to be caused by trafermin, it is also expected to improve the quality of life (QOL) of patients with diabetic ulcers.176
- Prostaglandin E1 promotes wound healing by its effects on increasing cutaneous blood flow-increasing177 and promotion of angiogenesis.178 It also acts on fibroblasts, promoting their proliferation, and stimulates proliferation of keratinocytes by increasing the interleukin-6 released from fibroblasts. Because oleaginous plastibase is used as the base, PGE1 is appropriate for wounds with appropriate or deficient exudates but not for wounds with rich exudates or marked edema.
- Tretinoin tocopherol exerts granulation- and angiogenesis- promoting effects by promoting migration and proliferation of cells including fibroblasts. Because an emulsion base with a water content of 70% is used, the preparation is appropriate for wounds with a strong tendency to dry, but not for wounds with rich exudates or marked edema. It should be used after adequately evaluating the wound surface condition.
- Bucladesine sodium promotes wound healing by improving localized blood flow and promoting angiogenesis, granulation, and epidermal formation.179 Because macrogol used as the base is hygroscopic, the drug should be used for wounds with excessive exudates or marked edema. However, caution is necessary as it may cause drying of wounds with deficient exudates.
- There are few RCTs or non-randomized comparison studies on topical treatment specifically for diabetic ulcers, and so following the treatments for chronic wounds is valid.180
- In recent years, the effects of various growth factors and gene therapy on wound healing have been attracting attention, and there is a report with a high evidence level concerning the use of platelet-derived growth factor (PDGF) and epidermal growth factor (EGF) for the treatment of diabetic ulcers.181 While PDGF is already in clinical use in the USA, neither of these agents has yet been approved in Japan.182
13.5.4 CQ13: What dressing materials should be used for diabetic ulcers with no signs of infection?
Description of recommendation: For wounds with appropriate/deficient exudates, we recommend using hydrocolloids (1A), hydrogels (1B), or polyurethane foam (1B). For wounds with excessive effusion or marked edema, we recommend the use of calcium sodium alginate dressings (1C). In addition, we propose the use of Hydrofiber® (2C) for wounds with excessive effusion or marked edema.
Recommendation level:
Wounds with appropriate to deficient exudates:
[1A] Hydrocolloids.
[1B] Hydrogels, polyurethane foam.
Wounds with excessive exudates or marked edema:
[1C] Alginate dressings.
[2C] Hydrofiber®.
- There is one RCT on the use of hydrocolloids for the local treatment of diabetic ulcers183 and so the evidence level is II. However, a low number of cases were included in the study, and an additional study did not find hydrocolloids to have a higher utility than other dressing materials.184
- There are three RCTs regarding hydrogels157, 185, 186 and so the evidence level is II. However, the conclusions as to the efficacy of hydrogels are discordant among these reports. There is also a report indicating that the utility of hydrogels was not especially higher than that of other dressing materials.187 There are two RCTs regarding polyurethane foam188, 189 and so the evidence level is II. However, the conclusions as to its efficacy are discordant among these reports. There is also a report that the utility of polyurethane foam was not higher than that of other dressing materials.190 There is one RCT concluding that alginate dressing was inferior to silver-containing Hydrofiber® in improving ulcer depth,191 and one analytic epidemiological study concluding that there was no difference in healing time compared to conventional gauze dressing,192 and so the evidence level is II. However, since there are few reports using these dressings for the local treatment of diabetic ulcers, the recommendation levels from the guidelines for pressure ulcers, which are similar chronic skin wounds, were followed here, resulting in a level of 1A for hydrocolloids, 1B for hydrogels and polyurethane foam, and 1C for alginate dressings. In addition, there is one RCT on the use of Hydrofiber® for the local treatment of diabetic ulcers, and so the evidence level is II and the recommendation level is 2C, but the number of cases was low. Chitin, hydropolymer, and similar agents cannot be recommended due to the paucity of reports, but their use for diabetic ulcers is not ruled out.
- For diabetic ulcers, the dressing materials used and the time of their use must be selected in consideration of the condition of the wound and the skin around it, the patient's general condition and characteristics of the dressing materials193, 194 assuming sufficient caution against local infection. Dressing materials can be expected to maintain a moist wound environment, provide relief, and have a local protective effect. Furthermore, they also have high utility in easing the burden at the site of medical care.
- In chronic wounds, exudates obtained from occluded wound surfaces have been reported to inhibit cell proliferation.195 Wound bed preparation is a treatment resulting just from the appropriate control of exudates, and it should be applied to diabetic ulcers with sufficient knowledge about its theory and practice.
- Hydrocolloids maintain a moist environment without adhering to the wound. They prevent crust formation by reducing drying of the wound, promote migration of epidermal cells by maintaining a moist environment at the wound, and thus promote healing.196 They also prevent exposure of denuded nerve endings to air, thereby mitigating the characteristic tingling pain of shallow wounds.197
- Hydrogels not only promote granulation and epithelialization by maintaining a moist environment but they also alleviate inflammation and relieve pain due to their rapid cooling effect.198 Also, being transparent, they allows observation of the wound.199
- Polyurethane foam can absorb approximately 10 times its weight in exudates and promotes granulation and epithelialization by maintaining an appropriate moist environment. It leaves no residue resulting from dissolving or detaching, and it is unlikely to detach newly formed epithelium even if shifts from the wound surface.197
- Alginate fiber can absorb 10–20 times its weight of water.198 It promotes wound healing by gelling when absorbing a large volume of exudates and maintaining a moist environment around the wound.199 Moreover, calcium ions in alginate and sodium ions in blood/body fluids are exchanged across the interface between alginate fiber and the wound, and calcium ions diffuse into the capillaries due to the concentration gradient. This produces a hemostatic effect.200 However, there are no reports indicating that it has a clearly higher efficacy compared to other dressing materials.201
- Hydrofiber® can absorb approximately 30 times its weight of water.198 It retains approximately two times more water than alginate dressings and promotes granulation by maintaining a moist environment optimal for healing over a prolonged period.198 It prevents maceration of the healthy skin around the wound by blocking the horizontal spread of the exudates it has absorbed.198
- Silver-containing dressing materials and similar agents have been recently commercialized in Japan, and may be used for diabetic ulcers with local infection. However, they do not yet have an established evaluation.202, 203
