Development of Entrustable Professional Activities and Standards in Training in Pediatric Neurogastroenterology and Motility
North American Society for Pediatric Gastroenterology, Hepatology and Nutrition and American Neurogastroenterology and Motility Society Position Paper
This article has been developed as a Journal CME and MOC Part II Activity by NASPGHAN. Visit https://learnonline.naspghan.org/ to view instructions, documentation, and the complete necessary steps to receive CME and MOC credits for reading this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal's Web site (www.jpgn.org).
Drs Leonel Rodriguez and Jaime Belkind-Gerson are senior co-authors.
The authors report no conflicts of interest.
ABSTRACT
Neurogastroenterology and motility (NGM) disorders are common in childhood and are often very debilitating. Although pediatric gastroenterology fellows are expected to obtain training in the diagnosis and management of patients with these disorders, there is an ongoing concern for unmet needs and lack of exposure and standardized curriculum. In the context of tailoring training components, outcome and expressed needs of pediatric gastroenterology fellows and programs, members of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) and American Neurogastroenterology and Motility Society (ANMS) developed guidelines for NGM training in North America in line with specific expectations and goals of training as delineated through already established entrustable professional activities (EPAs). Members of the joint task force applied their expertise to identify the components of knowledge, skills, and management, which are expected of NGM consultants. The clinical knowledge, skills and management elements of the NGM curriculum are divided into domains based on anatomic regions including esophagus, stomach, small bowel, colon and anorectum. In addition, dedicated sections on pediatric functional gastrointestinal (GI) disorders, research and collaborative approach, role of behavioral health and surgical approaches to NGM disorders and transition from pediatric to adult neurogastroenterology are included in this document. Members of the NASPGHAN-ANMS task force anticipate that this document will serve as a resource to break existing barriers to pursuing a career in NGM and provide a framework towards uniform training expectations at 3 hierarchical tiers corresponding to EPA levels.
Graphical Abstract
An infographic is available for the article at: http://links.lww.com/MPG/C11.
Neurogastroenterology and motility (NGM) disorders are common in childhood and are often very debilitating. As in adults, they are among the most challenging diagnoses to make and treat effectively. These pediatric disorders occur within a developing bowel, exhibit different pathophysiology than in adult patients, and often require distinct diagnostic and management approaches that must take developmental age and caregivers into consideration. A recent study noted that although pediatric gastroenterology fellows are expected to obtain training in the diagnosis and management of patients with NGM disorders, unmet needs and lack of exposure and standardized curriculum remain of ongoing concern (1.). In the context of tailoring training components, outcome and expressed needs of pediatric gastroenterology fellows and programs, members of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) initiated a project to define expectations for NGM training in North America. The project extended to a collaborative joint task force with the American Neurogastroenterology and Motility Society (ANMS). Members of the joint task force developed guidelines for training in pediatric NGM and applied their expertise to identify the components of knowledge, skills, and management, expected of NGM consultants.
LEVELS OF COMPETENCY
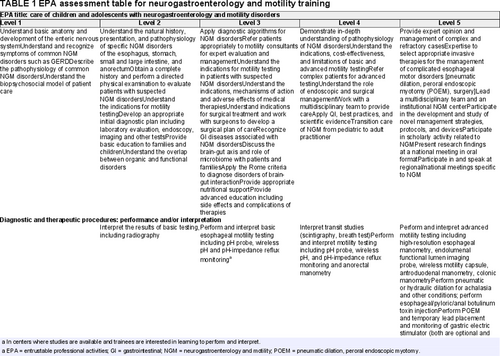
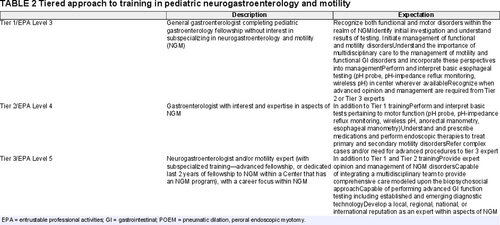
Medical training has shifted in recent years from an apprenticeship and time-based model to an outcomes-based system focused on key domains of medical practice, known as core competencies (2.). In this system, the specific expectations and goals of training are delineated through milestones and entrustable professional activities (EPAs) (3.). EPAs are critical activities performed by medical professionals that can be observed and assessed. Common EPAs for all pediatric subspecialties were developed by the American Board of Pediatrics, and 5 EPAs specific to pediatric gastroenterology, hepatology and nutrition were developed by the NASPGHAN EPA Task Force (4., 5.). An additional EPA in NGM was developed concomitantly with these guidelines (Table 1), reviewed by senior members of the NASPGHAN EPA task force, and is appended. The ANMS has previously endorsed guidelines for training in adult NGM, which are based on a 3-tiered approach (6.). As the pediatric NGM training guidelines presented herein are a joint venture between NASPGHAN and ANMS and should be understandable to both pediatric and adult motility consultants, both frameworks are utilized, with EPA level 3 corresponding to Tier 1, EPA level 4 corresponding to Tier 2, and EPA level 5 corresponding to Tier 3.
METHODS
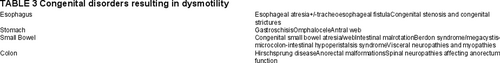
Recognizing the unmet needs and knowledge gap in the field of NGM, both NASPGHAN and the ANMS have actively conducted several activities with the main objectives of standardizing and improving the quality of training in this field (7.). As the learning and practice environment shifted towards highly specialized gastroenterology careers including NGM, it is important for educators and educational programs to develop strategies to provide relevant training to the trainee with specific career interests. Consequently, both the educational program and the trainee need to recognize elements of training that are essential to the trainee's career and take ownership of the timing and content of learning (6.). A tiered approach to training with corresponding EPA levels (Table 2) serves this purpose, where the trainee is provided training and knowledge that directly relates to the requirements of the training program, to gravitate toward their subspecialty niche of interest. It is important to note that a consultant, based on their career interest, may achieve EPA Level 4 or 5 (Tier 2 or 3) status in a particular area or anatomic region within NGM field and can choose to focus on clinical practice, clinical, translational or basic science research and combination thereof. Finally, the differences between children and adults are important to highlight, as both the evaluation and treatment tend to be different, particularly for congenital and neonatal conditions. Therefore, training in NGM, as in all pediatric subspecialties has the added challenge of teaching the management of different diseases, accounting for different ages of presentation. Although similar names for the syndromes/diseases are often used, the diagnostic and therapeutic approaches may differ greatly depending on the age group (eg, gastroparesis in a premature neonate vs gastroparesis in a teenager). A broad list of congenital abnormalities that often result in gastrointestinal dysmotility as part of the specific syndromes can be found in Table 3.
