A glimpse into the psychological status of E.N.T inpatients in China: A cross-sectional survey of three hospitals in different regions
Abstract
Objective
To determine whether E.N.T inpatients have a higher prevalence of mental illness than the general population and whether certain diseases are more likely to be associated with mental illness than other diseases.
Methods
This cross-sectional survey was conducted in the E.N.T departments of three hospitals in different cities in China. The psychological status of all consecutive adult inpatients was assessed within 1–2 days following hospital admission using the Symptom Checklist-90 (SCL-90), Zung Self-Rating Depression Scale (SDS) and Zung Self-Rating Anxiety Scale (SAS). Inpatients from the general surgery and pneumology departments at the same hospital were enrolled and surveyed as control groups.
Results
The 439 patients enrolled in the final analysis accounted for 88.0% of all E.N.T inpatients during the study period. Of these patients, 16.4% were in an anxious state and 79.5% were in a depressive state. The overall anxiety (41.7 ± 9.7) and depression (55.9 ± 29.2) scores were much higher than Chinese norm (29.8 ± 10.0 and 33.5 ± 8.6, respectively), and significant differences were observed (t = 20.89, P < 0.01 and t = 13.12, P < 0.01, respectively). Although 18.7% of the E.N.T patients were psychiatric distress, these patients scored lower on the SCL-90 than the Chinese norm. Furthermore, the patients in the E.N.T department had a higher prevalence of anxiety and depression than those in the general surgery department but a similar prevalence to those in the respiratory department.
Conclusion
Psychological distress, particularly anxiety and depression, are widespread in patients with otolaryngological diseases. Therefore, the identification and treatment of co-occurring psychiatric disorders in this high risk and clinically challenging group of patients are urgent in China.
List of abbreviations
-
- ND
-
- nasal diseases
-
- LP
-
- laryngopharyngeal diseases
-
- OD
-
- otological diseases
-
- BT
-
- benign tumors of the head and neck
-
- MT
-
- malignant tumors of the head and neck
-
- OSA
-
- obstructive sleep apnea–hypopnea syndrome
-
- O
-
- others
-
- SCL-90
-
- the Symptom Checklist 90
-
- SDS
-
- the Zung Self-Rating Depression Scale
-
- SAS
-
- Zung Self-Rating Anxiety Scale
-
- SOM
-
- Somatization
-
- O–C
-
- Obsessive–Compulsive
-
- INT
-
- Interpersonal-Sensitivity
-
- DEP
-
- Depression
-
- ANX
-
- Anxiety
-
- HOS
-
- Hostility
-
- PHOB
-
- Phobic-Anxiety
-
- PAR
-
- Paranoid Ideation
-
- PSY
-
- Psychoticism
Introduction
Somatic diseases are often accompanied by psychological disorders. Up to 50% of general medical and surgical inpatients have symptoms indicative of psychological distress or disturbance, including depression, anxiety, and substance abuse,1-3 and an increasing number of studies have begun to focus on the relationship between psychiatric presentations and physical diseases. Patients with otorhinolaryngological diseases may be more susceptible to mental illness. Postolache et al4 demonstrated a state-level relationship, rather than only a trait-level relationship, between changes in allergy symptom scores and changes in depression scores in patients with recurrent mood disorders exposed to seasonal peaks in aeroallergens. Head and neck cancer patients exhibit the highest rates of major depressive disorder among all oncology patients; fifteen to fifty percent of these cancer patients experience major depressive disorder, which typically emerges during the course of treatment with peak symptoms occurring 2–3 months after diagnosis.5 Depression may be more common in chronic rhinosinusitis than previously recognized.6 Additionally, an increase in tinnitus annoyance was positively correlated with the severity of anxiety and depression in normal-hearing patients.7
Nevertheless, to date, it remains unclear whether E.N.T diseases result in a higher prevalence of mental health impairments or co-occurring psychiatric disorders amplify the subjective symptom scores of quality of life. Patients with common E.N.T diseases are more likely to show comorbidity with psychiatric disorders. Psychological interventions for this patient group are highly important for both patients and doctors. To properly manage patients with both E.N.T diseases and concurrent mental illness, these patients must first be identified. Therefore, obtaining a global understanding of the psychological status of E.N.T patients in China in a real-world inpatient setting and current social environment is urgent. The objective of this study was to determine whether E.N.T inpatients have a higher prevalence of mental illness than the general population and whether certain diseases are more likely to be associated with mental illness than other diseases using a cross-sectional survey in three different hospitals in different cities in China.
