Transconjunctival Blepharoplasty and the Use of the “Silent Assistant”
INTRODUCTION
Blepharoplasty refers to any technique that alters the appearance, position, or function of the eyelids (i.e., surgical correction of eyelid deformities).1 People of all ages and for a variety of conditions may undergo a blepharoplasty. The most common reason for patients to want a blepharoplasty is to improve the “bags” under the eyes, which are due to overabundance or pseudoherniation of the orbital fat.2
The transconjunctival approach was first described in 1924 in the French literature. However, most surgeons continued using the transcutaneous skin-muscle flap or skin-flap techniques.3 The transconjunctival technique offers the advantage of having no external scar and it preserves the integrity of the muscle sling that helps support the lower eyelid.2 Many of the complications of the transcutaneous approach are drastically reduced or avoided by the transconjunctival approach, such as lower eyelid retraction, ectropion, entropion, or inferior oblique palsy.4
We have found that a helpful technique is the use of the “silent assistant,” which is a suture placed in the conjunctival flap for retraction. This serves to protect the globe, retract the tissues, and eliminate extra instruments and hands needed in the area to give the surgeon better access to the operative field.
SURGICAL TECHNIQUE
Our technique for the transconjunctival blepharoplasty and the use of the silent assistant involves five steps. To clarify the terminology in this report, medial refers to the nasal aspect and lateral refers to the temporal aspect.
Step 1: Preoperative Procedure
The eyes are marked before surgery with the patient in the upright sitting position. In the operating theater the patient is placed in the supine position and given intravenous sedation. The local anesthetic is 1% lidocaine plus epinephrine 1:100,000 mixed with hyaluronidase as a 20 mL/1 mL anesthetic hyaluronidase solution. This is administered into three quadrants of the lower lid through the conjunctiva, down to the level of the bony ocular rim. First, the central sector is injected, followed by the medial and lateral sectors, respectively. The anesthetic is allowed to take effect for 15 to 20 minutes before proceeding, to obtain maximum benefit of anesthesia and hemostasis. Both eyes are injected simultaneously.
Step 2: Incision
A Pyrex eye shield is used to protect the globe, and a Desmarres retractor is used to retract the lower lid. The inferior ocular rim position is palpated and the conjunctiva is exposed. A needle-tipped, monopolar cutting electrocautery is used with a protective sheath around the shaft for further protection. The incision is made several millimeters below the tarsal plate and extends about 6 mm in length.
Step 3: Exposure
The medial extent of the incision extends to within 5 mm of the cul-de-sac, to avoid the punctum. It should be noted that the punctum extends 2 mm inferiorly before it turns medially. The 5-mm margin gives an adequate boundary of safety. If the incision needs to be enlarged, it should always be laterally. Iris scissors and a cotton-tipped applicator for retraction are used to dissect out the fat pads. Laterally, the incision may extend to the lateral rim of the orbit, just below the canthus.
Step 3: The “Silent Assistant”
Once the incision is made and the superior conjunctival flap separated, a 6-0 silk suture is placed into the superior edge of the conjunctival flap (Fig. 1). A clamp is placed on the suture, which is then draped over the brow and forehead. This allows the flap to be retracted in a superior position, by the weight of the clamp, to cover the globe. This self-retracting suture acts as the “silent assistant” to retract the tissues, protect the globe, and alleviate instruments and hands in the surgical field, in order to give the surgeon better access (Fig. 2).
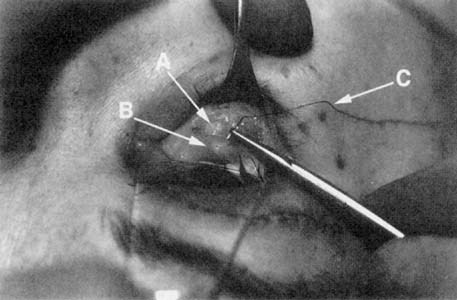
The “silent assistant.”Placement of a suture to retract the conjunctival flap superior (A = herniated fat pad; B = conjunctival flap; C = silk suture).

The silent assistant. The conjunctival flap being retracted to protect the globe (A = herniated fat pad; B = conjunctival flap; C = silk suture).
Step 4: Removal of Fat Pads
The fat from the medial and lateral compartments is dissected out first to expose the valley of the inferior oblique muscle and identify the inferior oblique muscle. The fat pad of the medial and central lower lid fat compartments is continuous, separated by the inferior oblique muscle. This fat pad is covered by fascia, which is the arcuate expansion of the inferior oblique muscle. Cutting this fascia makes the central and lateral fat pad sectors continuous. The medial fat pad is sequentially removed, and care is taken to keep the dissection planes smooth for a better cosmetic result. Once the fat has been removed from all three areas, the upper lid is palpated. This serves to exaggerate any remaining bulges or asymmetry in the lower lid. Pressure on the upper lid causes the fat pads to protrude from the lower-lid fat compartments. The amount of fat should be compared between the two eyes to evaluate the distribution of fat removal of the three compartments bilaterally. Relatively equal amounts of fat should be removed from the respective compartments of each eye.
Step 5: Immediate Postoperative Examination
Intraoperatively, the patient's vision and movement of the extraocular muscles are examined for deficits. Meticulous hemostasis is obtained using electrocautery. The silent assistant stitch is removed and the wound edges are re-approximated. The conjunctiva is not sutured. Both lids are examined for symmetry. Cold compresses are applied during the immediate postoperative period.
DISCUSSION
The transconjunctival approach reduces the incidence of postoperative eyelid retraction and ectropion compared with the traditional approaches.4, 5 There is no visible scar or eyelash distortion and it is a relatively minimally invasive procedure. Our experience is in line with previous studies that have shown a drastic reduction in complications, including less postoperative bruising than with the transcutaneous procedures. An important convenience for patients is that they are able to apply makeup to the lower lid the next day. This allows them to continue with their everyday life, instead of hiding until the bruising and healing have resolved. There are, however, disadvantages to the transconjunctival approach. For instance, the inexperienced surgeon may have a difficult time defining the correct tissue planes and the three fat compartments, which may lead to damage of the inferior oblique muscle.
The use of the silent assistant stitch provides the surgeon with improved exposure of the surgical field, thereby reducing the possibility of complications, as well as protecting the globe with the patient's own conjunctiva during the procedure. This decrease in the overall procedure time permits more efficient use of operating room staff and potentially contributes to producing a cosmetically improved result.
CONCLUSION
The use of the transconjunctival approach in conjunction with the silent assistant is our preferred method for a lower-lid blepharoplasty. To date, our patients have been very satisfied with the results.