It is important to note that this curriculum is based on shared expert opinion by the members of the NASPGHAN-ANMS task force and should serve as a guide for training pediatric gastroenterology fellows and young faculty with NGM focus in an academic as well as community practice settings. The document is not meant to be prescriptive, and the task force did not try to establish precise rotation structure, procedure number, and interpretation expectations as part of the NGM training. It is, however, expected that all pediatric gastroenterology fellows have a working knowledge of common NGM disorders and achieve EPA Level 3 or Tier 1 assessment tool training before graduating. For example, a trainee who does not plan to pursue further training in NGM would be expected to achieve an entrustment level of 3 (trusted to execute with supervision at a distance) for most of the tasks listed. EPA Level 4 and 5 or Tiers 2 and 3 training can be achieved by different pathways. For examples, 1 can achieve the skills and acquire knowledge within the context of a standard 3-year pediatric gastroenterology fellowship in a center with a NGM expert or pursue further training (fourth year Advanced Fellowship in Pediatric Neurogastroenterology) offered by some centers, and ultimately by working alongside NGM faculty in a neurogastroenterology center.
Regardless of the pathway chosen to develop the necessary skills to practice as a pediatric NGM specialist, both mentors and those in training should follow the standards discussed in this training guideline.
The clinical knowledge, skills and management elements of the NGM curriculum are divided into domains based on anatomic regions including esophagus, stomach, small bowel, colon and anorectum. In addition, we include a dedicated section on pediatric functional GI disorders followed by section focusing on research and collaborative approach. We also include the roles of behavioral health and surgical approaches to NGM disorders. A section on pediatric transition to adult neurogastroenterology is also included in this document. All pediatric gastroenterology trainees are expected to have the knowledge and understanding of conditions that could mimic NGM disorders; thus, these were not included in this document. In particular, mucosal disorders, such as eosinophilic esophagitis (along with other eosinophilic gastrointestinal disorders), Helicobacter pylori gastritis, celiac disease, inflammatory bowel disease (IBD), and so forth.
Specific Anatomic Regions for Consideration
Esophageal Motor Disorders
Oropharyngeal and esophageal motor disorders can present with dysphagia, heartburn, regurgitation, aspiration, chest pain, food impaction, and/or weight loss. Some unique aspects are related to the care of the pediatric patient with esophageal motor disorders. It is important to recognize that other conditions like eosinophilic esophagitis and gastroesophageal reflux disease can present with same symptoms in pediatric patients. In addition, the general pediatric gastroenterologist should be aware of congenital and acquired conditions associated with esophageal dysmotility including esophageal atresia, connective tissue disorders, and prior fundoplication surgery, in addition to primary motor disorders, such as achalasia and secondary disorders like scleroderma. Furthermore, as pediatricians, it is important to understand the long-term implications (including into adulthood) for esophageal motility disorders including risk of erosive reflux disease, Barrett esophagus, esophageal strictures, and chronic lung disease.
It is also important to understand the unique issues related to esophageal testing in children including prescription drugs, such as antipsychotics, sedatives, and anesthetics, which affect results, nuances of how to feed infants, and children during testing, and the difficulty assessing symptoms during testing in nonverbal or very young children.
As esophageal motility disorders may be lifelong, it is important to provide multidisciplinary support whenever possible to patients and their families and recognize the need for transition of care to adult gastroenterology colleagues whenever appropriate.
EPA Level 3 (Tier 1) consultant should understand the basic physiology of normal oropharyngeal and esophageal motor function, common disorders arising from dysfunction, utilization of esophageal function testing to diagnose these disorders, and initial management. In addition, perform and interpret basic esophageal testing (pH probe, wireless pH, and pH-impedance reflux monitoring) in centers wherever available.
EPA Level 4 (Tier 2) consultant should be able to perform basic esophageal testing (pH probe, wireless pH, and pH-impedance reflux monitoring), understand the indications, basic interpretation, utilization, limitations, and complications of diagnostic esophageal motor testing and management of esophageal motor disorders.
EPA Level 5 (Tier 3) consultant should have a detailed understanding of oropharyngeal and esophageal pathophysiology, provide performance, and expert interpretation of esophageal function tests, and coordinate the management of motor disorders and their consequences including assessment of complications from esophageal surgery and endoscopic procedures.
Entrustable Professional Activities Level 3 Consultant
Knowledge
- Understand the anatomical and functional/regulation differences between the oropharynx and the upper and lower esophagus and its implications on motility dysfunction.
- Understand the presenting signs and symptoms of gastroesophageal reflux disease (GERD).
- Understand the pathophysiology of GERD.
- Understand the medical and surgical therapies for gastroesophageal reflux and limitations of these therapies including side effects.
- Describe the pathophysiology, diagnosis, management, and complications of achalasia.
Assessment
- Understand the investigation of esophageal symptoms, particularly transit symptoms (dysphagia, esophageal regurgitation) that can lead to a diagnosis of esophageal motor disorders.
- Differentiate oropharyngeal from esophageal dysphagia and provide appropriate investigation and management, including recommendations for enteral feeding whenever appropriate.
- Comprehend diagnostic algorithms for oropharyngeal and esophageal dysphagia and develop knowledge to request appropriate diagnostic testing.
- Recognize situations where endoscopic intervention is indicated for the short-term and long-term management of esophageal motor disorders.
Testing
- Understand the role of reflux testing (pH probe, pH-impedance reflux monitoring, wireless pH) in the patients with suspected reflux and know the technical limitations to the study, and perform and interpret in centers where available and trainee is interested in learning.