Materials and methods
Patients
To obtain an overview of China, this cross-sectional survey was conducted in the E.N.T departments of three hospitals in different cities in China. All hospitals are Level ⅢA and included the Affiliated Beijing Chaoyang Hospital of Capital Medical University in Beijing, the First Hospital of Shanxi Medical University in Shanxi Province, and the Heze Municipal Hospital in Shandong Province, which are extensively representative. The project was approved by the institutional review boards in all three cities. All patients enrolled in the study received written and oral information about the study and provided informed consent to participate.
All consecutive adult inpatients (≥18 years of age) with stable E.N.T-related illnesses were recruited for the study between March and May of 2015. The patients were interviewed within 1–2 days following hospital admission. The survey consisted of self-administered questionnaires that were administered by trained investigators in the hospital rooms.
The exclusion criteria included the following: (1) emergency hospitalization, (2) patients in a coma state or patients who were unable to communicate because of cognitive impairment, (3) severe ongoing depression or drug addiction, (4) patients who have been diagnosed with a mental disturbance, and (5) patients whose condition was unstable because of serious diseases of general vital organs, such as respiratory failure, cerebral hemorrhage, cerebral infarction, serious hepatic insufficiency, serious renal insufficiency, and diabetes with severe fluctuating blood sugar levels.
Summary of the otolaryngology disease categories: The patients were divided into the following 7 subgroups based on their disease classification: nasal diseases (ND), including chronic nasal-sinusitis or nasal septum deviation; laryngopharyngeal diseases (LP); otological diseases (OD), including chronic suppurative otitis media and ear cholesteatoma; benign tumors of the head and neck (BT); malignant tumors of the head and neck (MT); obstructive sleep apnea–hypopnea syndrome (OSA); and others (O). Since different diseases originating from the same location or organ always result in similar clinical symptoms or primary complaints, therefore, might result in the same mental impairment, this grouping strategy might offer additional information.
Inpatients from the general surgery and pneumology departments at the same hospitals were enrolled in March of 2015 and surveyed as the control group to represent surgical and medical inpatients, respectively.
Measures
All subjects completed self-reported questionnaires, including survey of demographic characteristics, the Symptom Checklist 90 (SCL-90), the Zung Self-Rating Depression Scale (SDS) and the Zung Self-Rating Anxiety Scale (SAS).
The SCL-90, which is also called the Self-Reporting Inventory or Hopkin's SCL,8 is one of the most popular psychopathological tests and is based on a factor analysis for global clinical populations. The SCL-90 consists of 90 self-reported questions, and each question is answered on a 5-point Likert scale (0 for not at all, 1 for slightly, 2 for moderately, 3 for quite a bit, and 4 for extremely), including the following nine subscale dimensions (domain): (1) Somatization (SOM), (2) Obsessive–Compulsive (O–C), (3) Interpersonal-Sensitivity (INT), (4) Depression (DEP), (5) Anxiety (ANX), (6) Hostility (HOS), (7) Phobic-Anxiety (PHOB), (8) Paranoid Ideation (PAR), and (9) Psychoticism (PSY). The SCL-90 was first introduced in China by Wang9 in 1984, and the Chinese version of the SCL-90 was published by Jin et al10 in 1986, which established a baseline score for each different population in China. In China, a total average score higher than 1.44 on the SCL-90 indicates a more urgent need for individual intervention. An average subscale score greater than 2 provides detailed information regarding the type and severity of the symptom.
The development and use of the SDS and SAS have proven to be valuable in the assessment of anxiety and depression in a group of hospitalized inpatients.11, 12 These scales are standard mental assessment instruments, and the reliability and validity of the Chinese versions have been evaluated in a Chinese population.13, 14
The SDS self-report questionnaire contains 20 items that were constructed based on the clinical diagnostic criteria that are most commonly used to characterize depressive disorders and cover the affective, psychological and somatic symptoms associated with depression.11 The SDS includes ten symptomatically positively worded and ten symptomatically negatively worded questions, and each question is scored on a scale of 1–4 (1 = a little of the time, 2 = some of the time, 3 = a good part of the time, 4 = most of the time). The severity of the depression can be measured by dividing the sum of the raw score values obtained on the 20 items by the maximum possible score of 80, and the scores range from 0.25 to 1.0. In the Chinese population, an index lower than 0.53 indicates that an individual does not show signs of depression; a score of 0.53–0.62 indicates that an individual suffers from low depression, a score of 0.63–0.72 indicates that an individual suffers from moderate depression and a score greater than 0.72 indicates that an individual suffers from severe depression.
