Use of the Burch–Schneider cage and structural allografts in complex acetabular deficiency: 3- to 10-year follow up
Abstract
This study aimed to evaluate retrospectively the clinical outcomes and complications of structural allografts and Burch–Schneider antiprotrusio cages to treat severe acetabular defects in revision total hip arthroplasty (THA). Between July 2003 and December 2010, 29 patients (representing 31 hips) underwent revision THA using structural allografts and Burch–Schneider cages for acetabular reconstruction. The patients had a mean age of 59 years (range, 37–79 years). Seventeen hips had a Paprosky IIIA defect, 12 hips had a IIIB defect, and two hips had a pelvic discontinuity (PD) acetabular defect. After a mean follow up of 5.5 years (range, 3.0–10.5 years), all patients, except for two patients with recurrent infections, significantly improved, based on the mean Harris hip score (30 points vs. 67 points, p < 0.001) and the Western Ontario and McMaster Universities Arthritis index (WOMAC) score (65 points vs. 32 points, p < 0.001). Using re-revision surgery as the endpoint, the cage had a survival rate of 76% [95%, confidence interval (CI), 67.4–84.6%] at 5 years and 57% (95% CI, 39.3–74.7%) at 10 years. Other complications included hip dislocation [3 (9.7%) hips]; deep infection [3 (9.7%) hips]; and sciatic nerve impingement, vesicle-acetabular fistula, and leg lengthening [1 (3.2%) hip]. There was a trend toward a higher failure rate in hips with four revisions, compared to hips with three revisions or fewer (p = 0.055). Three hips with a failed cage underwent re-revision surgery using a standard noncemented acetabular component. In conclusion, a structural allograft with Burch–Schneider antiprotrusio cage for complex acetabular defect is a technique-demanding procedure with a 5-year survival rate of 76%. Even with failed cage reconstruction, re-revision surgery with a noncemented acetabular component may be feasible once the allograft has healed.
Introduction
Massive acetabular bone deficiency is a challenging problem during revision total hip arthroplasty (THA). Acetabular bone loss may occur because of osteolysis, infection, stress-shielding, or mechanical destruction by a loose component [1]. Options for reconstruction include jumbo or extra-large cups [2]-[4], small structural allografts with conventional acetabular components [5], morselized allografts with cemented cup [6]-[8], or a trabecular metal cup [9]. However, for complex acetabular deficiencies such as a Paprosky type III defect or pelvic discontinuity (PD), an antiprotrusio cage with structural bone grafts may be required [10]-[12]. The Burch–Schneider cage reconstruction has the advantages of bridging the acetabular deficiency and protecting the structural bone graft until it incorporates into the host bone [13]. However, there is a substantial cage failure rate of 10.5–34.0% in midterm follow up [7], [11]-[14]. The aim of the study was to evaluate retrospectively the clinical outcomes and complications of using the Burch–Schneider antiprotrusio cage and structural allografts for complex acetabular reconstruction with a minimal follow up of 3 years.
Methods
Failed THAs with complex acetabular deficiency reconstruction via antiprotrusio cage and structural allografts that were performed between July 2003 and December 2010 were reviewed retrospectively. The inclusion criteria were (1) failed THAs with a Paprosky III defect [15] or (2) a grade 3 or 4 acetabular defect, based on the American Academy of Orthopedic Surgeons (AAOS) system criteria [16], that required a structural femoral head or distal femoral allograft to reconstruct the segmental defect of the acetabulum, which was supported by a Burch–Schneider antiprotrusio cage. The exclusion criteria were (1) use of cages or rings for acetabular deficiency in primary THA, (2) use of antiprotrusio cages and morselized allografts or small structural allografts in the cavitary defects of the acetabulum after failed THAs, and (3) hips with Paprosky type II defects that were reconstructed by a primary acetabular component and structural or morselized bone grafts.
Thirty-four patients (representing 36 hips) were included, five patients (representing 5 hips) were excluded, three patients died of a malignancy within 2 years postoperatively, and two patients were lost to follow up. Thus, 29 patients remained: 11 males and 18 females (representing 31 hips) with a mean age of 59 years (range, 37–79). They had a complete clinical follow up for at least 3 years. Disease diagnoses were osteoarthritis in 12 hips; osteonecrosis of the femoral head in 10 hips, which included two hips with acetabulum osteonecrosis due to irradiation therapy for cervical cancer; post-traumatic arthritis in four hips; rheumatoid arthritis in one hip; ankylosing spondylitis in one hip; pigmented villonodular synovitis in one hip; and tuberculosis in two hips.
