Reduced Plasmacytoid Dendritic Cell Output Is Associated With High Risk in Low-grade Myelodysplastic Syndrome
Supplemental digital content is available for this article.
Myelodysplastic syndromes (MDSs) are a group of clonal hematopoietic stem cell (HSC)-derived neoplasms characterized by ineffective hematopoiesis, morphologic dysplasia, genetic abnormalities, and risk of progression to acute myeloid leukemia (AML). The WHO classification recognizes several diagnostic subtypes,1, 2 and risk stratification most often utilizes the Revised International Prognostic Scoring System (IPSS-R).3, 4 Flow cytometry (FC) is a useful adjunct testing modality in the evaluation of MDS, but alone it is insufficient for diagnosis of MDS.1, 5 A combination of clinical risk scores and morphologic subtype are used for clinical decision-making in the treatment of MDS. However, identifying lower-risk MDS patients at risk of progression and thus needing aggressive treatment at diagnosis remains a clinically unmet need.
Plasmacytoid dendritic cells (pDCs) are major type I interferon producing dendritic cells that mediate between the innate and adaptive immune systems.6, 7 Studies suggest that pDCs proportions are altered in MDS.8-10 In AML, loss of pDC differentiation correlates with inferior outcome.11 Here, we determine pDC proportions in subgroups of MDS, utility of pDCs in risk stratification, and the differentiation potential of pDCs in MDS.
This study was approved by an Institutional Review Board. We assessed 197 consecutive adult patients with MDS and bone marrow (BM) analysis by FC performed at our hospital (Suppl. Table 1). As a control, we evaluated staging BMs in 10 chemotherapy naive adult patients with stage I or II (by Ann Arbor staging system) mature B-cell lymphomas. Controls had no cytopenias, no BM involvement by lymphoma, and no evidence of myeloid neoplasia.12
Plasmacytoid dendritic cells were quantified on diagnostic BM aspirates as a percent of total WBC by FC based on low side scatter, moderate CD45, bright CD123 and HLA-DR expression (Suppl. Digital Methods and Figure 1). In the control group, pDCs had a median proportion of 0.26% (IQR 0.24% to 0.38%), consistent with prior estimations of pDC proportions.13, 14 Compared to control groups, pDCs were not significantly different in MDS with del5q (median 0.39%, IQR 0.18%–0.56%) or MDS-SLD (0.20%, 0.15%–0.36%) but were significantly lower in MDS-MLD (0.16%, 0.06%–0.32%), MDS-EB1 (0.07%, 0.03%–0.18%), and MDS-EB2 (0.07%, 0.03%–0.19%) (Figure 1A). Defining low-grade MDS (LG-MDS) as MDS with isolated del5q, MDS-SLD, and MDS-MLD, and high-grade MDS (HG-MDS) as MDS-EB1 and 2, LG-MDS (0.18%, 0.07%–0.38%) had significantly higher pDCs than HG-MDS (0.07%, 0.03%–0.19%) (P < 0.0001). Decreasing pDC proportion was significantly associated with worsening IPSS-R risk categories in 163 patients with enough data available to calculate IPSS-R category (Kruskal–Wallis test, P < 0.0001, Figure 1). Combined high- or very high-risk patients (0.07%, 0.04%–0.16%) also showed decreased median pDC compared to those with intermediate risk or better (0.22%, 0.07%–0.34%) (P < 0.0001) (Figure 1B). Higher cytogenetic risk was also associated with lower pDCs (Suppl. Figure 2).
As some patients received disease modifying therapy prior to presentation, we compared pDCs in untreated patients versus those who received any therapy before presentation at our hospital. Disease-modifying therapy was not associated with differences in pDC proportions (Suppl. Figure 3A,B). Since therapy-related myeloid neoplasia (t-MN) is a separate, prognostically relevant diagnostic category, we also assessed pDCs in patients that qualified for diagnosis of t-MN compared to de novo MDS and found no differences (0.13% [IQR 0.04%–0.26%] versus 0.099% [IQR 0.043%–0.25%], P = 0.45, Suppl. Figure 3C). This was similar in LG-MDS subgroups (P = 0.8213) as well as in intermediate-risk or better IPSS-R subgroups (P = 0.1469). Thus, neither t-MN nor disease modifying therapy for MDS appear to affect pDC proportions.