The SAS consists of 20 questions that can also be scored from 1 to 4 (1 = a little of the time, 2 = some of the time, 3 = a good part of the time, 4 = most of the time). Fifteen questions are scaled, and the numbers increase as the symptoms worsen. The scores of the remaining five questions decrease as the symptom severity decreases. The severity of anxiety can be measured by an index equal to the SAS score/80 (the total points). In the general Chinese population, the index also has the following 4 clinical categories: no anxiety (lower than 0.5); low anxiety (0.50–0.59); moderate anxiety (0.60–0.69) and severe anxiety (higher than 0.70).
To identify a simple method for screening patients for psychological problems, the severity of the general patient symptoms was evaluated using the Visual Analogue Scale (VAS), which uses a vertical 10 cm VAS from 0 to 10 with gradations (0 indicating the non-occurrence symptoms and 10 indicating the highest intensity of possible symptoms). Participants are free to choose any point on this scale based on their subjective sensation of their symptoms.
Statistical analysis
The data are expressed as a frequency for the nominal variables and as the mean ± standard deviation (SD) for the continuous variables. The statistical analyses were conducted using SPSS 16.0 software (SPSS Inc, Chicago). Various statistical methods were utilized depending on the experiment.
One-way analysis of variance (ANOVA) was performed to examine differences among the demographic variables. Pearson Chi-square test or the Fisher probabilities method was performed to compare the morbidity rate or gender proportions among the different groups. Single sample T test was used to compare the score values of E.N.T sample with general population. A linear regression analysis was performed to determine the relationship between the VAS and SAS, SDS and SCL-90. Differences were considered statistically significant at the 5% level (P < 0.05).
Results
Demographic characteristics
In total, 476 inpatients from E.N.T departments who met the inclusion criteria were included in the survey, including 439 patients who completed the questionnaire without missing data in the final data analysis, which resulted in a response rate of 92.2%. The control group consisted of 209 inpatients from the general surgery department who also participated in the survey, including 184 inpatients who completed the questionnaire, which resulted in a response rate of 88.0%. Finally, 84 of the 93 (90.3%) inpatients from the department of respiration completed the questionnaire without missing data. Descriptions of the study subjects are shown in Table 1. The mean age of the 707 participants at the time of the interview was 47.0 ± 15.9 years, including 373 males (52.8%) and 334 females (47.2%). Fig. 1 displays the distribution of various diseases in the E.N.T departments from the three hospitals at the time of the interview. ND, LP and OD accounted for the majority of inpatients in the E.N.T departments at each hospital.
| Department | Hospital | Total cases (n) | Cases included (%) | Cases with complete data | Proportion of complete data (%) | Age (y,  ± s) ± s) |
Gender Male/Female |
|---|---|---|---|---|---|---|---|
| E.N.T | Chaoyang | 245 | 219 (89.4) | 207 | 94.5 | 41.7 ± 13.2 | 122/85 (1.44) |
| Shanyi | 182 | 166 (91.2) | 148 | 89.2 | 49.7 ± 17.1 | 82/66 (1.24) | |
| Heze | 101 | 91 (90.1) | 84 | 92.3 | 42.2 ± 13.8 | 45/39 (1.15) | |
| General Surgery | Chaoyang | 63 | 52 (82.5) | 46 | 88.5 | 45.2 ± 16.8 | 18/28 (0.64) |
| Shanyi | 133 | 113 (85.0) | 98 | 86.7 | 55.2 ± 15.4 | 34/64 (0.53) | |
| Heze | 49 | 44 (89.8) | 40 | 90.9 | 46.3 ± 17.1 | 20/20 (1.00) | |
| Respiration | Chaoyang | 35 | 29 (82.9) | 27 | 93.1 | 53.9 ± 13.6 | 18/9 (2.00) |
| Shanyi | 42 | 35 (83.3) | 32 | 91.4 | 61.2 ± 20.1 | 18/14 (1.29) | |
| Heze | 35 | 29 (82.9) | 25 | 86.2 | 54.2 ± 13.4 | 16/9 (1.78) | |
| Total 1 | 528 | 476 (90.2) | 439 | 92.2 | 42.3 ± 13.8 | 249/190 (1.31) | |
| Total 2 | 245 | 209 (84.2) | 184 | 88.0 | 50.6 ± 16.7 | 72/112 (0.64) | |
| Total 3 | 112 | 93 (83.1) | 84 | 90.3 | 55.8 ± 15.5 | 52/32 (1.63) | |
| Total 4 | 885 | 778 (88.0) | 707 | 90.9 | 47.0 ± 15.9 | 373/334 (1.12) |
- Total 1: E.N.T Department; Total 2: General Surgery Department; Total 3: Respiration Department; Total 4: Three Departments.
