A lesion mimicking malignancy in the cesarean scar: Decidualize endometriosis
Dear Editor,
We are presenting a case of cutaneous endometriosis with decidualization in a cesarean section scar.
Endometriosis is a benign estrogen-dependent condition found in 6–10% of the female population. It is characterized by the presence of endometrial glands and stroma outside the uterus. It is more commonly found within the female pelvic cavity, attacking the ovaries, the rectovaginal pouch and the peritoneum of the genital floor. Less frequently, it can occur in extrapelvic sites, especially in abdominal surgery scar areas following hysterectomy and cesarean section, and in the perineum following vaginal deliveries with episiotomy [1]. Rarely endometriosis under the influence of progesterone, either from pregnancy or exogenous sources, can demonstrate decidualization [2]. These histopathologic findings can be mistaken for malignancy.
A 33-year-old woman presented with the mass from the area compatible with old cesarean scar. Gross examination of the excised mass was 3 × 2 × 1.5 cm. The cut surface was creamy-white with a nodular appearance. In histopathological evaluation, there was a proliferation of variable sized glands lined by large polygonal cell aggregates with abundant granular, eosinophils (Figures 1A and 1B). Mitotic figures were absent. The decidual cells were nuclear positive for progesterone receptor (PR) (Figure 1C) and strongly positive for CD10 (Figure 1D) and vimentin. They were negative for a panel of estrogen receptor (ER), cytokeratin (CK), epithelial membrane antigen, p63, desmin, CD68, and calretinin. The glandular epithelial cells were positive for CK AE1/AE3, CK 7, and PR, but negative for CK 5/6, ER, and calretinin. The histological diagnosis was cutaneous endometriosis with marked decidualization.
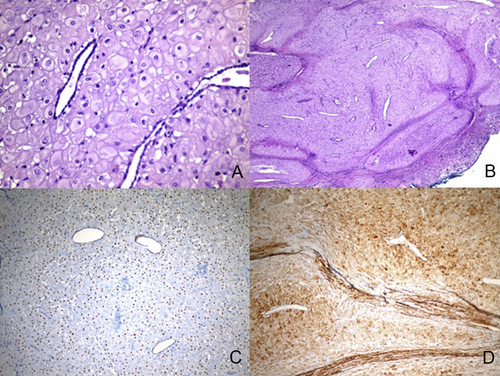
(A–B) Nodular proliferation of variable sized glands lined by large polygonal cells resembling the pregnancy-like response of the endometrium to progestin [hematoxylin and eosin: (A) × 400; (B) × 40]; (C) nuclear positivity with progestin receptor (×200); (D) cytoplasmic positivity with CD10 (×100).
During pregnancy, decidualization can occur externally to the uterus; the stromal cells become epithelioid, plump, and eosinophilic decidual cells [3]. This phenomenon has been attributed to progestational effects on endometriosis. This assumption is supported by the fact that the endometrium is the natural precursor of decidua and by the similar topographic distribution of endometriotic and gestational decidual tissue within the peritoneal cavity.
The primary importance in recognizing decidual tissues resides in separating them from other morphologically similar entities that are included in the differential diagnosis based on morphology. Malignant mesothelioma can be very similar to decidua. A morphological variant initially thought to afflict only young women has been described and is characterized by large polygonal cells with ample glassy eosinophilic cytoplasm and prominent nucleoli, and a poor prognosis. The term deciduoid malignant mesothelioma is used to reflect this similarity [4]. The tumors described in these cases retain the classic immunophenotype of conventional mesotheliomas; therefore, these tumors express calretinin and CKs (including CK 5/6) but demonstrate negative staining for ER and PR [5]. A panel of antibodies should be used to determine this distinction. Samples from the present case did not immunoreact with any of the CKs tested or with calretinin. Additional features suggestive of malignancy (e.g., cytological atypia and increased mitotic activity) were also absent. An immunohistochemical panel can help to differentiate decidulize endometriosis from other similar entities.