- Understand when to refer for esophageal motility testing.
Management
- Create a differential diagnosis and therapeutic plan for patients presenting with feeding difficulties, regurgitation, chest pain, and dysphagia.
- Provide effective education, reassurance, and support for patients and their parents.
- Recognize when and how to refer for behavioral and dietary therapies.
Entrustable Professional Activities Level 4 Consultant
Knowledge
- Understand in-depth physiology of oropharyngeal and esophageal contractility and peristalsis including neurohormonal regulation of deglutition and overlap with functional disorders.
- Describe the pathophysiology, diagnosis, management, and complications of major esophageal motor disorders, including esophagogastric junction (EGJ) outflow obstruction, aperistalsis, distal esophageal spasm, and hypercontractile esophagus.
- Recognize congenital disorders associated with dysmotility.
Assessment
- Recognize conditions that may mimic or confound the diagnosis of esophageal motor disorders, including eosinophilic esophagitis, functional dysphagia, esophageal diverticula, organic obstructive syndromes, nonerosive reflux disease (NERD) and GERD.
- Understand the symptoms, complications, and workup needs in the post-operative esophagus including patients who have had fundoplication or patients who have had esophageal surgery.
Testing
- Appreciate the indications, limitations, complications, and cost-effectiveness of diagnostic esophageal function studies, especially endoscopy, esophageal high-resolution manometry (HRM), and contrast radiography, for the diagnosis and guidance of management of esophageal motor disorders.
- Perform and interpret pH probe, wireless pH, and pH-impedance probe testing.
Management
- Understand the impact of anti-reflux surgery on esophageal function and craft a diagnostic workup for symptomatic patients who had anti-reflux surgery.
- Understand the clinical sequelae of esophageal motor dysfunction and their management.
- Understand the pharmacology, efficacy, routes of administration, and appropriate use of medications for esophageal motor disorders.
- Understand the pulmonary manifestations of GERD and other esophageal motor disorders and be able to work on a multidisciplinary team including aerodigestive teams to optimize diagnosis and treatment.
- Understand the pathophysiology of NERD and visceral hypersensitivity syndromes with esophageal symptoms and how to treat these.
- Recognize circumstances where surgical intervention is indicated for the short-term and long-term management of esophageal motor disorders.
Entrustable Professional Activities Level 5 Consultant
Knowledge
- Understand the implications and management of minor motor disorders: ineffective esophageal motility, fragmented peristalsis.
- Understand the evaluation and management of complications, and recurrent symptoms following initial management of primary and secondary motor disorders.
- Have the expertise to train others in the field.
Assessment
- Distinguish overlapping functional esophageal symptoms from motor disorders and provide management recommendations
Testing
- Provide expertise, performance, and interpretation of advanced, emerging investigative, and therapeutic modalities including esophageal HRM, endolumenal functional lumen imaging probe, and postprandial HRM to asses for rumination.
Management
- Provide opinion and expert management of oropharyngeal and esophageal motor disorders within the context of age and comorbid conditions.
- Recognize appropriate patients for complementary and adjunctive therapies for functional esophageal disorders.
- Have the expertise to select appropriate invasive therapies for the management of complicated esophageal motor disorders [pneumatic dilation, peroral endoscopic myotomy (POEM), surgery]; perform pneumatic or hydraulic dilation for achalasia; perform POEM after requisite advanced endoscopic training to acquire necessary skills, which can last up to a year.
- Develop or join a state-of-the-art referral center for evaluation and management of esophageal motor disorders.
Gastric Motor Disorders
Gastric motor disorders, including gastroparesis are frequently seen in the pediatric population and often present with vomiting, early satiety, nausea, fullness, abdominal pain, abdominal distension, and weight loss. It is important to recognize that gastric outlet obstruction and gastric mucosal disorders can mimic symptoms of gastroparesis. It is, therefore, imperative to rule these out before embarking on diagnosing gastric motor disorders. EPA Level 3 (Tier 1) consultant should understand the physiology of gastric neuromuscular function and embryology of congenital gastric disorders. The consultant should also develop an understanding of the clinical presentation and course, initial management, and indications and basic interpretations of diagnostic testing of gastric disorders. EPA Level 4 (Tier 2) consultant should have a detailed understanding of the pathophysiology of gastric disorders, their presentations in both typical and atypical cases, and their management, including pharmacologic, endoscopic, and surgical interventions. In addition, the consultant should be able to utilize and interpret imaging studies (gastric scintigraphy, contrast studies) and apply findings from manometric (antroduodenal manometry, wireless motility capsule) diagnostic tests.
Finally, the consultant should understand the overlap of functional and motor disorders of the stomach both from a symptom and management perspective. EPA Level 5 (Tier 3) consultant should develop expert knowledge of the medical and surgical comorbidities of complex gastric disorders, provide expert interpretation of motor and accommodative testing in the context of these comorbidities, and lead multidisciplinary teams for cutting-edge and novel noninvasive and invasive management of pediatric gastric motor and sensory disorders.
Entrustable Professional Activities Level 3 Consultant
Knowledge
- Describe the developmental origin of the foregut and enteric nervous system and recognize its relevance to congenital disorders of the stomach.
- Understand the anatomy and physiology of the stomach.
- Have a basic understanding of gastric function and recognize the clinical presentation of disorders of motility and sensation.
Assessment
- Recognize most common primary and secondary etiologies for gastric motor disorders.
- Recognize conditions that may mimic or confound the diagnosis of gastric motor disorders including systemic, metabolic, anatomic, and mucosal diseases.
- Apply age-specific current Rome criteria to identify and differentiate functional gastric disorders.
Testing
- Recognize the indication and utility of abdominal X-ray, contrast X-ray, and gastric scintigraphy in the diagnosis and evaluation of gastric disorders.
- Understand the indications for antroduodenal manometry testing in the diagnosis and management of suspected gastric motor disorders.
- Understand the role of other less established modalities, such as wireless motility capsule and breath tests for measurement of gastric emptying in the diagnostic evaluation of gastric disorders.
Management
- Develop pharmacologic and nonpharmacologic strategies for acute and chronic gastroparesis.