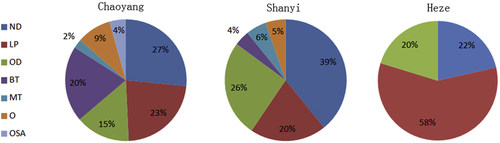
Distribution of diseases in E.N.T departments at three hospitals. ND: nasal diseases; LP: laryngopharyngeal diseases; OD: otology diseases; BT: benign tumor; MT: malignant tumor; OSA: obstructive sleep apnea–hypopnea syndrome; O: others.
Mental health problems in the inpatients
Table 2 displays the prevalence of psychiatric distress, anxiety and depression in the patients from the three departments located at three different hospitals.
| Department | Hospital | n | SCL-90 (%) | SAS | SDS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | Total (%) | Mild | Moderate | Severe | Total (%) | ||||
| E.N.T | Chaoyang | 207 | 24 (11.6) | 25 | 1 | 2 | 28 (13.5) | 74 | 91 | 4 | 169 (81.6) |
| Shanyi | 148 | 34 (23.0) | 14 | 0 | 0 | 14 (9.5) | 12 | 34 | 74 | 120 (81.1) | |
| Heze | 84 | 24 (28.6) | 26 | 4 | 0 | 30 (35.7) | 40 | 18 | 2 | 60 (71.4) | |
| General Surgery | Chaoyang | 46 | 7 (15.2) | 8 | 2 | 1 | 11 (23.9) | 16 | 21 | 2 | 39 (84.8) |
| Shanyi | 98 | 9 (9.2) | 1 | 1 | 0 | 2 (2.0) | 24 | 35 | 3 | 62 (63.3) | |
| Heze | 40 | 4 (10.0) | 2 | 1 | 0 | 3 (7.5) | 10 | 15 | 2 | 27 (67.5) | |
| Respiration | Chaoyang | 27 | 11 (40.7) | 5 | 1 | 2 | 8 (29.6) | 12 | 10 | 1 | 23 (85.2) |
| Shanyi | 32 | 4 (12.5) | 2 | 1 | 0 | 3 (9.4) | 2 | 6 | 13 | 21 (65.6) | |
| Heze | 25 | 4 (16.0) | 2 | 1 | 0 | 3 (12.0) | 6 | 8 | 5 | 19 (76.0) | |
| Total 1 | 439 | 82 (18.7) | 65 | 5 | 2 | 72 (16.4) | 126 | 143 | 80 | 349 (79.5) | |
| Total 2 | 184 | 20 (10.9) | 11 | 4 | 1 | 16 (8.7) | 40 | 56 | 5 | 128 (69.6) | |
| Total 3 | 84 | 19 (22.6) | 9 | 3 | 2 | 14 (16.7) | 20 | 24 | 19 | 63 (75.0) | |
- Total 1: E.N.T Department; Total 2: General Surgery Department; Total 3: Respiration Department; SCL-90: Symptom Checklist-90; SAS: Zung Self-Rating Anxiety Scale; SDS: Zung Self-Rating Depression Scale.
According to the SAS, of the 439 E.N.T patients, 16.4% were in an anxious state, including mild anxiety (14.8%), moderate anxiety (1.1%) and severe anxiety (0.5%). The overall anxiety score in the E.N.T patients (41.7 ± 9.7) was much higher than that of the Chinese norm (29.8 ± 10.0),14 and a significant difference was observed (t = 20.9, P < 0.01). The patients in the E.N.T departments had a higher prevalence of anxiety than those admitted to the departments of general surgery (8.7%, Chi-square values = 6.346, P = 0.012) but similar to those in the departments of respiration (16.7%, Chi-square values = 0.004, P = 0.952).
According to the SDS, 79.5% of the 439 E.N.T patients were in a depressive state (Table 2), including mild depression (28.7%), moderate depression (32.6%) and severe depression (18.2%). The overall depression score of the E.N.T patients (55.9 ± 29.2) was much higher than Chinese norm (33.5 ± 8.6),13 and a significant difference was observed (t = 13.1, P < 0.01). Depression was higher in the E.N.T patients than that in the patients from the departments of general surgery (69.6%, Chi-square values = 7.130, P = 0.008). There was no difference between the E.N.T patients and those from the department of respiration (16.7%, Chi-square values = 0.854, P = 0.356).
According to the SCL-90, 18.7% of the E.N.T inpatients were in psychiatric distress, which is higher than that in the department of general surgery (10.9%, Chi-square values = 5.775, P = 0.016) but not higher than that in the department of respiration (16.0%, Chi-square values = 0.703, P = 0.402). However, the E.N.T patients scored lower on the clinical score on the SCL-90 (1.3 ± 0.4) than the general Chinese population (1.4 ± 0.4, P < 0.01).