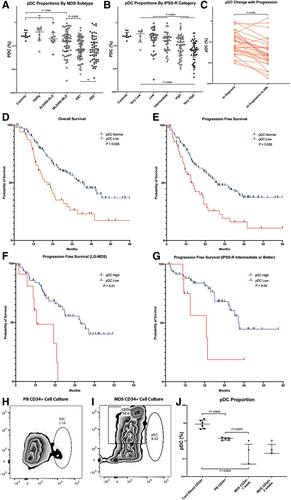
pDC proportion comparisons, survival analysis, and pDC culture experiment results. (A) pDC proportions in different WHO subclassifications of MDS. (B) pDC proportions in different IPSS-R risk groups. (C) Matched comparison of pDC proportions at diagnosis compared to time of progression to AML. (D) OS differences between pDC normal (upper three quartiles of pDC proportions) and pDC low (bottom quartile of pDC proportion) groups demonstrate an HR of 2.10 (95% CI: 1.37–3.21; P = 0.026). (E) PFS differences between pDC normal and pDC low groups. Progression events were defined by progression from low- to high-grade MDS, AML or death. PFS curves show an HR of 1.92 (95% CI: 1.28–2.88; P = 0.026). (F) PFS curves between pDC normal and pDC low groups within patients with only low-grade MDS show inferior PFS in patients with low pDC, with HR 2.04 (95% CI: 1.27–3.27, P = 0.01). (G) PFS was also lower in the pDC low groups within patients with IPSS-R risk category of intermediate or better, demonstrating HR 4.78 (95% CI: 1.14–20.1, P = 0.04). (H) Cell culture from normal peripheral blood CD34+ progenitor cells after 2 weeks demonstrates pDC differentiation (box). (I) Cell culture from CD34+ progenitor cells from an MDS patient shows loss of differentiation of pDCs. (J) pDC proportions after 2 weeks of culture from cord blood CD34+ progenitor cells compared to pDC proportions after 1 and 2 weeks of culture from CD34+ progenitor cells from an MDS patient. AML = acute myeloid leukemia; CI = confidence interval; HR = hazard ratio; IPSS-R = revised international prognostic scoring system; MDS = myelodysplastic syndrome; OS = overall survival; pDC = plasmacytoid dendritic cells; PFS = progression free survival.
Patients were monitored for progression for a median follow up time of 18.8 months (range 0.47–62.2 mo). Thirty of 197 patients progressed to AML and had FC data at both the time of diagnosis and at progression to AML. Lower pDCs were seen at time of progression to AML compared to that at the time of MDS diagnosis (median 0.025%, IQR 0.013%–0.064%, versus median 0.089%, IQR 0.039%–0.22%, P = 0.0005, Wilcoxon matched pairs test, Figure 1C).
We assessed outcomes in groups stratified by pDC proportions, evaluating differences in overall survival (OS) and progression-free survival (PFS). Progression events were defined progression to AML, progression from LG-MDS to HG-MDS, or death. When pDC was considered a continuous variable the associated hazard ratio (HR) for OS was 0.80 (95% confidence interval [CI]: 0.67–0.94; P value: 0.007) and for PFS was 0.81 (95% CI: 0.69–0.95; P value: 0.009). To facilitate the utility of pDC in a clinical setting, a maximal rank test was used to identify an optimal dichotomization. For OS, the maximal pDC split was 0.038% and PFS the split was at 0.04%. The HR for this split was 2.10 (95% CI: 1.37–3.21; P = 0.026) for OS and 1.92 (95% CI: 1.28–2.88; P = 0.026) for PFS (Figure 1D and E). As 0.04% was the lower quartile cutoff for pDCs in our cohort, we set a cutoff of <0.04% pDC for further survival analyses.