Index revision surgery was the first revision in 14 (45.2%) hips, the second revision in nine (29.0%) hips, the third revision in five (16.1%) hips, and the fourth revision in three (9.7%) hips. The indications for revision surgery were aseptic loosening THA in 25 (80.6%) hips and septic loosening in the other six (19.4%) hips. The severity of the acetabular deficiency was determined by preoperative radiographs of the hip and by intraoperative findings such as Paprosky IIIA defects (n = 17) and Paprosky IIIB defects (n = 12), and PD (based on AAOS classification; n = 2; Table 1). Six hips had concomitant femoral component revision secondary to loosening at the index procedure (n = 3) or removal of stem during previous periprosthetic infection (n = 3). This study was approved by the Institutional Review Board (103-6484B) of Chang Gung Memorial Hospital and is regarded as a retrospective review. All patients had complete follow up with a mean of 5.5 years (range, 3.0–10.5 years).
| Age (y) | 59 ± 11 (range, 37–79) | |
| Sex a | ||
| Male | 11 | |
| Female | 18 | |
| Initial diagnosis | Osteoarthritis | 12 (38.7) |
| Avascular necrosis | 8 (25.8) | |
| Postradiation osteonecrosis | 2 (6.5) | |
| Post-traumatic osteonecrosis | 4 (12.9) | |
| Rheumatoid arthritis | 1 (3.2) | |
| Ankylosing spondylitis | 1 (3.2) | |
| Tuberculosis | 2 (6.5) | |
| Tumor (PVNS) | 1 (3.2) | |
| Interval from the primary surgery to revision (y) | 14.1 ± 6.2 (0.8–25.8) | |
| Indications | Aseptic loosening of the cup only | 21 (67.7) |
| Aseptic loosening of both components | 3 (9.7) | |
| Periprosthetic joint infection | 5 (16.1) | |
| Postradiation acetabulum osteonecrosis | 2 (6.5) | |
| Severity of acetabular defect | Paprosky IIIA | 17 (54.8) |
| Paprosky IIIB | 12 (38.7) | |
| Pelvic discontinuity | 2 (6.5) | |
| Average follow up period (y) | 5.5 (3–10.5) | |
- Data are presented as n (%), mean ± SD (range), or n (range). PVNS = pigmented villonodular synovitis; SD = standard deviation.
- a One male and one female patient received consecutive bilateral revision surgery in this cohort. The male patient was diagnosed as having avascular necrosis of the bilateral femoral head, whereas the female patient had postradiation osteonecrosis of the acetabulum and femoral heads after radiotherapy for cervical cancer.
Surgical techniques
A posterolateral approach of the hip was performed in all patients. The failed acetabular component was removed first and the acetabular bed was thoroughly debrided until achieving healthy and bleeding bone beds. The acetabular bone defect was carefully inspected and recorded for the Paprosky classification [15].
For all hips, structural allografts were obtained from the distal femur or femoral heads and stockpiled in a deep frozen atmosphere at −75°C. After adequate shaping and sizing, the grafts were fit to cover the major-column defect of the acetabulum. The allograft, usually a femoral head allograft, was fixed to the acetabular defect with two to three 3.5-mm cancellous screws (Figure 1). For the two hips with PD, a distal femoral allograft was used that was performed in a “Figure 7” shape, as described by Paprosky et al [17].