There are significant differences in the prevalence of abnormal SAS and SCL-90 scores in the E.N.T inpatients among the three hospitals (P = 0.004). The Heze hospital had a higher prevalence than the other two hospitals. The depression scores did not differ among the three hospitals (Chi-square values = 4.168, P = 0.124).
The severity of the symptoms evaluated by the VAS was significantly positively correlated with the severity of the anxiety symptoms (F = 17.322, r = 0.353, P = 0.001) and the SCL-90 scores (F = 4.297, r = 0.184, P = 0.040). The optimal cut-off point to differentiate between the positive and negative anxiety status in the E.N.T inpatients was a VAS score of 5 (Linear regression equation y = 0.431 + 0.016x).
Table 3 displays the prevalence of psychiatric distress, anxiety and depression in patients with different diseases in the E.N.T department. Patients with OD showed the highest prevalence of anxiety (23.5%), followed by patients with benign tumors and LP (18.8% and 18.3%, respectively). The only two severely anxious patients suffered from ND.
| Group | n | SCL-90 (%) | SDS | SAS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | Total (%) | Mild | Moderate | Severe | Total (%) | |||
| ND | 131 | 32 (24.4) | 40 | 42 | 25 | 107 (81.7) | 12 | 0 | 2 | 14 (10.7) |
| LP | 126 | 24 (19.0) | 37 | 44 | 14 | 95 (75.4) | 22 | 1 | 0 | 23 (18.3) |
| OD | 85 | 19 (22.4) | 21 | 22 | 24 | 67 (78.8) | 16 | 4 | 0 | 20 (23.5) |
| BT | 48 | 6 (12.5) | 17 | 22 | 2 | 41 (85.4) | 9 | 0 | 0 | 9 (18.8) |
| MT | 13 | 0 | 3 | 3 | 4 | 10 (76.9) | 1 | 0 | 0 | 1 (7.7) |
| OSA | 27 | 1 (3.7) | 5 | 6 | 10 | 21 (77.8) | 4 | 0 | 0 | 4 (14.8) |
| O | 9 | 0 | 3 | 4 | 1 | 8 (88.9) | 1 | 0 | 0 | 1 (11.1) |
| Total | 439 | 82 (18.7) | 126 | 143 | 80 | 349 (79.5) | 65 | 5 | 2 | 72 (16.4) |
- ND: nasal diseases; LP: laryngopharyngeal diseases; OD: otology diseases; BT: benign tumor; MT: malignant tumor; OSA: obstructive sleep apnea–hypopnea syndrome; O: others; SCL-90: Symptom Checklist-90; SAS: Zung Self-Rating Anxiety Scale; SDS: Zung Self-Rating Depression Scale.
The percentage of severe depression in the positive E.N.T patients screened by the SDS was higher in the patients with OSA (47.6%), malignant tumors (40.0%) and OD (35.8%). Patients with benign tumors and ND were more vulnerable to depression. There were no significant differences in the SCL-90 scores among individuals with ND, LP and OD (Chi-square values 1.098, P = 0.578).
Factor analyses of the SCL-90
The patients in the E.N.T department of the Heze Hospital had a high prevalence of psychiatric distress in all ten domains of the SCL-90, followed by Shanyi Hospital. The subscale dimensions of O–C and hostility were the most common psychiatric symptoms in the E.N.T inpatients (Fig. 2). The prevalence of the psychiatric symptoms of SOM, hostility and paranoid ideation were higher in the patients with ND and OD than that others. Psychoticism was common in the patients with LP (Fig. 3).
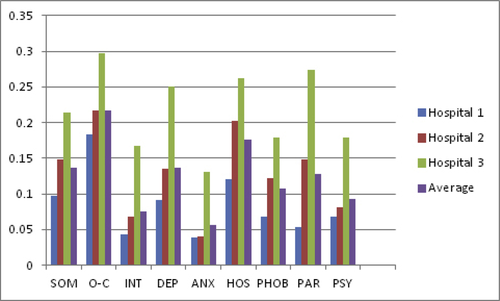
Prevalence of psychological distress in nine domains of the SCL-90 in patients with E.N.T diseases at three hospitals. The nine subscale dimensions are (1) SOM, (2) O–C, (3) INT, (4) DEP, (5) ANX, (6) HOS, (7) PHOB, (8) PAR, and (9) PSY. SOM: Somatization; O–C: Obsessive–Compulsive; INT: Interpersonal-Sensitivity; DEP: Depression; ANX: Anxiety; HOS: Hostility; PHOB: Phobic-Anxiety; PAR: Paranoid Ideation; PSY: Psychoticism.
