Sinonasal inverted papilloma with intracranial extension
Dear Editor,
Inverted papilloma is a benign epithelial tumor with locally aggressive behavior, with the potential for malignant transformation into squamous cell carcinoma at a rate of around 10% [1]. The most common presenting symptom of an inverted papilloma is unilateral nasal obstruction, followed by rhinorrhea and epistaxis. Not much is known about the etiology of this tumor; however, allergy, human papilloma virus, chronic rhinosinusitis, environmental carcinogens, and tobacco smoking have been implicated.
An 89-year-old female patient with type 2 diabetes mellitus, hypertension, left-sided breast cancer, and uterine cancer came to our emergency room due to the sudden onset of convulsions and lower limb weakness. She had a history of nasal inverted papilloma managed by endoscopic operation more than 10 years ago. Brain computed tomography was performed, which revealed a tumor arising from her frontal and ethmoid sinuses. Magnetic resonance imaging was arranged 2 days after admission, and frontal lobe invasion was noted (Fig. 1). Under nasal endoscopy, a granulomatous mass arising from the right ethmoid sinus was found. A biopsy was performed, and the pathology showed the presence of an inverted papilloma with cellular atypia. Immunohistochemical stains revealed that the lesion were weakly positive for Ki-67. Considering the patient's age and general condition, conservative treatment with anticonvulsants was adopted with complete remission of the major neurological symptoms.
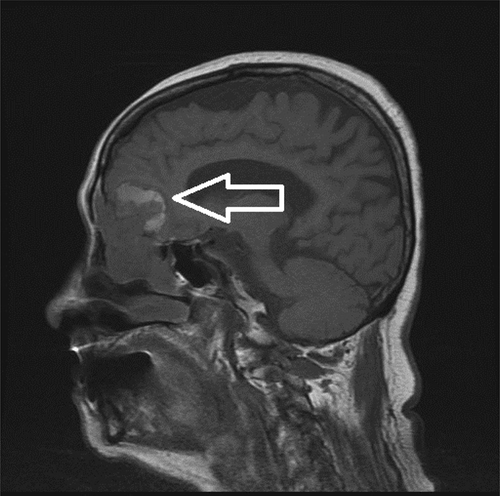
Tumor arising from the right frontal and ethmoid sinuses with frontal lobe invasion (arrow) is revealed by magnetic resonance imaging.
Inverted papilloma arises most frequently from the lateral nasal wall and ethmoid and maxillary sinuses. The tumor extends outside the nasal cavity in 7% of cases, and sometimes into the nasopharynx and the pterygopalatine and intracranial fossae. Intracranial extensions are rare. In the study by Miller et al. [2], 1469 cases were reviewed and only five cases demonstrated extension into the anterior cranial fossa. Inverted papilloma with intracranial extension is usually seen in recurrent cases, and this is especially true if the lesion affects the cribriform plate, fovea ethmoidalis, or orbits [3]. In a recent report by Visvanathan et al. [4], the authors claimed to have reported the first case of an inverted papilloma presenting with sudden neurological deterioration. Nevertheless, with the same sudden neurologic symptoms, no frontal sinus mucoceles were found in our case. Interestingly, many reported cases of intracranial extensions of inverted papillomas have experienced some typical neurological symptoms [2]. Taking our case into consideration, it is possible that even without the development of a mucocele, sudden neurological deterioration may occur.
Currently, it is widely accepted that extradural intracranial disease should be treated with radical excision, which usually requires a craniofacial approach [3]. However, dural invasion of inverted papillomas is associated with a decreased survival rate, regardless of the method of treatment. Chen et al. [5] found that the correct diagnosis prior to surgery is a determinant of outcome. The authors even recommended that using frozen sections may improve outcome. In conclusion, especially in recurrent cases, clinicians should be aware of the intracranial extensions of inverted papillomas, even if the patient appears to not have symptoms.