13.5.5 CQ14: Is negative pressure wound therapyuseful for the treatment of diabetic ulcers?
Description of recommendation: We recommend performing negative pressure wound therapy (NPWT) for diabetic ulcers. If these are infected, cautious observation is required.
Recommendation level: 1A.
- NPWT is recognized as a treatment that is particularly highly effective for pressure ulcers.204 There are three RCT on the utility of using negative-pressure wound therapy for the local treatment of diabetic ulcers,205-207 and so the evidence level is II and the recommendation level is 1A.
- NPWT produces its effects by draining exudates, reducing bacteria, and drawing in the wound by the negative pressure.195, 208-213
- With regard to the strength of the negative pressure to be applied, there are no reports on pressures with a particularly high utility for diabetic ulcers, and so an effect can be expected both at low pressures and at high pressures.207 In addition, there are no differences between commercial products.214
- In Japan also a number of devices can be used for NPWT, but some patients are still expected to be treated using custom-made instruments. In either case, the principle of applying a negative pressure to the wound is the same, and the same therapeutic effect is expected even if a custom-made instrument is used for NPWT. However, as there is the problem of possible infections, custom-made instruments should be used appropriately by an experienced physician.
- Because there is a report that exudates collected from the wound surface under NPWT inhibited cell proliferation, caution is needed in occluding a chronic wound for prolonged periods.208
- NPWT is now possible also on an outpatient basis. The instruments usable for outpatient treatment are compact and are expected to improve the QOL of outpatients.
13.5.6 CQ15: Are weight-bearing orthoses useful for the treatment and prevention of diabetic ulcers?
Description of recommendation: We recommend using weight-bearing orthoses to resolve ulcers occurring due to compression by dispersing pressure. Because they are also considered effective for preventing compression, their use is recommended.
Recommendation level:
[1A] Treatment.
[1A] Prevention.
- There is one systematic review concerning treatments using weight-bearing orthoses,215 and so the evidence level is I and the recommendation level is 1A. However, as the treatment was performed using custom-made orthoses prepared by specialists, such a treatment is not available at all medical facilities. Regarding prevention, there is one systematic review concluding that these are effective,216 and so the evidence level is I and the recommendation level is 1A. There are additional two RCTs. The first RCT compared custom-made shoes and ready-made shoes on calluses occurring at the soles of the feet in patients with a history of foot ulcers. This RCT performed a follow-up survey of the recurrence rate, reporting a significantly lower recurrence in the custom-made group.217 The other RCT had patients with mild foot deformities wear normal shoes and shoes for treatment, and did not find a significant difference in the occurrence of ulcers after 2 years of follow-up.218
- In patients who have developed foot deformities or sensory disorders due to diabetic neuropathy, ulcers are often caused at the sole or toes due to abnormal pressure distribution on the skin. Therefore, relieving weight, or in other words preventing pressure from being applied to ulcers, is the basis for treating neuropathic diabetic ulcers. Silicone weight-relieving orthoses are sold for preventing pressure concentrations due to foot deformities and can be easily purchased by patients. Insoles are a simple weight-relieving orthosis, but orthoses that firmly secure the leg and cause the thigh and lower leg to support the body weight as much as possible are even more effective.
- The total contact cast (TCC; a type of so-called “non-removable cast”) is the most standard and effective among weight-bearing orthoses. Indeed, the cure rate was significantly higher in a group treated with TCCs than in a group treated with a conventional dressing material.219 In addition, a comparison of a fiberglass cast and canvas shoes reportedly resulted in faster healing of ulcers caused by diabetic neuropathy when the cast was used.220 However, as TCCs are not removable and require re-wrapping, and their production has technical difficulties as well, more easily applicable methods are considered desirable. Therefore, a removable cast walker, which is a removable ready-made orthosis for the leg, was compared to a non-removable cast, prepared by covering the removable cast walker with a rapidly drying plastic cast material to immobilize it similarly to a TCC. The cure rate after 12 weeks was reported to be significantly higher by the latter treatment in one report,221 while there are also reports that even after improving removable casts and non-removable casts there was no difference in the cure rate compared to TCCs, resulting in the former being recommended due to their simplicity.222, 223 There is also a report indicating an equivalent therapeutic effect between removable cast walkers and TCCs as a type of non-removable cast,224 and a report that removable cast walkers were superior in their weight-bearing properties at the forefoot compared to TCCs.225 Instead, there is a report that the cure rate of ulcers did not differ when TCCs were compared with custom-made temporary footwear,226 and a report that TCCs resulted in faster healing compared to removable cast walkers and half-shoe type orthoses.227
13.5.7 CQ16: What drugs are useful for the treatment of diabetic ulcers due to vascular disorders?
Description of recommendation: Among antithrombotic drugs, we recommend administering dalteparin (1A), argatroban (1C), sarpogrelate hydrochloride (1D), or cilostazol (1D). Among vasodilators, we recommend administering PGE1CQ26 (1C), Lipo-PGE1 (1C), or beraprost sodium (1D).