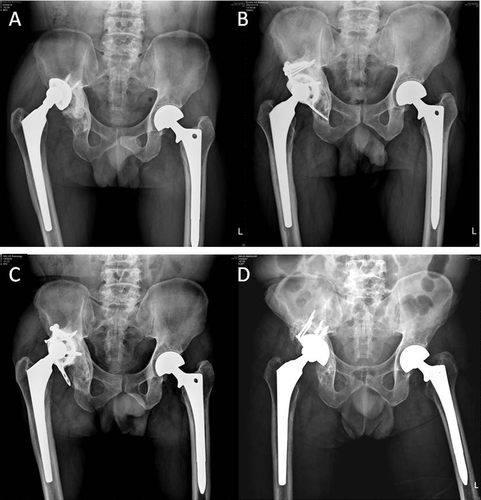
(A) A 52-year-old man presented with aseptic loosening of right total hip arthroplasty. Operative findings showed Paprosky type IIIA acetabular deficiency with a 7 cm × 5 cm superoposterior wall defect. (B) After reconstruction, radiography shows partial consolidation of the allograft and restoration of the bone stock at the 1-year follow up. (C) However, because of inadequate medialization of the cage, it moved to a higher position and loosened with the collapse of the superior structural allograft at 6.5-years after the index reconstruction. (D) The failed cage and residual small contained defect were treated with noncemented primary acetabular component, morselized allografts, and a small structural allograft. There was no measurable migration or displacement of the acetabular component at the 28-month follow up.
The acetabular bed was further reamed to an optimal size. The appropriate antiprotrusio Burch–Schneider cage (Braun; Aesculap, Tuttlingen, Germany) was prebent to fit the socket. The ischial flange was slotted into the obturator space with or without screw fixation. The iliac flange was placed on the lateral aspect of the ilium and fixed with two to four 6.5-mm titanium screws (Figure 1). The cage and host bone interface was further impacted with morselized allografts through the holes over the cage. The polyethylene liner was fixed on the cage using polymethylmethacrylate (PMMA) cement in a position of 35–45° inclination and 20–35° anteversion (Figure 1).
Femoral revision was selected for six patients who had loosening of both components. The size of the femoral head varied patient by patient to fit the brand of the original femoral component, which was not revised. The size of the femoral head was 26 mm in two (6.5%) hips, 28 mm in 14 (45.2%) hips, 32 mm in 14 (45.2%) hips, and 36 mm in one (3.2%) hip. The size of the cage was 64 mm in one hip, 62 mm in one hip, 58 mm in five hips, 56 mm in one hip, 54 mm in one hip, 52 mm in 19 hips, and 50 mm in two hips.
Postoperative care
For 3 days postoperatively, cefazolin (1 g every 8 hours) was administered intravenously. Three days after the procedure, ambulation was allowed with partial weight-bearing with the patient wearing an abduction brace. Full weight-bearing was not allowed until there was radiographic evidence of graft healing. All patients returned postoperatively for follow up at 1 month, 3 months, 6 months, 9 months, and 12 months.
Clinical evaluation
The grading of pain and walking ability were routinely recorded. The modified Harris hip scores [18] and Western Ontario McMaster University Arthritis Index (WOMAC) [19] were calculated preoperatively and on follow up. All complications were recorded such as superficial wound infection, deep infection, vesicle–acetabulum fistula, neurovascular injury, loosening of the components, and dislocations.
Radiographic evaluation
All patients had radiographic examinations using anteroposterior and lateral radiographic views. Rather than resorting to a histologic study, graft healing was determined when the plain film presented visible trabecular bridging of the host–donor interface, integration of fragments, and radiolucent line (i.e., remodeling) [20], [21].
Antiprotrusio cage loosening was defined by Gill et al [22], who described definite cage loosening as screw breakage, acetabular migration of > 5 mm, or progressive radiolucent lines at the cage-bone interface medially and superiorly or around the screws. The failure of the cage construct was defined as cage loosening, mechanical failure, and any reason for re-revision surgery.
Statistical analysis
Differences between the pre- and postoperative scores were evaluated with the Wilcoxon signed ranks test for paired samples. The endpoints for failure rate analysis were failure of the cage construct or until the last follow up. The failure rate of cage with various revision times were compared with Pearson's Chi-square test. The 5- and 10-year survival of the prosthesis and periacetabular allograft was calculated using the Kaplan–Meier survivorship curve with 95% confidence intervals [23]. All reported p values were two-tailed and statistical significance was set at p < 0.05. All statistical analyses were conducted using the SPSS 5.0 version (SPSS Inc., Chicago, IL, USA).