- Understand the diagnostic overlap between gastroparesis and functional dyspepsia and other functional gastric disorders.
- Provide effective education, reassurance, and support for patients and their parents.
- Recognize when and how to refer for behavioral and dietary therapies.
Entrustable Professional Activities Level 4 Consultant
Knowledge
- Recognize the contributions of neurogenic and myogenic function in disorders of gastric motility (accommodation, mixing, and emptying) and sensation.
- Understand the natural history, epidemiology, pathophysiology, and surgical treatment of gastroparesis and other gastric motility disorders.
- Able to identify functional gastrointestinal disorders mimicking and overlapping with a gastric motility problem.
- Recognize gastric congenital disorders associated with dysmotility.
Assessment
- Recognize the role of infection/inflammation and systemic diseases, such as diabetes as well as anatomical mechanical gastric obstruction (eg, gastric volvulus, webs, etc) in the clinical setting.
- Describe the diagnostic (radiographic, manometric, endoscopic) and treatment approaches (medical, surgical) for the management of gastric motility and sensory disorders.
Testing
- Have the expertise to perform and/or interpret endoscopic and transit studies (scintigraphy, breath test, wireless motility capsule).
- Recognize the role of antroduodenal manometry and be able to apply the findings of this test in the medical and surgical management of gastric disorders.
Management
- Develop a treatment strategy for symptomatic gastroparesis including dietary and lifestyle approaches, prokinetics, neuromodulators, nausea-reducing agents known to help with gastric accommodation and be aware of novel therapeutics.
- Understand the role of endoscopic (eg, pyloric dilation, pyloric botulinum toxin injection) and surgical (pyloroplasty, gastric electrical stimulator) management for gastric dysfunction including the use of gastric or jejunal feeding tubes for nutritional improvement.
- Know how to evaluate and treat dumping syndrome secondary to vagal lesions, pyloromyotomy, postsurgical, and so forth.
- Recognize the role of biofeedback in the management of these disorders.
Entrustable Professional Activities Level 5 Consultant
Knowledge
- Be able to describe the anatomy and physiology of the enteric nervous system and target cells, the components of the gastric anatomy as well as the connections with the autonomic and central nervous systems.
- Be able to identify the major signaling mechanisms and neurotransmitters in the stomach and how pharmacological agents target these mechanisms.
- Develop advanced knowledge of primary endoscopic and surgical management and the postsurgical sequela of gastric emptying/accommodation disorders, such as postinfectious and diabetic gastroparesis.
- Have the expertise to train others in the field.
Assessment
- Utilize radiographic modalities in the diagnosis and management of complex gastric disorders in the context of pre-existing medical and surgical comorbidities.
- Develop expert knowledge in the clinical value of gastric scintigraphy, upper gastrointestinal series, endoscopic evaluation, antroduodenal manometry, wireless motility capsule and others, in the guidance of medical and surgical management of gastric dysmotility.
Testing
- Expert application, performance, and interpretation of antroduodenal manometry studies.
- Appreciate the limitations, cost-effectiveness, and implications of antroduodenal manometry testing in the diagnosis and management of gastric disorders.
- Expert application and interpretation of gastric function studies (emptying, accommodation, electrical activity, etc).
Management
- Provide expert consultation, including manometric evaluation and management of complex gastric disorders.
- Develop expert knowledge and recognize the clinical indications and limitation of invasive therapies for the management of gastric disorders including botulinum toxin injections, gastric electrical stimulation, vagal nerve stimulation, surgical pyloroplasty, pyloric dilation, and need for G-tube/J-tube for venting and/or nutrition.
- Expertise in management of chronic pain including use of neuromodulating medications and indication for use of nonmedical interventions, such as behavioral, acupuncture, and herbal treatments.
- Be able to assess the clinical value of gastric electrical stimulator for management of gastric disorders (in rare cases, be able to assist, and/or perform the temporary lead placement and the monitoring of gastric electrical stimulators).
- Develop or join a state-of-the-art referral center for evaluation and management of gastric motor disorders.
Small Bowel Motor Disorders/Intestinal Failure
Small bowel motility disorders present significant challenges in clinical care despite important progress in our understanding of pathophysiology. Small bowel motor diseases may present with symptoms including feeding intolerance, abdominal distension, ileus, vomiting, weight loss/failure to thrive, constipation, diarrhea, and/or abdominal pain. The severity of the symptoms can range from mild and intermittent to persistent and disabling. The latter represents the end of the spectrum of intestinal dysmotility, pediatric intestinal pseudo-obstruction (PIPO), which can be primary or secondary and can result in intestinal failure. Differentiating this condition from disorders that mimic intestinal dysmotility (like functional abdominal pain, fictitious disorders, and behavioral/psychiatric conditions) is paramount to avoid the performance of unnecessary procedures and interventions. EPA Level 3 (Tier 1) consult should understand the physiology of normal intestinal motor function, common disorders arising from dysfunction, utilization and basic interpretation of intestinal function testing to diagnose these disorders and be able to provide initial management of intestinal dysmotility. EPA Level 4 (Tier 2) consultant should understand the indications, interpretation, utilization, limitations, and complications of advanced small bowel motility testing, and management of small bowel motor disorders and intestinal failure. In addition, Tier 2 consultant should be able to integrate a multidisciplinary team to evaluate patients with small bowel dysmotility and intestinal failure. EPA Level 5 (Tier consultant should have the expertise in evaluating and treating small bowel motility disorders, be able to perform advanced small bowel motility testing, develop a multidisciplinary team and cultivate a referral center, and achieve the expertise to teach and train others and advance the knowledge of the field.
Entrustable Professional Activities Level 3 Consultant
Knowledge
- Understand the embryological origin of the small bowel (midgut) and its relevance to congenital and acquired small bowel motor dysfunction.
- Recognize the presence of intestinal motor disorders and be able to recommend initial testing and interpretations of testing including radiologic imaging.
- Recognize key etiologies contributing to small bowel dysmotility including systemic, metabolic, anatomic, and mucosal diseases.
- Understand the medications, which affect small bowel motility.