Recommendation level:
[1A] Dalteparin.
[1C] Argatroban, Lipo-PGE1, PGE1.
[1D] Sarpogrelate hydrochloride, cilostazol, beraprost sodium.
- There is a RCT indicating the efficacy of dalteparin, an antithrombotic agent for treating angiopathic ulcers.228 The evidence level is II and the recommendation level is 1A. There is a case series study indicating the efficacy of argatroban,229 and so the evidence level is V and the recommendation level is 1C. For sarpogrelate hydrochloride, there is only a report indicating its efficacy for PAD in general230 and an expert opinion, and so the evidence level is VI and the recommendation level is 1D. Regarding cilostazol, there is no evaluation of its effectiveness for the treatment of diabetic ulcers, but it is highly effective for the treatment of PAD,231 and there is a report that it suppressed the formation of diabetic ulcers as a result of preventive administration,232 and so it was rated similarly with a recommendation level of 1D.
- Among vasodilators, there is a case series study on the efficacy of Lipo-PGE1233 and a case report on PGE1,234 so the evidence level is V and the recommendation level is 1C. There are only expert opinions on the use of beraprost sodium for diabetic ulcers, so the evidence level is VI and the recommendation level is 1D.
- Diabetic ulcers can be broadly divided into those due to neuropathy and those due to circulatory disorders such as PAD, but there are cases where it is difficult to make a clear distinction between the two and cases in which both are causes. In this section, antithrombotic agents and vasodilators are discussed in this order.
- There is one RCT only regarding dalteparin, a low-molecular weight heparin (LMWH), as an antithrombotic agent, for use in diabetic patients with foot ulcers and PAD.228 Although the cure rate and limb salvage rate were significantly higher with dalteparin compared with placebo, the time until cure was not shortened. In addition, while its effects on ulcers are not discussed, a similar RCT was carried out by the same institution,235 and promotion of skin oxygenation and suppression of the thrombogenic activity were reported in the dalteparin group. However, it is indicated in Japan only to prevent clotting during hemodialysis and for use when there is disseminated intravascular coagulation (DIC).
- Argatroban was evaluated in 43 patients with skin ulcers, including those with collagen disease, pressure ulcers, and diabetes.229 The drug was administered to 14 patients with diabetic ulcers without distinction between circulatory and neuropathic ulcers, and at least a decrease in the ulcer size was noted in 69% of the patients. Moreover, the drug is frequently used clinically, although it is not covered by Japanese National Health Insurance when used for diabetic ulcers.
- Concerning sarpogrelate hydrochloride, there are many expert opinions supporting its effectiveness, although it is not possible to isolate the cases in which this agent was use for diabetic ulcers as described above, although it is used frequently. In Japan, a decrease in the ulcer size and improvements in pain and cold sensation were observed in a study in patients with severe chronic arterial obstruction exhibiting ischemic ulcers.230 It is covered by Japanese National Health Insurance for skin ulcers caused by PAD.
- Regarding cilostazol, there is one report evaluating the incidence of foot ulcers in diabetic patients with peripheral circulatory disorders, who were divided into 47 subjects to whom the drug was administered for an average of 16 months at a dose of 100 mg × 2 per day and 31 subjects who did not receive the drug.232 It was shown to significantly decrease the incidence, which in the two groups was 4.25% and 35.48%, respectively. In addition, cilostazol has been reported to reduce the size of leg ulcers in 177 PAD patients in a multicenter double-blind study in Japan, although not all the subjects had diabetic ulcers.230 Cilostazol is covered by Japanese National Health Insurance only for use in ulcers based on PAD. There are only a few studies on its use for diabetic ulcers, although there are many expert opinions indicating that it is effective.
- Aspirin and ticlopidine are frequently used drugs, but their effectiveness for the treatment of diabetic ulcers has not been sufficiently evaluated.
- Regarding clopidogrel, an additional indication for suppressing thrombus/embolism formation in PAD was added in September 2012, but there is no evidence with respect to diabetic ulcers.
- Concerning ethyl icosapentate, there is a report that at least a partial improvement was observed in 80% of the patients with ASO in a clinical study in Japan, but the subjects of this study were not restricted to those with diabetes as an underlying disease.
- There is a RCT of iloprost, a PG derivative. An improvement was observed in 62% of the patients administrated iloprost compared with 23.5% of those administrated a placebo, which was a significant difference.236 However, while this drug is approved in Western countries, it is not on the list of official drug prices available for Japan.
- Regarding Lipo-PGE1, there was a study in Japan in which patients with diabetic ulcers consisting of 71 individuals with vascular disorders, 70 with neuropathy, and 125 with a combination of both were treated for 4 weeks intravenously at 5–10 μg/day, resulting in improvement rates of 68.8%, 83.6%, and 65.3%, respectively.233 Lipo-PGE1 is believed to have a greater effect in ulcers due to neuropathy as they primarily arise due to microcirculation disturbances, compared to ulcers from vascular disorders in which issues are observed in thicker vessels. There is also a case study indicating the efficacy of PGE1.234 Lipo-PGE1 is covered by Japanese National Health Insurance for diabetic ulcers, but PGE1 is only approved for ulcers caused by PAD.
