S122: SAFETY AND EFFICACY OF CRIZANLIZUMAB IN ADOLESCENTS WITH SICKLE CELL DISEASE (SCD): INITIAL DATA FROM THE PHASE II, MULTICENTER, OPEN-LABEL SOLACE-KIDS TRIAL
Background: Vaso-occlusive crises (VOCs) are the hallmark of SCD. P-selectin, a cell adhesion molecule, plays a key role in the multicellular interactions leading to VOCs. In the SUSTAIN trial, crizanlizumab 5 mg/kg, a first-in-class humanized monoclonal antibody that blocks P-selectin, significantly reduced the annualized rate of VOCs versus placebo and had a favorable safety profile in adults with SCD.
Aims: To describe the initial safety and efficacy results for patients with SCD aged 12 to <18 years treated with crizanlizumab 5 mg/kg in the SOLACE-kids trial (ClinicalTrials.gov: NCT03474965; EudraCT: 2017-001747-12).
Methods: SOLACE-kids is an ongoing Phase II study to establish and confirm appropriate dosing (Part A) and evaluate long-term safety and efficacy (Part B) of the confirmed dose of crizanlizumab, with or without hydroxyurea, in pediatric patients with SCD (any genotype) and ≥1 VOC leading to a healthcare visit within 12 months prior to screening. Patients (target enrollment N≥100) are stratified by age: Group 1 (12–<18 years), Group 2 (6–<12 years) and Group 3 (6 months–<6 years). Patients receive crizanlizumab on Day 1, Day 15, then every 4 weeks (up to 2 years). This analysis reports initial safety and efficacy results for Group 1 patients receiving crizanlizumab 5 mg/kg.
Results: As of 28 August 2020, 50 patients have been enrolled in Group 1 (median [min–max] age 14.9 [12.0–17.9] years; 58% female; 88% HbSS genotype; 64% Black/African American; 84% receiving hydroxyurea). Median (range) duration of crizanlizumab exposure was 36.6 (6–98) weeks; 88% of patients received treatment for ≥26 weeks.
The most common adverse events (AEs) regardless of causality with study treatment were headache (n=14 [28%]), vomiting (n=12 [24%]) and back pain (n=9 [18%]). Treatment-related AEs occurred in 12 (24%) patients. Grade ≥3 AEs occurred in 13 (26%) patients, most commonly anemia (n=3 [6%]) and back pain (n=2 [4%]). Grade ≥3 treatment-related AEs (back pain and pain in extremity) were reported in one (2%) patient. Eleven (22%) patients had serious AEs; none were deemed treatment related. No AEs led to treatment discontinuation except one patient who died of suspected meningitis (considered unrelated to treatment).
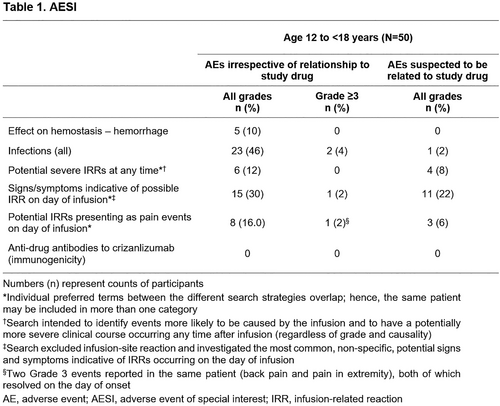
The incidence of AEs of special interest (AESI) is shown in Table 1. No infusion-related reactions were serious, and all had resolved at data cut-off, except for one case of Grade 1 dizziness. There were no cases of anaphylaxis to crizanlizumab. No pain events were serious, and all had resolved or were resolving by data cut-off.
The median (Q1–Q3) number of VOCs leading to a healthcare visit at baseline was 3.0 (1.0–5.0) versus 1.6 (0.0–3.7) while on treatment, a median absolute reduction from baseline of –1.0 (–3.0 to 0.5). At baseline, the median (Q1–Q3) rate of hospitalizations/emergency room visits was 4.0 (2.0–8.0) versus 1.5 (0.0–2.7) while on treatment, a median absolute reduction from baseline of –2.4 (–5.0 to 1.0). Eighteen (36%) patients did not experience a VOC leading to a healthcare visit during crizanlizumab treatment.
Summary – Conclusion: In this initial analysis, crizanlizumab 5 mg/kg was safe and well tolerated in patients with SCD aged 12–<18 years, consistent with the established profile of crizanlizumab in adults. No new safety signals were identified. Crizanlizumab 5 mg/kg led to a clinically relevant reduction in VOCs in this patient population compared with baseline.