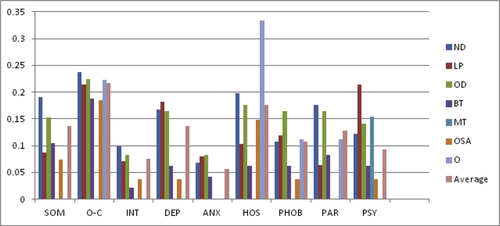
Prevalence of psychological distress in nine domains of the SCL-90 in patients with different E.N.T diseases. The nine subscale dimensions are (1) SOM, (2) O–C, (3) INT, (4) DEP, (5) ANX, (6) HOS, (7) PHOB, (8) PAR, and (9) PSY. SOM: Somatization; O–C: Obsessive–Compulsive; INT: Interpersonal-Sensitivity; DEP: Depression; ANX: Anxiety; HOS: Hostility; PHOB: Phobic-Anxiety; PAR: Paranoid Ideation; PSY: Psychoticism.
Consistent with results of the SDS and SAS, depression was more common than anxiety in the E.N.T patients. However, the percentages of individuals with depression (60/439) and anxiety (25/439) screened by SCL-90 factor analysis were significantly lower than those evaluated by the SDS (349/439, 13.7% vs. 79.5%, P < 0.001) and SAS (72/439, 5.7% vs. 16.4%, P < 0.001).
Discussion
To the best of our knowledge, this study is the first to address the psychological status of E.N.T patients in three Chinese cities in a nearly real-world inpatient setting and social environment. The patients enrolled in the study accounted for 88.0% of all E.N.T inpatients during the study period.
Our results show that the prevalence of both anxiety and depression is more common in E.N.T patients than that in the general Chinese population. The prevalence of depression was nearly eight times greater than that of anxiety (81.7% vs. 9.2%). Furthermore, the patients in the E.N.T departments had a higher prevalence of anxiety and depression than those in the departments of general surgery but similar rates to the patients in the departments of respiration. Although 18.7% of the E.N.T patients were in psychiatric distress, they had lower clinical scores on the SCL-90 assessment than the general Chinese population. Furthermore, the patients with OD showed the highest prevalence of anxiety, followed by patients with benign tumors and LP. The only two severely anxious patients suffered from ND. More than one-third of the patients with OSA, malignant tumors and OD suffered from serious depression in the E.N.T group according to the SDS analysis. Moreover, the data show that the psychiatric symptoms of SOM, hostility and paranoid ideation are more common in patients with nasal and OD. Psychoticism is common in patients with LP. Therefore, patients with different E.N.T diseases experience different mental illnesses. There are significant differences in the prevalence of abnormal of SAS and SCL-90 scores in the E.N.T inpatients among different hospitals.
Despite the differences in methodologies, most published studies indicate some type of indistinct relationship between E.N.T-related diseases and mood syndromes.
Recently, an investigation of 117 Chinese patients with CRS demonstrated that the SAS and SDS scores (39.4 ± 11.6, 54.1 ± 11.0) were significantly higher than average,15 which is consistent with our results. Another study showed that psychiatric distress was prevalent in ninety-five patients awaiting surgery for CRS who were assessed using the psychiatric distress questionnaire (BSI and PHQ); 17% of these patients tested positive for anxiety, and 25% of these patients tested positive for depressive disorders.16 In a Chronic Rhinosinusitis Epidemiology Study (CRES), patients with CRS visiting E.N.T outpatient clinics at 30 centers across the United Kingdom showed significantly higher mental health morbidity than controls across the mental health and emotional well-being domains of the SF-36 (QoL – quality of life tool) and SNOT-22 (a nasal symptom score), particularly those with CRSsNPs.17 Although it remains controversial whether anxiety and depression can influence a patient's subjective symptom scores in chronic rhinosinusitis,16, 18, 19 anxiety and depression are prevalent in patients with CRS despite a number of methodological variances. A literature review by Sansoneet al. 20 found that most published studies indicate that individuals with allergies, which is another common nasal disease, appear to be at a higher risk of an unknown degree for developing various types of anxiety or mood syndromes. The most common symptoms, such as a runny nose, sneezing, and nasal congestion, contribute to the same mental conditions as those in patients with CRS and AR. Hence, in this study, we classified all types of ND into one subgroup for the analysis, although most patients with AR do not require hospitalization. The same grouping strategy was used during the data analysis. However, there is one study that provided a different result.21 Notably, patients who are waitlisted for ESS did not demonstrate any significant level of psychiatric distress.