- Beraprost sodium, a PGI2 derivative, has been reported to improve the distance of intermittent claudication and ABI in PAD patients, and to improve peripheral hemodynamics in patients with PAD complicating diabetes. There is an analytic epidemiological study on its effect on patients with PAD-complicated diabetes237 and a case series study about its ulcer size reducing effect.238 It is used frequently since it is an oral medication, many expert opinions support its effectiveness, and it is covered by Japanese National Health Insurance for ulcers accompanying PAD.
13.5.8 CQ17: What drugs are useful for the treatment of diabetic ulcers due to neuropathy?
Description of recommendation: We recommend administering the vasodilator lipo-prostaglandin E1 (PGE1) (1A), PGE1 (1C), or beraprost sodium (1C). We recommend administering the antithrombotic drug dalteparin (1D).
Recommendation level:
[1A] Lipo-PGE1.
[1C] PGE1, beraprost sodium.
[1D] Dalteparin.
- For the treatment of neuropathic ulcers, there are two RCTs on the use of the vasodilator, Lipo-PGE1.239, 240 The evidence level is II and the recommendation level is 1A. There is a case series study on PGE1.241 The evidence level is V and the recommendation level is 1C. There is one RCT on beraprost sodium.242 The evidence level is II, but the subjects were not limited to ulcers caused by neuropathy and this drug is not covered by the Japanese National Health Insurance, and so the recommendation level is 1C. Among antithrombotics, there is a case report on dalteparin, which is a low-molecular weight heparin (LMWH),243 and so the evidence level is V, but it is not used much and is not covered by the Japanese National Health Insurance program, and so the recommendation level is 1D.
- Concerning vasodilators, many evaluations using Lipo-PGE1 have been performed, including a comparison study with PGE1 and a placebo. In a double-blind RCT in which patients with diabetic neuropathy or diabetic ulcers were selected, the subjects were divided into three groups that were respectively administered (1) Lipo-PGE1 at 10 μg/day, (2) a placebo, or (3) PGE1 at 40 μg/day for 4 weeks. The results showed there was a significant difference in ulcer reduction between the Lipo-PGE1 and the placebo groups after the first week, and between PGE1 and the placebo groups after the second and third weeks.239 There is also a multicenter RCT in which Lipo-PGE1 or PGE1 was administered for 4 weeks to inpatients with at least one symptom, including spontaneous pain, sensory abnormality, skin ulcers, or skin necrosis due to diabetic neuropathy.240 Ulcers and gangrene were observed in 27 and 24 patients, respectively, and it was reported that the final degree of improvement was significantly higher in the Lipo-PGE1 group than in the PGE1 group, and that the ulcer size reduction rate was also greater in the Lipo-PGE1 group. In an investigation comparing Lipo-PGE1 to a placebo, the skin ulcer improvement rate was significantly higher in the Lipo-PGE1 group at 69% compared with the placebo group at 32%.244 In addition, a report investigating the rate of improvement using Lipo-PGE1 for ulcers caused by neuropathy and those caused by vascular disturbance found a rate of 83.6% in neuropathic ulcers, which was a significantly greater effect than in those caused by vascular disturbance.233 There are also a large number of case reports, including one in which Lipo-PGE1 was effective in four patients with diabetic ulcers accompanied by neuropathy, supporting its efficacy.245 The drug is covered by the Japanese National Health Insurance program for diabetic ulcers and ulcers caused by systemic lupus erythematosus (SLE), systemic sclerosis (SSc), and PAD, such as chronic arteriosclerosis obliterans.
- Concerning PGE1, there is a case series study in which the drug was administered by intravenous infusion at 20–80 μg/day to 11 patients with ulcers associated with diabetic neuropathy, resulting in a rate of improvement by at least an effective amount of 73%.241 The only symptoms for which this drug is covered by the Japanese National Health Insurance program are ulcers caused by PAD.
- Concerning beraprost sodium, there is one RCT involving 50 patients with diabetic ulcers without PAD. By administering 60–120 μg/day for 6 weeks, the cure rate was significantly higher in the treated group, at 48% compared to 8% in the control group.242 However, similar to PGE1, beraprost sodium is not covered by the Japanese National Health Insurance program for diabetic ulcers.
- Regarding antithrombotic drugs, dalteparin (2500 units) was administered to 10 patients with diabetic ulcers complicated by peripheral neuropathy or peripheral arterial obstructive diseases for 8 weeks, and the ulcerated area was reduced in eight subjects, of which four were cured. However, lesions due to peripheral neuropathy and those due to peripheral arterial obstruction were not clearly distinguished and the number of patients was small.243 Dalteparin is covered by Japanese National Health Insurance only for DIC and to prevent blood coagulation during hemodialysis.
13.5.9 CQ18: What drugs are useful against diabetic neuropathy?
Description of recommendation: For painful diabetic neuropathy, we recommend administering amitriptyline hydrochloride (1A), or nortriptyline (1B), tricyclic antidepressants: duloxetine (1A), a serotonin noradrenaline reuptake inhibitor (SNRI); gabapentin (1A) or pregabalin (1A), Ca2+ channel alpha2delta ligands; or mexiletine (1A), an antiarrhythmic agent. For diabetic neuropathy in general, we propose the administration of epalrestat (2A) as an option.
Recommendation level:
Painful diabetic neuropathy:
[1A] Amitriptyline hydrochloride, duloxetine, gabapentin, pregabalin, mexiletine.
[1B] Nortriptyline.
Diabetic neuropathy:
[2A] Epalrestat.