In univariate analysis, variables other than pDC proportion significantly associated with OS and PFS included well-known factors such as age, t-MN, cytogenetic risk category, and IPSS-R category (Table 1). Multivariate analysis using Cox proportional hazards regression showed that age, t-MN, and IPSS-R risk categories were associated with a significant effect on OS, and low pDC proportion trended towards significance for OS (HR 1.54, 95% CI 0.92–2.58, P = 0.099). Only age and IPSS-R risk category were significantly associated with PFS by multivariate analysis.
| Variable | HR (95% CI) | P value |
|---|---|---|
| Overall survival (univariable) | ||
| Age | 1.030 (1.011–1.049) | 0.002 |
| Sex (male) | 0.743 (0.493–1.120) | 0.155 |
| Grade (high) | 1.169 (0.765–1.788) | 0.470 |
| t-MN | 1.619 (1.067–2.454) | 0.023 |
| pDC low (<0.04%) | 2.095 (1.370–3.205) | <0.001 |
| CG category | ||
| Very good + Good | — | — |
| Intermediate | 1.299 (0.672–2.516) | 0.437 |
| Poor | 1.795 (0.854–3.772) | 0.123 |
| Very poor | 3.734 (2.155–6.470) | <0.001 |
| IPSS-R category | ||
| Very low + low | — | — |
| Intermediate | 1.126 (0.478–2.621) | 0.786 |
| High | 1.788 (0.871–3.673) | 0.113 |
| Very high | 3.992 (2.003–7.957) | <0.001 |
| Overall survival (multivariable) | ||
| Age | 1.032 (1.010–1.054) | 0.004 |
| t-MN | 1.773 (1.103–2.850) | 0.018 |
| pDC low (<0.04%) | 1.541 (0.922–2.576) | 0.099 |
| IPSS-R category | ||
| Very low + low | — | — |
| Intermediate | 1.089 (0.460–2.576) | 0.846 |
| High | 2.057 (0.964–4.391) | 0.062 |
| Very high | 4.123 (2.025–8.406) | <0.001 |
| Progression-free survival (univariable) | ||
| Age | 1.020 (1.003–1.038) | 0.019 |
| Sex (male) | 0.872 (0.587–1.295) | 0.497 |
| Grade (high) | 1.368 (0.914–2.048) | 0.127 |
| t-MN | 1.308 (0.873–1.959) | 0.193 |
| pDC low (<0.04%) | 1.916 (1.274–2.883) | 0.002 |
| CG category | ||
| Very good + good | — | — |
| Intermediate | 1.405 (0.768–2.569) | 0.270 |
| Poor | 1.656 (0.821–3.343) | 0.159 |
| Very poor | 2.897 (1.711–4.906) | <0.001 |
| IPSS-R category | ||
| Very low + low | — | — |
| Intermediate | 1.210 (0.552–2.653) | 0.634 |
| High | 1.733 (0.885–3.393) | 0.109 |
| Very high | 3.814 (1.997–7.284) | <0.001 |
| Progression-free survival (multivariable) | ||
| Age | 1.025 (1.004–1.045) | 0.017 |
| t-MN | 1.478 (0.935–2.335) | 0.094 |
| pDC low (<0.04%) | 1.475 (0.897–2.426) | 0.125 |
| IPSS-R category | ||
| Very low + low | — | — |
| Intermediate | 1.167 (0.530–2.569) | 0.702 |
| High | 1.882 (0.930–3.809) | 0.079 |
| Very high | 3.825 (1.976–7.402) | <0.001 |
- CG = cytogenetics; CI = confidence interval; HR = hazard ratio; IPSS-R = Revised international prognostic scoring system; pDC = plasmacytoid dendritic cells; t-MN = therapy-related myeloid neoplasia.
