Multiparametric MRI as a Noninvasive Monitoring Tool for Children With Autoimmune Hepatitis
This study was funded by the Eureka Eurostars 2 Grant (E!10124), Clinical trial number: NCT03198104 (https://clinicaltrials.gov/ct2/show/NCT03198104).
The authors report no conflicts of interest.
ABSTRACT
Objectives:
Autoimmune hepatitis (AIH) is a progressive liver disease managed with corticosteroids and immunosuppression and monitored using a combination of liver biochemistry and histology. However, liver biopsy is invasive with risk of pain and bleeding. The aim of the present study was to investigate the utility of noninvasive imaging with multiparametric magnetic resonance imaging (MRI) (mpMRI) to provide clinically useful information on the presence and extent of hepatic inflammation, potentially guiding immunosuppression.
Methods:
Eighty-one participants (aged 6–18), 21 healthy and 60 AIH patients, underwent multiparametric MRI to measure fibro-inflammation with iron-corrected T1 (cT1) at the Children's Memorial Health Institute in Warsaw alongside other clinical blood tests and liver biopsy at recruitment and after an average of 16-month follow-up (range 9–22 months). Correlation analyses were used to investigate the associations between cT1 with blood serum markers and histological scores.
Results:
At recruitment, patients with AIH had a higher cT1 value than healthy controls (P < 0.01). cT1 correlated significantly with key histopathological features of disease. Treatment naïve AIH patients showed evidence of inflammation and heterogeneity across the liver compared to healthy controls.
At follow-up, cT1 showed utility in monitoring disease regression as most patients showed significantly reduced fibro-inflammation with treatment (P < 0.0001) over the observational period. Six patients had histological fibrosis and clear fibro-inflammation on MR despite biochemical remission (normalized aspartate aminotransferase (AST), alanine aminotransferase (ALT), and immunoglobulin G [IgG]).
Conclusions:
Multiparametric MRI can measure disease burden in pediatric AIH and can show changes over time in response to therapy. Active disease can be seen even in biochemical remission in children.
What Is Known
- In pediatric autoimmune hepatitis patients, a liver biopsy is recommended before reducing or withdrawal treatment.
- Noninvasive techniques can aid monitoring of autoimmune liver disease.
What Is New
- Iron-corrected T1 can provide detailed liver fibro-inflammation assessment in autoimmune hepatitis.
- Iron-corrected T1 can identify those patients who have active disease despite having normal biochemistry.
- Iron-corrected T1 correlates with blood markers of disease activity and severity.
Autoimmune hepatitis (AIH) is a chronic autoimmune liver disease with a fluctuating course, which, if not managed effectively, can result in advanced liver disease with all its complications (1.). Patients with AIH may experience acute flares throughout life and require treatment with corticosteroids [which are associated with several complications (2.)] and immunosuppressant therapy. Liver biopsy remains the major monitoring parameter in children (3.), but lifelong monitoring using transient elastography and a combination of blood tests (including immunoglobulin G [IgG], antibodies, etc.) (4.) is also common. Identifying disease remission, indicated by normalization of aminotransferases and IgG, absence of symptoms, and normalization or minimal inflammatory activity on liver biopsy, is important because of treatment implications. However, despite having normal biochemical markers, a proportion of patients may display inflammation and increased fibrosis on liver histology (5., 4.), with up to 80% of patients experiencing a disease flare (6.). However, liver biopsy has considerable interobserver and sampling variability and heterogeneity and carries a risk of well-recognized complications such as intra-abdominal bleeding, pain, and death among several others (7.-10.). Therefore, current guidelines recommend using biopsy only at diagnosis, nonresponsiveness to treatment, and for consideration of removal from immunosuppressive therapy (3., 11.).
There is, therefore, a need for robust, objective, reproducible noninvasive biomarkers of liver tissue characterization that can be used to assist with diagnosis, monitoring of therapeutic response, remission, and prediction of those at risk of flares and progressive liver disease. Recent guidelines (11.) have included recommendations concerning the use of noninvasive techniques. Serum-based biomarker panels were not recommended as their true utility in AIH is currently unknown. Vibration-controlled transient elastography has a high coefficient of variation and was recommended after at least 6 months of treatment due to its susceptibility to the effects of hepatic inflammation (12., 11., 13.).