- For painful diabetic neuropathy, there is a systematic review246 and an RCT247 indicating the efficacy of amitriptyline hydrochloride. The evidence levels are I and II, respectively, and the recommendation level is 1A. There is a non-randomized comparison study indicating that nortriptyline has equivalent effects as amitryptiline,248 and so the evidence level is III and the recommendation level is 1B. There is a RCT examining duloxetine,249 and so the evidence level is II and the recommendation level is 1A. There is one RCT regarding gabapentin250 and two RCTs examining pregabalin,251, 252 and so the evidence level for each is I and the recommendation level is 1A. There is a RCT253 and a meta-analysis254 on mexiletine hydrochloride, and so the evidence level is I and the recommendation level is 1A.
- For diabetic neuropathy, there are two systematic reviews on epalrestat255, 256 and so the evidence level is I, but no significant difference in treatment effect was seen when compared to placebos. In addition, there is a meta-analysis257 with an evidence level of I, but the effectiveness determination differed depending on the parameters evaluated, so the recommendation level was set at 2A.
- Diabetic neuropathy is the most common complication. The primary type is diabetic polyneuropathy and includes polyneuropathy of the sensory and autonomic nerves and painful diabetic neuropathy. Neuropathic pain is the primary cause of painful diabetic neuropathy. Pain arises due to nerve degeneration and is a symptom observed in a variety of other conditions, including postherpetic neuralgia. In addition, guidelines for the pharmacological treatment of neuropathic pain have been produced in Japan for painful diabetic neuropathy.
- Amitriptyline hydrochloride is an antidepressant and exerts its effects by activating the descending pain control system. A systematic review has indicated its utility for neuropathic pain in general,246 and a placebo-controlled double-blind RCT has found a significant difference in the pain relief that it causes for diabetic neuropathic pain.247 In addition, nortriptyline, which is another tricyclic antidepressant, was found to have an equivalent analgesic effect, and has few side effects such as anticholinergic effects, so it is recommended more for the elderly.248 However, neither amitriptyline hydrochloride nor nortriptyline is covered by Japanese National Health Insurance for neuropathic pain.
- Duloxetine, an SNRI, has a mechanism of action of activating the descending pain control system, just like tricyclic antidepressants. There is a report that administering 60 and 120 mg/day significantly reduced the pain score compared to a placebo, and that administering 60 mg/day divided into two doses produced the same effect as a single dose and also reduced side effects.249 An additional indication of this drug for pain caused by diabetic neuropathy was added in February 2012.
- Gabapentin and pregabalin bind to the alpha2delta subunit of voltage-gated calcium channels, suppressing the release of excitatory neurotransmitters. The two are analogs and have the same mechanism of action, but pregabalin has a stronger affinity to the alpha2delta subunit, and so a smaller dosage may be used. There is a double-blind RCT for gabapentin involving 165 subjects reporting that its improvement of QOL and pain was significantly superior to the placebo.250 Pregabalin has similarly been found to be effective in RCTs,251, 252 and was found to ease pain even in intractable cases in which other agents were not previously found to be effective.253 Pregabalin has been covered by the Japanese National Health Insurance for neuropathic pain, including that of the central nervous system, as of February 2013. However, gabapentin is only covered as an antiepileptic drug as part of combined therapy for partial seizures in epilepsy patients, for which a sufficient effect has not been observed.
- Mexiletine hydrochloride is an antiarrhythmic agent whose mechanism of action is blocking sodium channels. In a double-blind RCT performed in Japan, 300 mg/day was administered, which significantly reduced spontaneous pain and subjective symptoms such as numbness compared to a placebo.254 In addition, a meta-analysis has also indicated its utility.255 It is covered by the Japanese National Health Insurance program for the improvement of subjective symptoms accompanying diabetic neuropathy.
- Opioids such as oxycodone and tramadol have strong analgesic effects, but have issues associated with tolerability. Their administration is considered for intractable cases.
- It has been suggested that multiple factors such as metabolic disorders, decreased blood flow, abnormal nerve regeneration, and similar conditions are involved in the origin of sensory disturbances in polyneuropathy. Among these, polyol metabolism disorders are the most important causative factors; aldose reductase is activated in hyperglycemic states, promoting polyol metabolism pathways.
- There are two systematic reviews that provide a comprehensive evaluation of aldose reductase inhibitors (ARIs) indicating that they did not produce a significantly different therapeutic effect compared to placebos in polyneuropathy patients.256, 257 In addition, there is a meta-analysis stating that although ARIs improve motor nerve conduction velocity (NCV) compared to a control group, they do not produce a significant effect in other parameters and it is difficult to evaluate in a short-term study.258
- Epalrestat is approved in Japan and is the subject of the greatest number of reports. There is a RCT finding it is effective for autonomous nerve function recovery when administered early when neuropathy occurs, but it was ineffective for motor and sensory nerve damage.259 There is also a RCT finding that epalrestat delays the progression of neuropathy and reduces symptoms in patients with good blood sugar control and mild microangiopathy.260 In addition, there are reports that it significantly improved leg numbness, sensory disturbance, and cold sensation, as well as subjective symptoms and nerve function.261, 262 There are additional numerous molecular epidemiological studies and descriptive studies, including those performed abroad, and so it is considered to be effective.
- There are many other drugs suggested for diabetic neuropathy treatment, including numerous reports that the antioxidant alpha-lipoic acid and L-carnitine are effective. In addition, C-peptide, benfotiamine, a derivative of fat-soluble thiamine B1; trandolapril, an ACE inhibitor; Lipo-PGE1, and similar agents have been reported to be useful.
13.5.10 CQ19: Is glycemic control useful for improving the cure rate of diabetic ulcers?
Description of recommendation: Proper glycemic control is recommended as it reduces local factors inhibiting wound healing and leads to improvement in the mechanism of wound healing.