Hearing impairments, tinnitus and dizziness, which are most common symptoms of OD, are recognized causes of emotional and psychological disturbances worldwide. A systematic review by Theunissen22 reported that the literature consistently demonstrates that hearing-impaired children and adolescents are more prone than their normally hearing peers to develop depression, aggression, oppositional defiant disorder and psychopathy. In a survey of 544 patients experiencing dizziness as measured by the Beck Depression Inventory (BDI) and the Spielberger State-Trait Anxiety Inventory (STAI), the prevalence of high depression and anxiety scores were 11% and 18%, respectively. Bhatt7 found that 26.1% of the 21.4 million adult tinnitus sufferers reported problems with anxiety in the preceding 12 months, while 25.6% showed signs of depression. Those reporting tinnitus symptoms as a “big” or “very big” problem were more likely to concurrently report anxiety and depressive symptoms. The inpatients surveyed in the study with different OD are at risk of developing mental problems.
Studies investigating the relationship between psychopathological problems and common pathologies of the pharynx and larynx are scarce. Pooled data analyzed from 160 patients with muscle tension dysphonia,23 benign vocal fold lesions, paradoxical vocal fold movement disorder, or glottal insufficiency indicated that 25.0%, 36.9%, and 31.2% of the patients showed elevated stress, anxiety, and depression scores, respectively. Tang et al 24 reported that anxiety (39.8%), depression (31.2%) and sleep disorders (23.7%) were significantly more common in individuals with globus sensation, which is one of the common symptoms of throat and pharyngeal illness, that in healthy controls. In this study, we found that anxiety and depression are common in inpatients with LP, even though most of these diseases are vocal fold-related diseases.
Surprisingly, our data show that patients with benign tumors are more susceptible to mental issues than those with malignant tumors (SAS: 9/48, 18.8% vs. 1/13 7.7%; SDS: 41/48, 85.4% vs. 10/13, 77.8%). Patients with benign and malignant tumors face similar situations, such as fears of the unknown, malignant transformation, mortality, possible side effects, complications induced by treatment, and concerns regarding the long-term effects of the tumor and treatment on their quality of life. Psychological distress is, therefore, common in patients with cancer or benign tumors, and depression and anxiety are highly typical.25, 26 William et al.5 found that the prevalence of depression in head and neck cancer patients ranges from 15% to 50%. Despite the small sample size, our results suggest that the psychological comorbidities of patients with tumors, regardless of malignancy, should be given increased attention.
Several studies have highlighted the association between OSA and depression and anxiety with a rate of 17%–41%.27-30 Because of the overlap in symptoms between the two conditions, such as insomnia, fatigue, decreased libido, irritability, weight changes, and cognitive difficulties, the assessment of depression in OSA is challenging, and it is difficult to find a reliable method to identify depression and anxiety in the presence of OSA. Different questionnaires have varying proportions of shared symptoms, including the SAS and SDS used in this study, which might increase the prevalence of depression in OSA.31 Moreover, structural and functional brain alterations have been found in anxious OSA subjects.32 More studies should be performed to clarify the possible pathophysiological mechanisms that could explain how obstructive sleep apnea can cause or worsen depression.
Based on the discussion thus far, psychological comorbidities are common among nearly all types of illnesses found in patients admitted to E.N.T departments. In addition, these mental issues exist broadly among those with otorhinolaryngologic diseases. It is important to provide a framework for subsequent investigations aiming to elucidate the scope, type and extent of the different types of E.N.T disorders. The results of our study are consistent with previous investigations. A multitude of factors might cause depression and anxiety in this group, such as sex, age, and socio-economic status. Hospitalization by itself is one of the most important factors. Previous studies have described a high prevalence of psychiatric comorbidity among general medical and surgical patients based on various assessment tools.33 In our study, the prevalence of psychological distress or disturbance was also high in the respiratory department and general surgery department. Booth et al2 reported that almost half (46.6%) of 1007 medical and surgical inpatients met the lifetime criteria for at least one diagnostic mental disorder, including 9.0 percent who showed signs of major depression or dysthymia, which is consistent with other reports.1, 34 Somatic illnesses and their consequences evoke strong emotions. These emotions may affect the course of the illness and the treatment efficacy through their physiological components. Since the presence of these conditions has been found to be associated with increased costs, length of stay and excess utilization of general medical services,35-37 investigations of mental status on a large scale are warranted.
In addition to the common factors, the psychological state is significantly affected by the special symptoms induced by diseases, which might result in a different prevalence and type of psychological distress among various diseases. Our study revealed that patients with E.N.T diseases more frequently suffer from comorbid psychiatric illnesses than the patients in the control groups. This phenomenon may be attributed to the part of the body affected by the E.N.T diseases. For example, the most basic aspects of one's humanity, including the ability to speak, eat, breathe, and appear in public, may all be affected by laryngeal diseases or its treatment. Another reason maybe the interaction between the somatic symptoms and mental states. For instance, the common symptoms of nasal illness, such as obstruction, increase the risk of developing mental health problems. However, excessive anxiety and depression might exacerbate the subjective sensation of nasal discomfort.