- Understand nutritional support options and be familiar with the complications associated with motility disorders, and their prevention and treatment.
Assessment
- Perform a thorough clinical interview and physical examination aiming to identify conditions leading to small bowel dysmotility.
Testing
- Understand the role of imaging studies and the indications, basic interpretation, and clinical utility of transit studies.
- Understand the indications to refer patients for consultation for advanced gastrointestinal motility studies (eg. wireless motility capsule, antroduodenal manometry).
Management
- Indicate therapies aimed at improving symptoms related to small bowel dysmotility.
- Recognize situations where endoscopic and/or surgical intervention is indicated for the short-term and long-term management of small bowel motor disorders.
- Recognize the clinical indications for referral for an expert evaluation and treatment.
- Provide effective education, reassurance, and support for patients and their parents.
- Recognize when and how to refer for behavioral and dietary therapies.
Entrustable Professional Activities Level 4 Consultant
Knowledge
- Recognize the role of systemic disease, side effects of medications, and consequences of bowel surgery as a mechanism for small bowel motor dysfunction, intestinal failure, and bowel transit problems leading to symptoms.
- Recognize the implications of secondary motility disorders (eg, autoimmune conditions, post-infectious, medication-related, and spinal cord abnormalities) on patient presentation, evaluation, and response to therapy.
- Recognize the clinical value of imaging, scintigraphic modalities, and wireless motility capsule in the diagnosis and management of small bowel motility disorders.
- Have the knowledge and expertise in the use of advanced pharmacological and nonpharmacological treatments of motility disorders.
Assessment
- Identify functional gastrointestinal disorders mimicking small bowel motor disorders and differentiate those from pediatric intestinal pseudo-obstruction.
Testing
- Understand the indications, interpretation, clinical utility and limitations of transit studies, and provide recommendations based on those results.
- Understand the clinical utility of the advanced motility studies (antroduodenal manometry, wireless motility capsule), and to provide recommendations based on study results.
Management
- Integrate a multidisciplinary team for evaluation and treatment of small bowel motor disorders.
- Understand the indications and complications of enteral and parenteral nutrition.
- Understand the indications and side effects of medical therapies aiming to improve symptoms related to small bowel motor dysfunction.
- Understand the indications and complications of interventional therapeutic procedures and able to perform those, including endoscopic dilation of strictures and placement of feeding tubes.
- Understand the indications and complications associated with surgical procedures aiming to improve enteral tolerance.
- Understand the indications and complications of surgical interventions, including central venous catheter placement, ostomy creation, and placement of feeding tubes for enteral access.
Entrustable Professional Activities Level 5 Consultant
Knowledge
- Have the expertise in advanced management of nutrition needs, including enteral and parenteral nutrition and its complications, utilization of surgical ostomy in management of small bowel motor disorders and intestinal failure.
- Recognize and implement treatment of small bowel motor disorders, including prokinetics, neuromodulators, and symptomatic relief agents.
- Have the expertise to train others in the field.
Assessment
- Recognize patients who might benefit from surgical interventions including small bowel transplantation, ostomy, and colectomy for advanced and complex small bowel motor disorders.
- Develop a treatment algorithm for patients with an ostomy who have complications.
Testing
- Master the abilities to perform, interpret and understand the cost-effectiveness of the antroduodenal manometry and wireless motility capsule, including its potential complications and the management of those.
- Maintain proficiency on the performance of the test and develop expertise to teach others.
- Participate in the design and implementation of protocols for new devices and/or techniques to evaluate small bowel motility.
Management
- Develop or join a state-of-the-art referral center for evaluation and management of small bowel motor disorders.
- Expert understanding of the indications, limitations, side effects and cost-effectiveness of nutritional interventions, including parenteral nutrition, and develop a systematic approach to prevent such complications.
- Successfully cultivate a multidisciplinary team for evaluation and treatment of small bowel motor disorders.
- Expert understanding of the indications, limitations, side effects and cost-effectiveness of medical interventions aimed at improving intestinal motor function (eg, pyridostigmine and octreotide), particularly those that require special protocols (eg, compassionate care program for cisapride).
- Expert performance of interventional endoscopic therapeutic procedures (like dilation of strictures and assistance with enteral tube placement), including their indications, limitations, complications, and cost-effectiveness.
- Participate in the design and implementation of protocols for new devices and/or techniques to treat small bowel motor disorders (eg, intestinal pacing).
Anorectal and Colonic Disorders
Anorectal and colonic disorders, including colonic dysmotility, anorectal malformations, Hirschsprung disease (HD), and neurogenic bowel may present with refractory constipation, diarrhea, fecal incontinence, abdominal distention, vomiting, and obstructive symptomatology. EPA Level 3 (Tier 1) consultant should understand the physiology of anorectal and colonic neuromuscular function and embryology of congenital colorectal disorders. The consultant should develop an understanding of the clinical presentation and course, initial management, and indications and basic interpretation of diagnostic testing of colorectal disorders including colonic dysmotility, refractory constipation and fecal incontinence, anorectal malformations, HD, and neurogenic bowel. EPA Level 4 (Tier 2) consultant should have a detailed understanding of colorectal disorders and their presentation and management, including pharmacologic and surgical interventions. The consultant should be able to utilize and fully interpret radiographic (colonic scintigraphy, defecography, radiopaque marker study, contrast enema) and manometric (anorectal and colonic manometry) diagnostic tests. EPA Level 5 (Tier 3) consultant should have expert knowledge of the medical and surgical comorbidities of complex colorectal disorders, perform advanced motility testing, and provide expert interpretation in the context of these comorbidities, and lead multidisciplinary teams for the advanced noninvasive and invasive management of pediatric anorectal and colonic motor disorders.
Entrustable Professional Activities Level 3 Consultant
Knowledge
- Describe the developmental origins of the hindgut and enteric nervous system and recognize the relevance to congenital disorders of the colon and anorectum.
- Understand the anatomy and physiology of the colon and pelvic floor.
- Develop a basic understanding of colonic and anorectal function and recognize the clinical presentation of disorders of motility and sensation.
Assessment
- Recognize key primary and secondary etiologies for colonic motor disorders including neurogenic and myogenic processes.