Recommendation level: 1C.
- There are three case reports263-265 and two expert opinions266, 267 concerning the effectiveness of blood sugar control (glycemic control) for improving the cure rate of diabetic ulcers. The evidence level is V and VI, and the recommendation level is 1C. Consequently, controlling symptoms of the primary disease is believed to contribute to a decrease in local factors inhibiting wound healing.
- Case reports and expert opinions constitute the majority of the published work evaluating the effects of glycemic control on ulcer healing in patients with diabetic ulcers, and so the evidence level is not high. However, the approach is recommended by foreign guidelines. Various inhibitory factors of wound healing are involved in the formation of diabetic ulcers, and glycemic control is believed to contribute to improvements in the mechanism of wound healing by reducing such factors.153, 268-271
13.5.11 CQ20: Does improving the nutritional status of diabetic patients promote the healing of diabetic ulcers?
Description of recommendation: Improving the nutritional status under the guidance of a specialist in nutrition is recommended.
Recommendation level: 1B.
- Regarding the relationship between nutritional condition and diabetic ulcers, there is one non-randomized comparison study finding that improved nutritional condition promoted ulcer healing,272 the evidence level is III, and the recommendation level is 1B.
- Generally, intervention by the NST is important in the treatment of ulcers, and nutritional guidance by an expert is considered extremely beneficial for disease management in diabetes patients in particular. However, there are not many reports concerning nutritional intervention and wound healing specifically for diabetic ulcer patients.
- Excessive nutritional supplementation with the objective of ulcer healing should not be carried out for diabetic ulcer patients. Since there are patients placed under caloric restriction to treat the primary disease as well as patients who require improvements to a poor nutritional condition, this treatment should not be uniformly implemented. Nutritional guidance by the NST led by a nutritionist should be attempted by monitoring daily changes in the patient's blood glucose levels.273-276
13.5.12 CQ21: Can hemodialysis cause diabetic ulcers or act as a factor delaying healing?
Description of recommendation: We recommend managing diabetic patients undergoing dialysis therapy with attention to the possibility that hemodialysis can affect the development of skin ulcers and delay their healing.
Recommendation level: 1C.
- There are five cohort studies277-281 and three case-control studies282-284 analyzing the effects of dialysis on diabetic ulcer formation and factors delaying healing, the evidence level is IVa, and the recommendation level is 1C.
- Dialysis is indispensable to sustain life in patients with marked diabetic nephropathy, and so dialysis cannot be withheld from such patients with renal failure. As a result, a RCT comparing outcomes with and without dialysis is impossible and so unsurprisingly clinical study results at a high evidence level cannot be obtained. However, it is a well-known fact that dialysis promotes the progress of vascular calcification and so it is certainly an exacerbating factor. In addition, partly due to the 2016 revision to the medical payment system in which there was a newly established monthly 100-point surcharge for guidance and management of leg PAD in chronic maintenance dialysis patients, it is extremely important to be cognizant that dialysis patients are at a high risk of diabetic ulcer formation and exacerbation.
- The number of dialysis patients in Japan has continued to increase, and the majority of incident dialysis patients have diabetic nephropathy. In Japan, hemodialysis accounts for 95% of dialysis cases, with peritoneal dialysis constituting only 5%, but the proportion abroad is reported to be 2/3 for hemodialysis and 1/3 for peritoneal dialysis. Thus, it should be noted that the references pertaining to this CQ include three types of reports: those dealing with hemodialysis alone, peritoneal dialysis alone, and both. During hemodialysis, the waste products of the entire body accumulated over 2 or 3 days must be eliminated in only 4 h, whereas peritoneal dialysis is performed gradually across four sessions per day lasting 30 min each time. Vascular calcification is frequently observed in dialysis patients, therefore dialysis as a medical action affects diabetic skin ulcers primarily by “indirectly promoting the progression of arteriosclerosis.”
- References include a report that dialysis is a risk factor for amputation of severely ischemic limbs and death (odds ratio: 8.93),277 a report that diabetes is a risk factor for dialysis patients who have had a major amputation (hazard ratio: 7.4),278 a report that dialysis is a risk factor for major amputation in diabetic ulcer patients (hazard ratio: 2.14),279 a report that in a 10-year follow-up survey, renal failure was a factor that negatively impacted outcomes,280 a report that the risk of ulcers and leg amputation was higher in a diabetes patient group with end-stage renal failure compared to groups with only the individual conditions,281 a report that the rate of ulcer formation and the rate of amputation were higher the more severe the diabetic nephropathy group,282 a report that dialysis in a diabetes patient was a risk factor for ischemic ulcers (odds ratio: 21.58),283 a report that cutaneous blood flow decreased during dialysis in diabetes patients,284 and similar studies. This analysis approached the issue from different angles, but suggested that dialysis of diabetes patients could lead to the occurrence and deterioration of ischemic ulcers.
- A majority of incident dialysis patients in Japan start because of worsening diabetic nephropathy. Calciphylaxis frequently seen in dialysis patients causes skin ulcers and worsens the prognosis, and so is the condition requiring the most attention. However, since there are few cases, no epidemiological studies of diabetic ulcers complicating this condition are seen.
13.6 Selection of other treatment methods and preventing recurrence
13.6.1 CQ22: Is hyperbaric oxygen therapy useful for the treatment of diabetic ulcers?
Description of recommendation: Hyperbaric oxygen therapy is recommended for the treatment of diabetic ulcers. However, not many facilities or institutions are equipped for this treatment.