Our study also highlighted that some differences in mental disorders are present between different type of diseases and different hospitals, which suggests that mental problems are more common and complicated in these specialized medical settings. For example, the psychiatric symptoms of SOM, hostility and paranoid ideation are more common in patients with ND and OD. It is of great importance to clarify the possible factors that increase the risk of hostility and paranoid ideation in this specific population. Different mechanisms may contribute to the situations of each disease, which suggests that attention should be paid to both the universality and particularity of the specific mental disorder experienced by the individual patient.
Although E.N.T doctors tend to be familiar with common co-occurring psychiatric disorders in certain E.N.T diseases, they are not always adept at diagnosing and treating concurrent mental illness. Thus, an understanding of this relationship and consideration of this situation during clinical training are essential. Our study provides a global scope of the psychological status of Chinese E.N.T patients in a nearly real-world inpatient setting and social environment, which has great positive implications for future research endeavors.
Another finding of the study is that the proportion of patients with anxiety and depression as identified by the SCL-90 (5.7% and 13.7%, respectively) was much lower than that found in patients screened with the SAS and SDS, which suggests that the SCL-90 does not sufficiently reflect these two common mental illnesses. However, the SCL-90 is best able to identify mental illnesses other than anxiety and depression. For instance, the analysis of the SCL-90 demonstrated that hostility is common in E.N.T inpatients. This knowledge is essential for targeted screenings and interventions. Notably, this does not imply that more is better because it is not easy for subjects to complete more than one questionnaire with high quality at one time. Thus, it is crucial to have reliable, simple, and sustainable methods for symptom monitoring that can be readily incorporated into daily medical practice.
The VAS has been found useful for assessing patients' subjective experiences or perceptions of a variety of clinical phenomena.38-40 In the present study, the severity of diseases evaluated by the VAS score was significantly positively correlated with the severity of anxiety symptoms and the SCL-90 score but not depression. Patient-based symptom severity scoring systems may be influenced by external factors, such as the patient's age, expectations, culture, and physical and mental capabilities; it is, therefore, perhaps not surprising that there is a correlation between the severity of the disease and its symptoms. Although the VAS is a simple and rapid evaluation of the overall disease severity in a primary care and specialist setting, its accuracy and reliability should be further evaluated in screening mental disturbances in E.N.T inpatients.
Since the association between psychiatric comorbidity and specific diagnoses is known, we did not limit the study to certain medical conditions. The decision to include all possible diagnoses without strict inclusion and exclusion criteria was made to mimic a real clinical setting to ensure that the prevalence estimates are more generalizable. Accordingly, one must be cautious when interpreting the results with respect to a particular subgroup because of the limited sample size. Notably, consistent with most prospective studies investigating psychiatric comorbidity in general medical or surgical inpatients, the prevalence relied on mental health symptoms rather than on psychiatric diagnoses, which might result in an overestimate of the presence of mental illnesses. There is no current information regarding the mechanisms underlying the increased prevalence of psychiatric disorders in this specific population. Further studies should evaluate the specific role of these conditions in selected categories of E.N.T disorders in susceptible individuals.
In summary, to the best of our knowledge, this study is the first to systematically investigate the specificity of the relationships among psychiatric distress, anxiety and depression and each of the major disorders in Otolaryngology within a single study sample. Our work underscores that the successful treatment of patients with E.N.T diseases should involve medical, social, and psychological interventions. Increased knowledge regarding this relationship might significantly improve diagnostic accuracy and treatment outcomes for both otolaryngology illness and concurrent mental disturbances.
Conclusion
In summary, this study has shown that psychological distress, particularly anxiety and depression, are widespread in patients with otolaryngological diseases. This study highlights the importance of identifying and treating co-occurring psychiatric disorders in this high risk and clinically challenging group of patients.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the hospitals' research committee (2015 LL128) and the 1964 Helsinki Declaration and its subsequent amendments.
Authors' contributions
TJ designed the experiment, analyzed and interpreted the patient data, and was a major contributor in writing the manuscript. LL, HF, HR and TC performed the investigation in different hospitals. ZS collected, analyzed and interpreted the patient data. All authors read and approved the final manuscript.
Funding
This study was funded by The Key Research and Development Program Funding of Shanxi Province (201603D121039).
Conflicts of interest
The authors declare that they have no conflicts of interest.