Results
The mean Harris hip score improved from 30 points (range, 7–54 points) preoperatively to 67 points (range, 16–91 points) at the time of the latest examination (p < 0.001). The mean preoperative WOMAC index value improved from 65 points (range, 14–93) preoperatively to 32 points (range, 11–48) at the latest follow up (p < 0.001; Table 2).
| Preoperative | Postoperative | p | |
|---|---|---|---|
| Modified HHS (points) | 30 ± 10 (7–54) | 67 ± 23 (16–97) | <0.001 |
| WOMAC hip index | 65 ± 20 (14–93) | 32 ± 9 (11–48) | <0.001 |
- Data are presented as mean ± SD (range). HHS = Harris hip score; SD = standard deviation; WOMAC = Western Ontario and McMaster Universities Arthritis Index.
Evidence of allograft consolidation and bony incorporation occurred in 27 (87.1%) hips with a healing time of 11.1 months (range, 4–40 months). Among four hips with nonunion of the grafts, one hip had recurrent infections and severe allograft resorption; one hip had an antiprotrusio cage with mechanical loosening and a re-revision was therefore deferred; and two hips in one patient had postradiation necrosis of the acetabulum.
Based on the Gill classification [22], six (19.4%) hips showed definite loosening of the Burch–Schneider cages at the latest follow up. Three of these hips had broken iliac screws. Acetabular component migration occurred in all six hips. No breakage of the Burch–Schneider cage was observed.
Seven (22.6%) cages were considered a treatment failure. The causes of failed cages were uncontrolled deep infection in one hip; nonhealing allograft, followed by moderate-to-severe resorption in three hips; cage loosening with complete allograft consolidation in two hips, and intractable painful leg length discrepancy in one hip.
At the time of review, six (19.4%) hips had undergone reoperation. However, one patient refused further surgical treatment because of low physical demand and surgical risks. Two cages were removed because of subsequent septic hip after cage loosening, and one hip had successful cage revision and structural bone grafts after the infection was controlled. The last three hips had a failed reconstruction cage and small contained defect after partial consolidation of the previous structural allograft; they were treated with a noncemented primary acetabular component and morselized allografts. At the follow up at 14 months, 16 months, and 28 months (average follow up of 19.3 months), the radiographs of the three hips confirmed that no hip had any measurable migration or displacement of the acetabular component (Figure 1). The average Harris hip score improved from 40.7 points to 78 points after the re-revision of a primary acetabulum component.
The failure rate of the cages was 21.4% (3/14 hips) in the first revision, 22.2% (2/9 hips) in the second revision, 0% (0/5 hips) in the third revision, and 66.7% (2/3 hips) in the fourth revision. The failure rate of the cage was not significantly associated with the revision time (p = 0.089). There was no significant increase in the failure rate in the fourth revision group, compared to the groups that underwent three revisions or fewer (p = 0.055; Table 3).
| Revision times | N | Average follow up period (y) | Failure rate * |
|---|---|---|---|
| 1st revision | 14 | 5.15 | 21.4 (3/14) |
| 2nd revision | 9 | 6.10 | 22.2 (2/9) |
| 3rd revision | 5 | 6.03 | 0 (0/5) |
| 4th revision | 3 | 4.41 | 66.7 (2/3) |
- Data are presented as % (n/N) unless otherwise indicated. * The cage failure rate is not significantly correlated with the revision time (p = 0.089). In addition, there is no increased failure rate in the fourth revision, compared to the failure rate with three revisions or fewer (p = 0.055).
Statistical analysis and implant survival
The endpoint was radiographic evidence of definite loosening of the acetabular component or any reason for re-revision. Kaplan–Meier survival analysis [22] revealed a 5- and 10-year survival of 76% (95% CI, 67.4%–84.6%) and 57% (95% CI, 39.3%–74.7%), respectively (Figure 2).
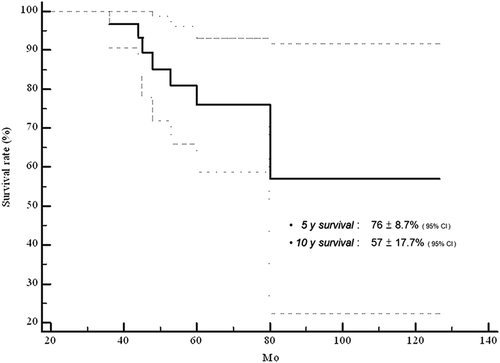
The Kaplan–Meier survivorship curves with the corresponding 95% confidence intervals for the following endpoints: radiographic cage loosening, mechanical failure, or any reason for re-revision surgery. CI = confidence interval.