Recommendation level: 1A.
- There are seven systematic reviews concerning hyperbaric oxygen therapy for the treatment of diabetic ulcers,285-291 the evidence level is I, and the recommendation level is 1A. Differences in evaluated variables can be seen among the systematic reviews, including that hyperbaric oxygen therapy is useful for avoiding major amputations,285, 286 that it is useful for treating wounds,285 that a short-term effect can be expected but that it does not have a long-term effect,286 that it is not useful for infected wounds,289 and that it is effective even in ischemic limbs.291 In addition, not only is hyperbaric oxygen therapy reported effective for reducing amputation rate,292, 294, 295 increasing transcutaneous oxygen pressure,294-296 and significantly shrinking ulcer size,293, 294 but it has also been reported to improve the QOL of patients, although this is not an evaluation specifically of the wound.298 Conversely, there was also a report that although an improvement was seen in the initial 2 weeks, no long-term effect was seen in wounds under oxidative stress.297
- By increasing the partial pressure of oxygen in blood and tissues, hyperbaric oxygen therapy not only relieves hypoxic conditions but also produces a wide range of effects such as alleviation of edema caused by the pressure and suppression of bacterial growth resulting from oxygen toxicity. However, this therapy can be performed only at the few medical facilities equipped with a hyperbaric oxygen therapy device and at least 1 h is needed for each round of application. This therapy is subject to low medical compensation, thus it is not widely used in Japan. Nevertheless, devices capable of localized hyperbaric oxygen therapy are being developed abroad and it is considered an effective treatment.
- This treatment is contraindicated in patients with untreated pneumothorax, and after ophthalmological treatment and surgery (when C3F8 or SF6 intraocular gases are used).
13.6.2 CQ23: Is low-density lipoprotein apheresis useful for the treatment of diabetic ulcers?
Description of recommendation: Low-density lipoprotein (LDL) apheresis is recommended because it can be expected to produce a therapeutic effect in diabetic ulcers complicated by major vascular disease.
Recommendation level: 1C.
- Concerning the effects of LDL apheresis on diabetic ulcers, there are two case series studies299, 300 and five case reports,301-305 the evidence level is V, and the recommendation level is 1C.
- LDL apheresis as a treatment for ASO of the leg is covered by the National Health Insurance program in Japan and has been reported to be effective. However, it is not mentioned as a treatment for diabetic or non-diabetic PAD in the TASC II, which is an international guideline for the diagnosis and treatment of ASO of the leg. Concerning its effectiveness in the actual clinical setting, there are only sporadic case series studies299 and case reports.301-305
- The underlying principle of this treatment is to adsorb and eliminate lipoproteins such as LDL and very low-density lipoprotein (VLDL), which are arteriosclerogenic factors, using dextran sulfate given its strong negative electrical charge as the adsorption ligand. However, the mechanisms of its effects on PAD are considered an improvement in blood viscosity due to elimination of lipids and clotting factors, improvements in oxygen and nutrient transport due to an increase in the erythrocyte deformability, and vasodilation caused by bradykinins generated during the treatment, rather than being caused by a decrease in LDL cholesterol. The clarification of the mechanisms of its effects have been advanced in recent years by a series of reports of increases in vasodilator materials such as nitric oxide (NO), vascular endothelial growth factor (VEGF), and insulin-like growth factor (IGF)-1, decreases in inflammatory materials such as oxidized LDL, intercellular adhesion molecule-1 (ICAM-1), high-sensitivity CRP and P-selectin, and decreases in factors that delay wound healing such as matrix metalloproteinsase-9 (MMP-9), tissue inhibitor of metalloproteinase-1 (TIMP-1), vascular cell adhesion molecule-1 (VCAM-1), and endothelin-1 (ET-1).
13.6.3 CQ24: Can the occurrence and exacerbation of diabetic ulcers be prevented by treating tinea pedis or toenail tinea unguium (toenail tinea)?
Description of recommendation: Treatment for tinea pedis or tinea unguium (toenail tinea) is recommended to prevent the occurrence and exacerbation of diabetic ulcers.
Recommendation level: 1A.
- Concerning whether treatment of tinea pedis is effective for the prevention of diabetic ulcers, there is one RCT,306 the evidence level is II, and the recommendation level is 1A. No significant difference was noted in the incidence of ulcers whether or not tinea pedis was treated, but there are reports that patients with tinea pedis are more likely to develop cellulitis307 and that infection is observed more frequently in patients with a high hemoglobin A1c level, indicating poor control of diabetes.308
- A report investigating the prevalence of tinea pedis and toenail tinea unguium in a group of diabetes patients and a control group with matched patient backgrounds found significantly higher rates of 46.7% and 53.3% in the diabetes patients compared to the controls.309 In addition, a report studying 230 diabetes patients examined by a podiatrist found toenail tinea unguim in 58.3% of cases, of which it was found in all toenails in 38.1% of patients.310
- There is no report with a high evidence level that tinea pedis exacerbates diabetic ulcers, but a study evaluating risk factors of the occurrence of ulcerative lesions in 1285 diabetic patients concluded that factors include concurrent visual impairment, history of foot ulcers, and history of foot amputation in addition to tinea unguium.311
- However, as to whether or not treatment of toenail tinea unguium contributes to the prevention of diabetic ulcers, a RCT showed that external application of nail polish containing an antifungal agent (ciclopirox 8%) did not significantly reduce the frequency of ulcer incidence in diabetes patients with tinea pedis.306
- However, taking into consideration the fact that cellulitis is more likely in tinea pedis patients308 and the fact that bacterial infection is a factor exacerbating diabetic ulcers, early treatment of tinea pedis is considered indispensable for preventing ulcer formation.