Multiparametric MRI (mpMRI) quantitative biomarkers have been shown to successfully affect clinical practice in several medical fields, including prostate breast cancer, and cardiology (14.-16.). mpMRI has also advanced liver disease clinical research and shown utility in the clinical assessment of liver disease (17.-20.). Iron corrected T1 (cT1) is an objective composite biomarker of fibrosis and inflammation (fibro-inflammation) with low interobserver variability and high repeatability over time and across scanners (21., 13.), as well as having very low coefficient of variation in monitoring liver disease at multiple timepoints (13.). Studies have shown that cT1 correlates with histological measures of fibrosis, portal and lobular inflammation, and ballooning, alongside being able to predict clinical outcomes and being cost-effective in the management of liver disease (18., 22.-24.). In addition to this, the mpMRI cT1 biomarker has been shown to indicate the presence of radiological portal hypertension in chronic progressive pediatric autoimmune liver diseases with high sensitivity and specificity (25.).
The aim of the present study was to investigate the utility of mpMRI in a pediatric population to discriminate between healthy controls and those with AIH. In addition, one of our objectives was to identify whether cT1 could help determine responsiveness to treatment in AIH pediatric patients.
METHODS
The present prospective observational study was sponsored by the Eureka Eurostars 2 Grant (E!10124) and received ethical approval (11/KBE/2016) in Poland. The study was entitled Kids4Life: Assessing Kids for Liver Inflammation and Fibrosis using noninvasive MRI and registered as a clinical trial (NCT03198104).
We enrolled 81 participants into the study; 21 healthy (aged 11 ± 3.7 years) and 60 biopsy confirmed AIH patients (aged 13.4 ± 3.7). Children aged 6–18 with biopsy confirmed or suspected AIH due to have a liver biopsy as part of clinical care were invited to have a research MRI scan (treatment naïve patients were those not on treatment before recruitment, N = 16). The diagnosis was based on liver histology with analysis of typical clinical, biochemical, and serological features after exclusion of other causes of liver injury, such as viral hepatitis, Wilson disease, nonalcoholic steatohepatitis, and drug-induced liver disease (3.). Exclusion criteria were claustrophobia and the inability to lie flat. A separate group of age-matched healthy volunteer children were also recruited to be scanned as part of the present research study. Healthy volunteers were defined as those with no active medical condition requiring treatment, including any liver diseases, diabetes, hypertension, autoimmune disorders, and any chronic gastrointestinal disorder. In the present study, biochemical remission was defined as aspartate aminotransferase (AST) <40 IU/L, alanine aminotransferase (ALT) <40 IU/L, and IgG <16.0 g/L.
After attending their first clinical visit, patients were treated according to the normal clinical pathway at the Children's Memorial Health Institute in Warsaw (IPCZD). MRI scans (healthy and AIH patients) were performed at the IPCZD. All scans were performed on 1.5T Siemens Avanto systems (Siemens Healthineers, Germany) with the standard LiverMultiScan (Perspectum, Oxford, UK) acquisition protocol described in detail by Bachtiar et al (21.). The individual components of the mpMRI acquisition protocol consisted of noncontrast T1, T2*, and proton density fat fraction (PDFF) mapping (21.). For T2* and PDFF maps, three 15 mm diameter circular regions of interest were placed on 4 slices on the transverse maps to cover a representative sample of the liver parenchyma. cT1 maps of the liver were delineated into whole liver segmentation maps using a semiautomatic method. Owing to the spatial nature of the cT1 maps of the liver, they also provide information on the heterogeneity of liver tissue defined through the interquartile range (IQR) of cT1 .
Histopathology Assessment
Percutaneous biopsies were performed under ultrasound guidance using a Menghini needle. The sample was assessed histopathologically for steatosis (and parenchymal fat percentage), lobular and portal inflammation, fibrosis (26.), and necrosis (27., 28.) by 2 experienced liver pathologists. Steatosis was assessed on a 4-tier scale (0–3), inflammation on a 3-tier scale (0–2), fibrosis on a 5-tier scale (0–4), necrosis on a 3-tier scale (0–2), hepatocyte ballooning on a 3-tier scale (0–2), cholestasis on a 4-tier scale (0–3), diffuse postnecrotic scarring on a 2-tier scale (0–1), and collagen proportion (%).
Data Analysis
Statistical analyses were performed using R version 3.5.3. Pearson correlation (r) was used to investigate all continuous variables that followed a normal distribution, whereas Spearman correlation (R) was used for continuous variables that did not follow a normal distribution. Owing to the measurement values being approximately lognormally distributed with a skew around 0, blood biomarker values were log transformed to make them approximately normally distributed, as well as to enable clearer visualization of the changes with disease severity to better understand the associations between these blood serum markers and cT1. Finally, correlation analyses to investigate the association between cT1 and histology scores were also performed. For all analyses, values of P < 0.05 were considered statistically significant.