- Recognize conditions that may mimic or confound the diagnosis of colonic and anorectal disorders including systemic, metabolic, anatomic, and mucosal diseases.
- Obtain relevant age-specific history and perform a directed physical examination to identify primary and secondary etiologies of colorectal disorders.
Testing
- Recognize the utility of abdominal X-ray and radiopaque markers in the diagnosis and evaluation of colorectal disorders.
- Understand the role of imaging including contrast enema, colonic scintigraphy, defecography, and lumbo-sacral MRI in the diagnostic evaluation of colorectal disorders.
- Appreciate the indications for anorectal and colonic manometry testing in the diagnosis and management of colorectal disorders.
- Understand the role of radiographic imaging and manometric testing in the evaluation of defecation disorders in congenital colorectal disorders including HD and anorectal malformations (ARM).
- Recognize when rectal biopsy to screen for HD is indicated.
Management
- Develop pharmacologic and nonpharmacologic strategies for acute and chronic constipation.
- Recognize and develop a management plan for retentive and nonretentive fecal incontinence.
- Recognize the presentation of HD-associated enterocolitis (HAEC) and be able to initiate an appropriate treatment strategy.
- Provide effective education, reassurance, and support for patients and their parents.
- Recognize when and how to refer for behavioral and dietary therapies.
Entrustable Professional Activities Level 4 Consultant
Knowledge
- Recognize the contributions of neurogenic and myogenic function in disorders of colorectal motility and sensation.
- Describe the natural history, epidemiology, pathophysiology, and surgical treatment of HD and ARM.
Assessment
- Recognize the role of histopathology and anatomical mechanical obstruction in HD and ARM who present with postoperative defecation disorders, including obstructive symptoms and fecal incontinence.
- Describe the diagnostic (radiographic, manometric) and treatment approaches (medical, surgical) for the management of postoperative defecation disorders in HD and ARM.
- Recognize the symptoms, complications and workup in the postoperative colon including patients who have had antegrade continence enemas, surgical resection, and intestinal diversion.
Testing
- Have the expertise to perform and interpret anorectal manometry studies.
- Recognize the role of colonic manometry and be able to apply the findings in the medical and surgical management of colorectal disorders.
Management
- Develop a treatment strategy for refractory constipation and fecal incontinence including novel therapeutics, retrograde enemas, and antegrade continence enemas.
- Understand the role of surgical management and its complications for colonic dysfunction including antegrade continence enemas, surgical resection, intestinal diversion, and anal botulinum toxin injection.
- Have expertise in management of antegrade continence enemas and retrograde continence enema regimens.
- Recognize the role of a team-based approach.
Entrustable Professional Activities Level 5 Consultant
Knowledge
- Be able to describe the anatomy and physiology of the enteric nervous system, the components of the colonic wall as well as the connections with the autonomic and central nervous systems.
- Be able to identify the major signaling mechanisms and neurotransmitters in the colonic wall and how pharmacological agents target these mechanisms.
- Have advanced knowledge of primary surgical management and the postsurgical sequela of defecation disorders in HD and ARM.
-
Have the expertise to train others in the field
Assessment
- Utilize radiographic modalities in the diagnosis and management of complex colorectal disorders in the context of pre-existing medical and surgical comorbidities.
- Have expert knowledge in the clinical value of anorectal and colonic manometry in the guidance of medical and surgical management of colonic dysmotility and postsurgical obstructive symptoms in HD and ARM.
Testing
- Expert application, performance, and interpretation of anorectal manometry studies.
- Expert application, performance and interpretation of colonic manometry studies.
- Appreciate the limitations, cost-effectiveness, and implications of anorectal and colonic manometry testing in the diagnosis and management of colorectal disorders.
Management
- Provide expert consultation, including manometric evaluation, and management of complex colorectal disorders.
- Develop a multidisciplinary team for the management of complex colorectal disorders.
- Have expert knowledge and recognize the clinical indications of invasive therapies for the management of colorectal disorders including botulinum toxin injections, antegrade continence enemas, sacral nerve stimulation, surgical resection and intestinal diversion, and re-do of complex anorectal surgical pull-throughs for HD and ARM.
- Develop or join a state-of-the-art referral center for evaluation and management of anorectal and colonic motor disorders.
Pediatric Functional Gastrointestinal Disorders/Disorders of the Gut-Brain Interactions
The majority of children and adolescents referred to a pediatric GI clinic present with symptoms that are ultimately attributed to disorders of the gut-brain interaction (DGBI). These disorders, also known as functional gastrointestinal disorders (FGIDs), are prevalent in the pediatric population. Symptoms associated with FGIDs, including nausea, early satiety, vomiting, constipation, abdominal pain, bloating, diarrhea can significantly impact a patient's well-being and quality of life. The psychosocial and financial burden on these patients and families is also significant. Moreover, these disorders have the potential to frustrate the medical provider, the patient and family, and may lead to severe disability.
FGID is a symptom-based diagnosis, and it is imperative to apply age-specific current Rome criteria. As the diagnosis is primarily dependent on a detailed history and thorough physical examination with limited and purposeful evaluation, the provider must have a genuine appreciation of these disorders and practices. This appreciation and ability to translate it into practice may come naturally to some but it can also be taught and modeled. As FGIDs are ubiquitous, all gastroenterologists should be well informed on the brain-gut axis and the role of microbiome as well as the general principles of treatment options and planning.
For pediatric gastroenterologists to have both diagnostic and therapeutic success, it is vital that the expert can demonstrate the following skills: understand the diagnosis is a positive diagnosis and not 1 of exclusion, establish a genuine and effective patient-parent-provider relationship, master patient-friendly language when discussing gut-brain pathways and visceral hypersensitivity, be familiar with a variety of pharmacologic, nonpharmacologic, and dietary therapy options and the rationale for recommending these interventions, demonstrate consideration of illness severity and the patient/family's ability to follow through with recommendations when generating a treatment plan, and work effectively within a multidisciplinary team. It is also imperative for pediatric gastroenterologists to demonstrate the ability to assess for genetic, medical, and psychological risk factors, triggers, and vulnerabilities that may contribute to the onset, exacerbation, and maintenance of a FGID and to appropriately incorporate and discuss the importance of these findings during the feedback component of a clinic visit.