Other complications
No patient experienced an immediate medical complication during hospitalization. Three (9.4%) hips in which relatively smaller heads were used (26 mm in 2 hips and 28 mm in 1 hip) had recurrent dislocations after surgery. All three hips were treated with abduction orthosis. One hip needed a revision to a larger head (range, 28–32 mm). One hip postoperatively sustained sciatic nerve impingement by the cage. It later required trimming of the cage margin and neurolysis of the sciatic nerve.
There was postoperative acute deep infection in a patient without a history of previous infection. No recurrent infection occurred until the recent follow up at 70 months. Two recurrent deep infections developed > 1 year postoperatively; one cage was removed because of uncontrolled infection and one cage was preserved after successful debridement and antibiotic therapy.
A 52-year-old female initially diagnosed as having postradiation osteonecrosis of the acetabulum and femoral head due to cervical cancer treatment had failed bilateral primary THA and progressive acetabular bone loss. After reconstruction surgery, the cages became loose in the 4th year on the left side and in the 5th year on the right side because of failed allograft incorporation. Furthermore, unresolved deep infection occurred several months later and vesico-acetabular fistula of the left hip was confirmed by intravenous pyelogram. This rare complication may occur because of progressive migration of the ischial flange and consecutive stress toward the bladder.
In total, complications occurred in 15 (48%) of 31 hips (Table 4).
| N | Portion (%) | |
|---|---|---|
| Cage loosening | 6 | 19.4 |
| Recurrent dislocation | 3 | 9.7 |
| Postoperation acute infection | 1 | 3.2 |
| Recurrent deep infection | 2 | 6.4 |
| Sciatic nerve impingement | 1 | 3.2 |
| Leg lengthening | 1 | 3.2 |
| Vesicle–acetabular vistula a | 1 | 3.2 |
| Total | 15 | 48.4 |
- a Vesicle–acetabular vistula developed in a cage with mechanical failure without evidence of a previous infection.
Discussion
There are various types of metal reinforcement rings used in the reconstruction of severe acetabular deficiency. The early Müller type ring only provides proximal fixation [24], whereas other devices provide dual fixation such as the Ganz [25] or Kerboull [26] rings, which uses a hook. The Burch–Schneider cage uses screws for distal fixation. Gerber et al [27] reported their experience with using the Ganz reinforcement ring and concluded that the lack of primary stability was the main cause of later graft failure and loosening of the reconstruction.
The Burch–Schneider cage offers stable proximal fixation of the ring to the ilium and distal fixation of the ischium with screws [22], [25], [28], [29]. Bonnomet et al [30] reported better results with the Burch–Schneider cage than with the Müller ring in patients with severe acetabular bone loss, and an 89.5% success rate in 57 patients who were followed 5–21 years. The current study demonstrates improved clinical outcomes with this procedure in 31 hips with severe acetabular deficiency with a mean follow up of 5.5 years.
However, there was a substantial rate of cage migration and aseptic loosening of the Burch–Schneider cage in patients with severe cranial or posterior wall defect of the acetabulum [31]. Goodman et al [32] reported a success rate of 76 and that cage-related complications were six neuropathies, four loose rings, three fractured flanges, three loose cups, seven dislocations, and three deep infections in 61 Burch–Schneider cages. The average follow up was 4.6 years. Forty-eight cages required structural allograft reconstruction because of a large (> 50%) uncontained acetabular defects or pelvic dissociation. However, there was no mention of the relationship between cage failure and the severity of the acetabular defect. They instead suggested a constrained acetabular liner to avoid dislocation, protection of the sciatic nerve, and slotting of the ischial flange into bone.
In the present study, the cage failure rate was 22.6% (7/31 hips). Six cage failures (19.4%) were associated with cage loosening or migration with bone resorption. This finding was similar to other reports of the use of Burch–Schneider cage and structural allografts [31]-[35]. The last patient who received the re-revision procedure did so because of painful leg lengthening after cage reconstruction rather than because of loosening. The survival analysis revealed 5- and 10-year survival rates of 76% (95% CI, 67.4–84.6%) and 57% (95% CI, 39.3–74%), respectively. This result is slightly less than the rate in other reports that included Paprosky type II defects. Philippe et al [36] reported a 14-year survival rate of 77.9%, which included patients with a Paprosky type II contained acetabular defect; by contrast, Symeonides et al [34] reported a 14-year survival rate of 61.75% in their series that included AAOS cavitary defect (i.e., type II).