We also evaluated outcomes in lower-risk subgroups. By WHO classification, there were 76 patients with LG-MDS. Using the previous cutoff of 0.04%, 11 patients were considered low pDC in the LG-MDS subgroup; survival analysis showed significantly worse PFS in these patients compared to those with higher pDCs (HR 2.04, 95% CI: 1.27–3.27, P = 0.01, Figure 1E). Within the LG-MDS subgroup, there was no significant difference in t-MN proportions between the low pDC versus higher pDC group (30% versus 39%, P = 0.7328), and t-MN status was not associated with significant differences in OS (HR 1.72, 95% CI: 0.83–3.57, P = 0.15) or PFS (HR 1.15, 95% CI: 0.60–2.22, P = 0.68).
Within IPSS-R risk categories, there were 69 patients in IPSS-R categories of intermediate, low, and very low risk. Only eight had low pDC but this was associated with inferior PFS compared to patients with higher pDCs (HR 4.78, 95% CI: 1.14–20.1, P = 0.04; Figure 1G). Interestingly, within this intermediate risk or better IPSS-R subgroup, there was a significantly higher proportion of patients with t-MN in patients with low pDCs compared to those with higher pDCs (62.5% versus 23%, P = 0.032), though t-MN status in this subgroup was not associated with differences in OS (HR 1.04, 95% CI: 0.38–2.83, P = 0.94) or PFS (HR 1.573, 95% CI: 0.68–3.64, P = 0.29).
When assessing the clonal relationships between pDCs and myeloid blasts, high-purity (>99%) sorted pDCs showed a mixture of neoplastic and normal cells by fluorescence in situ hybridization (FISH) (3%–100% of cells), whereas myeloid blasts were mostly neoplastic clones (84%–100%) (Suppl. Table 2). This suggested a differentiation blockage from myeloid blasts to pDCs consistent with previously studies showing dendritic cell differentiation defects in MDS.15 In contrast, a higher proportion of sorted myelomonocytic cells carried the shared cytogenetic abnormalities suggesting that differentiation defects vary between different lineages. To assess ex vivo pDC differentiation and growth in MDS, we used sorted CD34+ cells to culture pDCs from 5 MDS patients, 6 umbilical cord samples, and 5 healthy donors.16 Cord blood CD34+ cells showed 10%–20% pDCs after 2 weeks of culture and healthy donor PB CD34+ cells showed 1%–2%, whereas MDS patients showed 0%–1% pDCs (Figure 1H–J), confirming limited pDC differentiation from leukemic blasts in MDS at least in ex vivo culture.
Our findings demonstrate that low pDC proportion is associated with high risks in MDS, including high grade WHO subtypes, poor CG risk, and high-risk IPSS-R categories. We also find an association between pDCs and survival; pDC enumeration may complement MDS clinical risk stratification, especially in otherwise low-risk MDS, though multivariate analysis suggests that IPSS-R is still the strongest predictor of outcomes. While meeting criteria for t-MN does not appear to affect pDC proportions, survival differences with differing pDC levels might associate with history of chemoradiation. Unlike PFS, OS was not significantly different in these lower-risk groups, which may reflect that most high-risk MDS patients at our institution receive aggressive treatment.
Our data suggest that pDCs may be a marker of a functional defect in the leukemic stem cell population in MDS. While still poorly understood, our findings shed new light into the role of pDCs in MDS. However, it is notable that this is a retrospective, single-center study in a large cancer center and the cohort is somewhat biased toward therapy-related MDS and high-risk patients, which could impact our analysis of low-risk MDS patients. Nonetheless, we find a strong association between pDC proportion and IPSS-R risk category. More importantly, pDC proportion may provide additional risk stratification in otherwise low-grade and/or good-to-intermediate IPSS-R risk group of MDS, to identify patients at the highest risk of clinical progression and adverse outcome.
DISCLOSURES
WX has received research support from Stemline Therapeutics. All the other authors have no conflicts of interest to disclose.
SOURCES OF FUNDING
This study was funded by the Center for Hematologic Malignancies at MSKCC and in part through the NIH/NCI Cancer Center Support Grant P30 CA008748. WX was supported by a grant from Alex's Lemonade Stand Foundation and the Runx1 Research Program.