The Rome Criteria for FGIDs have been instrumental in providing the necessary tools to develop criteria-based diagnosis and a biopsychosocial treatment plan. We aim to create training standards that will guide the career development of pediatric gastroenterologists by clearly outlining the steps and objectives that pediatric gastroenterologists should attain as they grow their ability to diagnose and manage FGIDs. These standards are divided into 3 tiers, with practitioners at successive levels demonstrating increasingly advanced and nuanced skill sets.
EPA Level 3 (Tier 1) consultant should understand and have an appreciation of FGIDs and the important roles of microbiome and brain-gut axis. The consultant should be able to establish a positive diagnosis by gathering a detailed history, conducting a comprehensive physical examination, discussing the differential diagnosis and performing a thoughtful and balanced diagnostic evaluation if necessary. The consultant should also be able to demonstrate empathy and spend time educating the patient and the caregivers. The consultant should feel comfortable with the general principles of treatment options and planning, and understand when to refer to a neurogastroenterologist. EPA Level 4 (Tier 2) consultant should be familiar with visceral sensation of the GI tract and common FGID symptom triggers. The consultant should be comfortable recommending and initiating evidence-based basic and more advanced pharmacologic and/or nonpharmacologic therapeutic interventions including psychological and dietary therapies without delay. A consultant at this level should also be able to understand the link between FGIDs and common overlapping pain conditions (ie, headaches, postural orthostatic tachycardia syndrome [POTS]) and be prepared to discuss this link with patients and families. EPA Level 5 (Tier 3) consultant should have further expertise on overlapping pain conditions, the pathophysiology of FGIDs, and work to educate their colleagues. The consultant should know the limitations of the Rome criteria and be able to differentiate between overlapping symptoms of FGIDs and other GI disorders or non-GI functional disorders. The consultant should be able to develop individualized treatment plans for patients that integrate pharmacologic, nonpharmacologic, psychological, and dietary modalities based on illness severity and a patient/family's access to these interventions. The consultant should be able to work in collaboration with other service providers and be comfortable treating patients with complex FGIDs, including those that have become total parenteral nutrition (TPN)-dependent or dependent on enteral feedings because of pain. Consultants at this level should be able to identify the need for higher level of care, including pain rehabilitation centers or intensive outpatient treatment programs, for patients presenting with severe cases of FGIDs.
Entrustable Professional Activities Level 3 Consultant
Knowledge
- Understand normal motor and sensory physiology of the GI tract.
- Know how to apply the current Rome Criteria for all FGIDs.
- Explain underlying pathophysiology of FGIDs.
- Understand the importance and basic principles of the gut-brain axis and microbiome in FGIDs.
- Understand the role that visceral hypersensitivity plays in FGIDs.
- Understand the biopsychosocial model of illness.
- Be capable of providing a differential diagnosis.
- Remain cognizant of the overlap between functional and organic gastrointestinal disorders.
- Demonstrate effective communication skills in order to discuss the diagnosis and treatment with patients and families.
Assessment
- Systematically obtain the history of presentation, triggers, developmental, medical and surgical history, psychosocial history (including previous psychological diagnoses), and family history (including medical, psychiatric, and pain history of family members).
Testing
- Recognize that children with FGIDs undergo excessive and unnecessary testing when a provider is searching for an organic cause of their presenting symptoms.
- Develop a limited evaluation based on a thoughtful differential diagnosis.
- Discuss evidence-based reasoning for the testing management.
- Provide education about the diagnosis, taking into consideration the developmental and cognitive levels of patients and family members.
- Establish a working patient-parent-provider relationship that, at its core, is based on effective communication.
- Recommend basic pharmacological and nonpharmacological treatments based on evidence when available including life-style modifications that have been shown to improve the condition.
- Recognize cases that requires interdisciplinary consultation and demonstrate competency in explaining the rationale behind making these referrals.
- Recognize the need to consult with or refer patients to a pediatric psychiatrist for appropriate pharmacological management of comorbid psychiatric and functional symptoms.
- Provide effective education, reassurance, and support for patients and their parents.
- Recognize when and how to refer for behavioral and dietary therapies.
Entrustable Professional Activities Level 4 Consultant
Knowledge
- Know how to assess for triggers of functional gastrointestinal symptoms.
- Understand the role that psychological, social, environmental, and academic stressors along with coping mechanisms play in symptom development and functional impairment.
- Incorporate information from multiple evidence-based resources when discussing functional disorders and overlapping pain conditions with patients and families.
- Understand the pharmacology and mode of action of pharmacologic and nonpharmacologic treatment of FGIDs.
Assessment
- Differentiate between functional GI symptoms and non-GI functional disorders or symptoms of other organic conditions.
Testing
- Limit unnecessary testing and understand the indication and utility of transit and motility studies in the evaluation of FGIDs.
Management
- Provide the needed education and assurance about the diagnosis and the variety of treatment options using language that is well understood by patients and families.
- Recommend individualized advanced pharmacologic, nonpharmacologic, psychological, and dietary therapies.
- Be familiar with neuromodulation.
Entrustable Professional Activities Level 5 Consultant
Knowledge
- Discern the effect that other systems (ie, immune or autonomic nervous systems) can have on FGIDs.
- Confidently assess health-related quality of life, symptom specific anxiety, coping early life adversity, and functional impairment.
- Recognize structure and core features of the most effective brain-gut psychotherapies, including cognitive behavioral therapy (CBT) and clinical hypnosis.
- Understand areas of controversy in the pathophysiology of these disorders.
- Be capable of addressing new entities and approaches.
Assessment
- Understand functional symptoms in the presence of other well-defined comorbid conditions like IBD, pancreatitis, celiac disease, and so forth.
- Be familiar with the assessment of hypermobility, postural orthostatic tachycardia syndrome (POTS), or presence of anterior cutaneous nerve entrapment syndrome (ACNES).
- Recognize other overlapping pain syndromes, beyond abdominal pain.