Furthermore, there is little investigation on the relationship between the failure rate and the various revision times because the reason for failure is multifactorial. In the present study, a trend of increasing rate of failed reconstruction occurred in the fourth revision group, compared to the groups with three revisions or fewer (p = 0.055). The failure modes included cage loosening with complete allograft consolidation in one patient and nonhealing allograft in one patient. However, structural allograft achieved solid consolidation in two (66.7%) of three hips, which revealed that the host bed was still viable for healing the grafts, even after numerous surgical procedures.
Our study had some limitations: a small number of patients and possible reporting bias. More cases are necessary to illustrate whether reconstruction tend to fail after more revision times.
Dislocation is another complication after cage reconstruction. Udomkiat et al [37] reported a dislocation rate of 23% after metal ring reconstruction, and Goodman et al [32] reported a 12% dislocation rate in 61 cases after Burch–Schneider cage reconstruction. The following were considered: a weak abductor mechanism (including weakness of the gluteus medium by an extensive surgical procedure that may injure the superior gluteal nerve), nonunion of the trochanter, and vertical abduction angle of the cup [37]. A constrained cemented cup was suggested in selected cases [32], [37]. In the current study, three (9.7%) hips had recurrent hip dislocation, which was associated with a smaller femoral head (26 mm and 28 mm) and poor compliance of wearing the abduction orthosis postoperatively. Two hips were successfully managed with conservative treatment by using abduction orthosis, whereas a third hip required a revision to a larger head. No further dislocation was noted at the last follow up. To reduce the dislocation rate, using a larger femoral head (≥ 32 mm) and wearing an abduction brace orthosis are recommended for patients with cage reconstruction surgery.
The selection of morselized or structural allografts and a reinforcement ring for revision THAs is debatable. Some authors considered the Burch–Schneider cage to bridge the ilium and ischium and protect the bone grafts from resorption by excessive mechanical forces. Investigators have reported favorable results with morselized autografts or allografts [13], [34], [36]. However, if there is ≥ 40% segmental loss of the superior bone, the cancellous allografts are too weak to support acetabular ring reconstructions [14], [25]. Most reports that used morselized bone grafts and cage reinforcement and showed promising results had patients with mixed cavitary and combined acetabular defects [34], [36]. Perka and Lugwig [31] investigated the radiologic migration of the Burch–Schneider cage and revealed that posterior column defects were associated with a higher rate of aseptic loosening, cranial defects had a higher migration rate, and medial or anterior column defects had lower rates of migration and loosening. Superior migration of the cage could lead to loosening [22]. Thus, the Burch–Schneider cage in the absence of structural allograft is not recommended for significant combined superior and posterior column defects [14].
A structural allograft can be used for reconstruction of a superior acetabular defect to avoid a high hip center and improve leg length discrepancy [11], [27]. However, a certain percentage of cage reconstruction failure was still noted long-term because a smooth chrome–cobalt surface and osseous integration of the implant is not possible [31]. Goodman et al [32] report that their four cases of cage failure had partial healing of the graft after structural allograft reconstruction, which were considered sufficient bone stock for further revision. In a study of re-revision for failed cages or rings for uncontained defects of the acetabulum, Abolghasemian et al [38] reported 17 (34%) hips with re-revision surgery using a simple acetabular component without grafts or metal rings because of restored bone stock. In the current series, three (9.7%) hips had a re-revision procedure with a standard noncemented acetabular component after the index procedure in an average of 58 months. At the re-revision surgery, consolidation with partial re-vascularization of the allografts was confirmed in all three hips.
In conclusion, the Burch–Schneider antiprotrusio cage and structural allograft reconstruction for a complex acetabular defect is a technique-demanding procedure with a high complication rate. This study showed a 76% survival rate in 5 years. Even with failed cases, successful re-revision surgery with a noncemented acetabular component is feasible because of a healed allograft.
Acknowledgments
We thank Ms. Ya-Ju Yang for assistance with the statistical analysis.