RESULTS
Patient Demographics
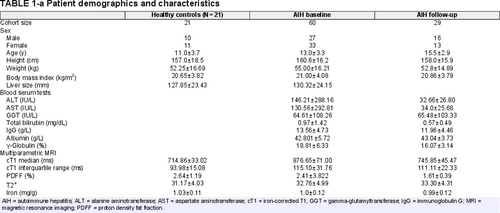
A total of 110 scans were performed (21 in healthy cohort, 60 at baseline, and 29 at follow-up in the present study as shown in Table 1). All baseline scans were performed at the start of the study, with a second scan for AIH patients performed after 16.2 months (between 9 and 22 months) of treatment. No patients developed de novo clinical cirrhosis or portal hypertension during the observational period. Moreover, independent t tests at baseline showed no significant histological differences in fibrosis (P = 0.88), necrosis (P = 0.58), steatosis (P = 0.17), portal inflammation (P = 0.20), and lobular inflammation (P = 0.33) between the whole group and the subgroup who had a second biopsy.
All of the 60 AIH patients recruited at baseline underwent a liver biopsy, with 2 having a biopsy, which was not good enough for histological examination. Forty-four patients had biopsy-proven AIH diagnosed before or at recruitment, whereas 16 patients were treatment naïve at baseline. At follow-up, patients returned for a repeat mpMRI scan and those who presented with flares or required a change in their treatment were scheduled to receive a second biopsy (Fig. 1). During the observation period, N = 5 were on azathioprine treatment, N = 7 were only on steroid (prednisone) treatment, N = 1 was on steroid and cylcosporin A (CsA), N = 14 were on a combination of azathioprine and prednisone treatment, N = 1 was on azathioprine, prednisone and CsA, and N = 1 was not on any treatment (from 5 months before follow-up). Of the N = 22 with clinical indication for repeated biopsy and agreed to undergo the procedure, N = 3 was on azathioprine treatment, N = 6 were only on steroid (prednisone) treatment, N = 12 were on a combination of azathioprine and prednisone treatment, and N = 1 on azathioprine, prednisone, and CsA (Fig. 1).
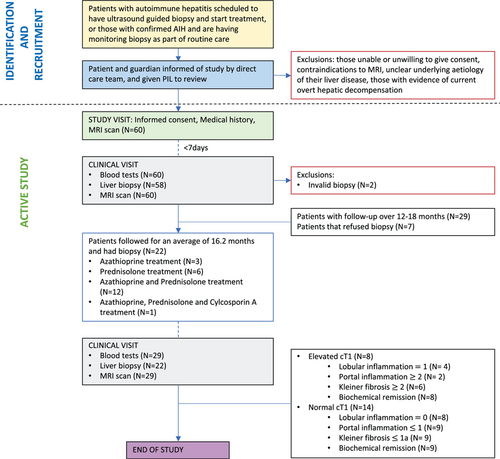
Study procedure and patient pathway throughout the clinical trial. AIH = autoimmune hepatitis; MRI = magnetic resonance imaging; PIL = patient information leaflet.
Baseline
Iron-Corrected T1 Versus Blood Biomarkers
Biochemical correlations between cT1 and ALT (R = 0.47, P = 0.0005), g-globulin (R = 0.50, P = 0.0017), AST (0.41, P = 0.0057), gamma-glutamyltransferase (R = 0.37, P = 0.014), and IgG (R = 0.34, P = 0.026) within the AIH group at baseline were statistically significant but moderate.
Iron-Corrected T1 Versus Histology
Associations between cT1 and histology showed significant positive correlations between cT1 and Kleiner Brunt fibrosis (R = 0.38, P = 0.001); portal and lobular inflammation (R = 0.35, P = 0.008, R = 0.32, P = 0.016, respectively); and necrosis (R = 0.43, P = 0.002).
Iron-Corrected T1 to Discriminate Between Healthy and AIH at Diagnosis
At recruitment patients with AIH had a higher cT1 value than healthy controls (P < 0.01). MRI can visualize the whole liver and measure its heterogeneity. In this population with low liver fat (median 3.23%), patents with AIH had heterogeneity in their fibroinflammatory burden, which resulted in them having higher cT1 and IQR values (median cT1 of 876 ms, median IQR of 115 ms) than healthy controls (median cT1 of 714 ms, median IQR of 93 ms; Fig. 2). In this cohort, complete discrimination was obtained using cT1 and IQR as a compound biomarker with a cT1 cutoff of 775 ms and an IQR of 125 ms.