- In addition, toenail tinea unguium often causes toenail thickening, which can be a cause of damage to the surrounding skin and increases patient burden. It is desirable for diabetic patients with difficulty in clipping toenails due to reduced vision or muscle strength to visit the dermatology or foot care outpatient clinic at regular intervals.
13.6.4 CQ25: Is treatment for calluses or foot corns useful for preventing diabetic ulcers?
Description of recommendation: We recommend taking appropriate measures such as shaving to prevent calluses and foot corns in diabetic patients.
Recommendation level: 1A.
- There is one systematic review on the relationship between plantar calluses/foot corns and foot ulcer formation,312 the evidence level is I, and the recommendation level is 1A. However, ulcers can be exacerbated by inappropriate treatment, and this document states that the risk of ulcers is not reduced by treatment for foot corns.
- Concentration of the weight load at particular sites of the sole is known to be a major factor of the formation of diabetic ulcers, and calluses and foot corns contribute to it. A retrospective study of 243 diabetes patients found callus or foot corn formation in 38% of the subjects.313 In addition, a prospective evaluation of 63 diabetic patients reported that a history of ulcers and the presence of calluses increased the risk of ulcer formation.314
- Calluses in diabetic patients exhibited much stronger inflammatory symptoms compared to those in non-diabetic patients, suggesting that they are a risk factor for foot ulcers.315
- Concerning treatments, there is a report evaluating the weight load on the sole and the presence of treatment in 33 diabetic patients divided into a group with calluses, a group with no calluses, and a group in which calluses were removed. The plantar pressure was significantly increased in the group having calluses, and the pressure was reduced significantly by removing calluses, and so the treatment is recommended.316 However, there is also a systematic review that the risk of ulcer formation is not reduced by treatment of calluses.312 Nevertheless, it has been reported that when commonly recommended foot care was performed on a continuing basis in accordance with a preventive program for diabetic foot lesions, ulcers caused by calluses were successfully prevented.317
- In addition, one report recommends caution when treating foot corns because severe foot ulcers and sepsis occurred after treatment for foot corns.318 Because treatments for calluses or foot corns such as scraping are medical procedures, they should be performed carefully under the supervision of a physician.
13.6.5 CQ26: Is patient education (including whole-body and foot bathing) useful for the treatment of ulcers in diabetics?
Description of recommendation: Patient education (self-learning) through diabetes classes is useful as part of the treatment and is recommended.
Recommendation level: 1A.
- There is one systematic review concerning the usefulness of patient education regarding matters such as physical therapy,319 which is rated as evidence level I and recommendation level 1A. There are a number of reports that patient education suppresses ulcer formation in diabetic ulcer patients,320-325 and patient education has been reported to reduce the risk of leg amputation in diabetic ulcer patients.326 Conversely, there is a RCT that found that education of patients with diabetic ulcers did not affect ulcer treatment,327 and there is also the opinion that the evidence is insufficient to conclude that patient education significantly decreases ulcer formation and leg amputation frequency.328 Thus, no consensus has been reached concerning education of patients with diabetic ulcers.
- In Japan, various grassroots opportunities have been taken to promote understanding in diabetic patients of the disease, and there have been certain accomplishments. For the management of diabetes, patient education is performed actively at each medical organization under names including “diabetes class.” Controlling diet and performing appropriate exercise in daily life are important for the control of diabetes, and patient education provides opportunities for patients to learn about matters important in the prevention of ulcer formation and promotion of their cure such as relieving weight and maintaining cleanliness through improved washing methods. In addition, it has been reported that patient education is important for controlling various symptoms of diabetes other than ulcers.328
- Education about the foot as well as normalizing blood sugar control is necessary for diabetic patients.329 In particular, it is important to provide guidance to the patient or caregiver to examine the feet daily.330
- Climate therapy such as bathing in hot springs is widely performed among diabetic patients. In pressure ulcer patients, the bacterial load has been shown to decrease with increases in localized blood flow caused by bathing, and bathing is defined by textbooks as a skin care technique and is recommended as part of treatment. Conversely, in diabetic skin ulcers, inappropriate foot bathing may induce infection, and so a diabetic ulcer is considered by some to be a contraindication to foot bathing, but the evidence is unclear. Hot spring bathing is widely performed as a folk therapy for diabetes. However, diabetic patients are more active than pressure ulcer patients, and they may have more opportunities to bathe far from the supervision by medical professionals. On such occasions, there is the possibility of sustaining burn injuries due to desensitization caused by diabetic peripheral neuropathy in addition to the risk of infection.331, 332 Therefore, bathing is recommended with the condition that appropriate guidance for bathing and skin care are provided.
- There is a report on bathing that carbon dioxide baths prevent the formation and enlargement of ischemic ulcers in diabetes patients with a severe ischemic limb who have undergone vascular reconstruction surgery,333 but there is also a report that heat stimulation of diabetes patients did not cause a significant increase in blood flow compared to healthy individuals.334
CONFLICT OF INTEREST STATEMENT
Takafumi Kadono is the Editor-in-Chief of Journal of Dermatology and a co-author of this article. Dr Kadono is excluded from editorial decision-making related to the acceptance and publication of this article. Minoru Hasegawa and Hideki Fujita are Editorial Board members of Journal of Dermatology are co-authors of this article. To minimize bias, they were excluded from all editorial decision-making related to the acceptance of this article for publication.