Testing
- Discuss evidence-based reasoning for the testing.
Management
- Develop an individualized treatment plan, which integrates various pharmacologic, nonpharmacologic, psychological, and dietary interventions.
- Recognize severe cases of pediatric FGIDs and work with a multidisciplinary team to facilitate admission to a higher level of care whenever necessary.
- Use the Multi-Dimensional Clinical Profile (MDCP) introduced in Rome IV to guide diagnoses.
- Have knowledge of specific nonpharmacologic interventions, like CBT, guided imagery, hypnosis, and so forth.
Research and Collaborative Approach
Throughout the tiered approach, implementing research and maintaining a solid infrastructure are major contributors for successful execution of patient care in NGM. EPA Level 3 (tier 1) consultant should be exposed to the main domains of clinical, translational and basic science research in the field of NGM. EPA Level 4 (Tier 2) consultant should apply findings from clinical, translational, and basic science studies to help guide patient care and seek opportunities to collaborate in clinical, translational, or basic science studies. EPA Level 5 (Tier 3) consultant should develop and/or actively contribute to clinical, translational, and/or basic research programs and begin to support and mentor trainees conducting research in the area of NGM. The consultant should be able to participate in the design, testing, and implementation of protocols for new pharmacologic agents, devices, and/or techniques to treat NGM disorders and gain ability to assess and monitor scientific advances for validity, rigor, and reproducibility. In addition, Tier 2 and 3 consultants should seek to participate in societal committees, councils, and consensus panels/documents in order to advance the NGM field.
Maintaining a collaborative team approach to care for patients with NGM disorders is an important skill set. EPA Level 3 and 4 (Tiers 1 and 2) consultants should recognize the role and collaborate with colleagues with specific expertise in pediatric surgery, nutrition, psychology/psychiatry, and physiotherapy. In addition, the consultant should be able to identify available resources for specific patient populations who would benefit from management by a multidisciplinary team or a tertiary motility center. EPA Level 5 (Tier 3) consultant should promote integration of a multidisciplinary team made up of pediatric gastroenterology, immunology, genetics, pediatric psychology, social work, nutrition, and other services including complementary medical, and physical therapy to provide a comprehensive care that is modeled upon the biopsychosocial approach.
Behavioral Health and Surgical Involvement in Neurogastroenterology and Motility Disorders
The chronic nature of NGM disorders can result in a reduced quality of life for patients, increased prevalence of adjustment-related difficulties, onset or exacerbation of internalizing mental health disorders, and family distress (8.). As such, treatment is often multidisciplinary and involves careful consideration of when and how to effectively consult a behavioral health provider who can address the social-emotional needs of the patients and their families and who can provide adjunctive, nonpharmacological strategies to reduce symptom triggers and physical discomfort while simultaneously helping patients to maintain or return to their ideal level of functioning (9.).
An important component of modern training in NGM is the interaction and involvement in interdisciplinary care with surgical colleagues. Pediatric GI training should allow fellows to interact with surgical colleagues in a supportive environment. Shared decision-making around failure of medical management, individualized care for patients and indications for surgical intervention are very important in patient treatment pathways and can only be fostered in interdisciplinary care models. Involvement of GI and surgery together in the treatment of achalasia, weighing antegrade enema options, and the need for colonic resection and neuro-modulation treatment options are important. Patient care is enhanced by interdisciplinary care between surgeons and physicians. Fostering these interactions during training will set a strong precedent for interactions during a working career.
Pediatric Transition to Adult Neurogastroenterology
Effective transition from pediatric to adult medical specialists often starts as early as 10 years of age and occurs across a life span. It is imperative to maintain health, as children become adults and is an essential process of communication between healthcare providers. Similar principles apply to the transition of care or transition readiness for children with disorders cared for by a pediatric neurogastroenterologist as they do for children with other complex, chronic conditions, such as IBD, solid organ transplant or cystic fibrosis (10., 11.). It is important for children and young adolescents to obtain age-appropriate skills and knowledge regarding their disease and disease management. Fostering a thoughtful process, involving the patient and caregivers at a developmentally appropriate level, recognizing that a multistep transition is required (rather than an abrupt transfer of care), and direct communication between pediatric and adult specialists are consistent tenets. However, children with congenital or acquired disorders of NGM including HD, esophageal achalasia, and pediatric intestinal pseudo-obstruction will benefit from specific transition focus depending on the condition. Identification of an appropriate adult specialist is frequently a challenging shared responsibility between patients, families, and pediatric specialists. Barriers may include geography, finances, insurance coverage, and finding a specialist with sufficient knowledge of or willingness to manage a specific condition. It is also important to note that diagnoses may change when transitioning from pediatric to adult criteria for NGM disorders causing further stress for the patient and family. Pediatric and adult specialists benefit from basic understanding of differences in training and practice between their colleagues, but it remains a mutual responsibility to utilize each other's expertise, sometimes through frequent written or verbal communication, to ensure a smooth transition. Patient and family self-advocacy also benefits from ongoing education and communication from their pediatric specialist during the transition process. Patients and families should be encouraged to share their concerns and fears before transition so that these can be acknowledged, and wherever appropriate be addressed directly. Once an adult NGM specialist is identified, providing appropriate documentation is vital which may include a summary letter, clinical notes, and reports from diagnostic testing including manometry, radiography, and endoscopy. Following an initial visit with the adult specialist, discussing with the patient and family their experience can help ensure they continue to feel supported in the transition and potentially identify additional needs.
CONCLUSIONS
In the context of providing relevant training to the trainees with specific career interest within the realm of NGM, the NASPGHAN-ANMS task force created a pediatric, tiered and EPA-based NGM curriculum in line with specific expectations and goals of training as delineated through already established milestones and EPAs. This document should serve as a resource to encourage pursuit of a career in NGM and provide a framework towards uniform training expectations at 3 hierarchical tiers in North America. As further advances in the field of pediatric NGM are made and training paradigms change, regular updates of the NGM curriculum will be necessary; societies will need to invest in the process of revision and renewal of the concepts described in this document (EPA NGM Supplemental Digital Content Document, http://links.lww.com/MPG/C10).