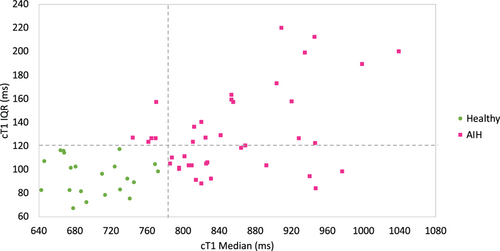
Scatterplot showing the distribution of cT1 medians and IQRs in healthy controls (N = 21) and AIH patients (N = 60). Healthy controls have both low cT1 medians and IQRs (bottom left quadrant), whereas AIH patients can have any (or both) of the two elevated. AIH= autoimmune hepatitis; cT1 = iron-corrected T1; IQR = interquartile range.
Iron-Corrected T1 to Monitor Changes in Fibro-Inflammation in Patients on Treatment at Follow-Up
Results showed average cT1 values of healthy participants (median cT1: 714 ms, IQR: 93 ms) were significantly lower (P = 0.001) than at baseline (median cT1: 876 ms, IQR: 115 ms). After treatment, there was a significant decrease (P = 0.0002) in cT1 values (from a groupwise mean of 876 to 745 ms). Moreover, due to this decrease in cT1 following treatment, the cT1 values for AIH patients were no longer significantly different from the healthy volunteer values (P = 0.36; Fig. 3). In addition, only portal inflammation decreased significantly (P = 0.01) over the observational period (this is commonly observed in the well-treated pediatric groups). Owing to the low histological scores of ballooning, fibrosis, necrosis, steatosis, and lobular inflammation (mainly 0 or 1), these did not change significantly between the two timepoints (P > 0.05).
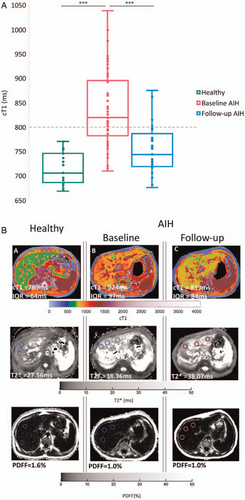
(A) cT1 median values of healthy cohort and those with AIH at baseline and follow-up. t tests showed that AIH baseline cT1 values were significantly higher than healthy (P < 0.01) and at follow-up (P < 0.001). 31% (N = 9) of patients had elevated cT1 values consistent with the presence of active fibroinflammatory disease after an average of 16.2 months. (B) Example cT1, T2*, and PDFF maps from (A) a healthy control and an AIH patient (B–C) baseline (B) and (C) follow-up. In the images, cooler colors represent areas with lower cT1 values, whereas warmer colors represent areas with higher cT1 values, which have been shown to correlate with fibro-inflammation. AIH = autoimmune hepatitis; cT1 = iron-corrected T1; PDFF= proton density fat fraction.
At follow-up, 9 of 29 patients (31%) had elevated cT1 values compared to both the healthy group (P < 0.0001) and the other AIH patients (P < 0.0001) consistent with the presence of active fibroinflammatory disease. Moreover, of the 9 patients with elevated cT1, only 1 (cT1 = 879 ms) was not in biochemical remission (AST/ALT > upper limit of normal) and had ALT = 74 IU/L and AST = 46 IU/L. This patient did not undergo a second biopsy at follow-up. In addition, of the 8 remaining patients with elevated cT1 and resolved biochemistry, N = 2 had resolved fibrosis and inflammation (on biopsy), N = 6 had Kleiner fibrosis scores ≥2, N = 4 had lobular inflammation of 1, whereas N = 2 had portal inflammation ≥2. Moreover, of the remaining 13 patients who had a biopsy at follow-up with cT1 <800 ms, N = 9 (70%) had Kleiner fibrosis ≤1a, portal inflammation ≤1, and portal inflammation ≤1. Therefore, cT1 had a sensitivity of 60%, specificity of 82%, positive predicting value of 0.75, and negative predicting value of 0.69 to identify those with ongoing histological activity.
Comparing all patients scanned at baseline and after standard of care treatment, the cT1 IQR decreased from 115 to 111 ms, indicating a decrease in the heterogeneity across the patients’ livers. Moreover, in the patients who received a second biopsy after treatment, cT1 changed significantly (P = 0.04), alongside ALT (P = 0.01), AST (P = 0.03), g-globulin (P = 0.02), IgG (P = 0.02), and portal inflammation (P = 0.01).
DISCUSSION
AIH, although relatively rare, is associated with ongoing morbidity and mortality. Clinical practice and treatment guidelines frequently diverge and challenges in agreeing standards of care result in reluctance on the part of clinicians and patients to use liver biopsy and an increasing recognition of treatment burden for patients. We sought to explore the clinical utility of using noninvasive, noncontrast MRI imaging to monitor liver health in a pediatric AIH cohort. cT1 significantly correlated with blood biomarkers and key aspects of histology at baseline. Additionally, including a measure of disease heterogeneity enhanced discrimination between healthy individuals and those with AIH.
Biochemical markers are used clinically to confirm hepatic events, especially as the degree of blood marker elevation is indicative of disease severity. However, despite their use in monitoring patient status (29.-31.), blood markers can be insufficient to assess the absence of disease activity as most patients with continued disease activity can present with normal biochemistry (32.). In the present study, of the 9 patients in biochemical remission but an elevated cT1, 8 underwent concomitant biopsy and 6 had findings on histology consistent with active disease despite having normal biochemistry.
As liver biopsy remains the gold standard (33., 34.), it is important that any additional biomarkers proposed for aiding diagnosis or monitoring of AIH should correlate with key histological characteristics of disease. The positive association between cT1 and key histological characteristics further supports the utility of cT1 as a quantitative biomarker. These results are in keeping with those observed in liver diseases with viral etiology or in steatohepatitis (35., 36.) where cT1 correlated with hepatic fat and fibro-inflammation and was a strong predictor of clinical outcomes (37., 38., 18.). Moreover, although cT1 had a moderately low sensitivity (60%) to identify those with histological activity, it had a high specificity (82%), moderate-to-high positive predicting value (0.75), and a moderate negative predicting value (69%), which show that it has the potential to be used as an adjunct marker, alongside other diagnostic tools, to rule in those with histological activity.
During the observation period, changes in cT1 associated with the effects of therapeutic response were observed, suggesting that it can be a useful additional biomarker in the monitoring of liver health following intervention in pediatric AIH. Moreover, in the subgroup of patients, who had elevated cT1 values, normal biochemistry, and liver biopsy at follow-up, 27% (6/22) of them had histologically active disease. Thus, in this subgroup, cT1 can be used to identify those patients who may benefit from a review of their treatment and thus help to decrease risk of disease progression and future flare events (31.). This highlights the potential utility of cT1 as a biomarker to monitor liver health in pediatric AIH patients.
By concurrently assessing the heterogeneous nature of the disease with cT1 IQR across the liver, this allowed for complete discrimination of the healthy cohort from the AIH cohort. Although requiring validation in an independent data set, this highlights the utility of mpMRI to provide additional detail to support diagnosis and monitoring of AIH. Visualization of disease heterogeneity also has the potential to guide invasive liver biopsy, where justified, to regions of active disease.
Although the results described above are promising, there are some limitations. A small number of patients were followed for an average of 16.2 months; therefore follow-up multicentre studies may be required to further validate the results in a wider population. In the present study, moderate correlations with coefficient were observed between cT1 and histological scoring. This was likely due to the exacerbated impact of sampling error with biopsy due to disease heterogeneity combined with the uneven distribution of patients across histological stages. Although there was a general decrease in the histology scores of fibrosis, necrosis, and inflammation in the patients who received a repeat biopsy, in this cohort only the portal inflammation scores showed a significant decrease over the observation period. This lack of significant change in the other histological scores could be attributed to the short study period, the sampling error associated with the biopsy procedure, and the size of the subcohort with repeat biopsies. Therefore, to further understand the associations between noninvasive biomarkers and disease progression/regression, larger longitudinal studies that explicitly consider sampling error and have a longer follow-up period may be considered. Furthermore, as cT1 is a noninvasive composite biomarker of fibrosis and inflammation (fibro-inflammation), it is not currently able to measure one independent of the other. Thus, although high cT1 does not imply the existence of both fibrosis and inflammation simultaneously, future work is ongoing to improve the biomarker so that it can distinguish between fibrosis and inflammation. Although the specificity and positive predictive values were good for a pilot study, the low sensitivity and negative predictive values highlight the need to further assess the performance of the cT1 in a bigger cohort in order to validate its utility within a generalized clinical setting.
To summarize, this is the first report showing that quantitative mpMRI can be used to noninvasively characterize underlying disease activity associated with AIH in pediatrics. The results show positive associations between cT1 and histological characteristics of the disease (fibrosis, portal and lobular inflammation, necrosis). These findings suggest that cT1 could be used as an adjunct biomarker to measure disease activity and assess liver health. Furthermore, the significant drop in cT1 following treatment highlighted its potential utility in treatment monitoring. The present pilot study identifies mpMRI as a potentially disruptive technology and justifies future prospective clinical trials to fully explore its utility. With further validation, this technology has the potential to provide useful information to aid in clinical decision-making, such as improved identification of patients with ongoing disease burden.