Prevalence and associated factors of early repolarization pattern in healthy young northeastern Thai men: A correlation study with Brugada electrocardiography
Abstract
Background
Early repolarization pattern (ERP) is characterized by J-point elevation with QRS notching or slurring in the terminal portion of the QRS complex. It may be associated with sudden death. Brugada syndrome (BS) is a genetic and fatal disease commonly found in northeastern Thai men. Data on the rate and predictors of ERP in Asian populations are limited. In addition, the correlation between ERP and BS has never been studied in an endemic area of BS. This study aimed to evaluate the prevalence of ERP and its associated factors in young, healthy male Asian subjects.
Methods
Between June 2011 and May 2012, 282 young, healthy men aged 20–45 years were enrolled at check-up clinics in Khon Kaen, Thailand. Subjects were divided into the ERP and non-ERP groups.
Results
There were 29 subjects with ERP (10.3%). The Sokolow–Lyon index was an independent factor for ERP with an adjusted odds ratio of 1.090 (95% CI: 1.027, 1.159). The Brugada ECG pattern was found in 11 (37.9%) subjects in the ERP group. The Brugada ECG pattern (non-type 1) was commonly found in lateral ERP patients. After the placement of high intercostal leads, the Brugada ECG pattern was dramatically increased compared with results obtained during standard ECG lead placement.
Conclusions
The ERP rate in young, healthy men from northeastern Thailand was 10.3%. A higher Sokolow–Lyon index was the only independent factor associated with ERP. Subjects with ERP should be examined with high intercostal leads to uncover Brugada ECG.
1 Introduction
Early repolarization pattern (ERP) is characterized by an elevation greater than 0.1 mV of the junction between the end of the QRS complex and the beginning of the ST segment (J point) and notching or slurring of the terminal portion of the QRS complex followed by a positive T wave [1].
The prevalence of ERP is 1–2% in the normal population. The condition is more commonly seen in young individuals, especially those predisposed to vagotonia, and in men. ERP is also frequently observed in athletes, cocaine users, and patients with hypertrophic obstructive cardiomyopathy [2]. The prevalence of ERP is as high as 10% in athletes, especially in high endurance athletes [3].
Over the last decade, evidence has mounted regarding the potential role of ERP in life-threatening arrhythmias and sudden unexplained deaths [4]. Several reports suggested that such arrhythmias are associated with ERP in the inferior or mid- to lateral precordial leads. ERP has recently been associated with vulnerability to ventricular fibrillation in independent case-controlled studies [5]. Clinical interest in ERP has been rekindled because of its similarities to Brugada syndrome (BS) [1].
Several studies attempted to demonstrate an association between ERP and BS, but much remains unknown [6]. BS is highly prevalent in the northeast region of Thailand and in Japan [7]-[9]. The use of high intercostal leads is a more sensitive method for the detection of the Brugada ECG pattern [7]-[9]. Little is known about the frequency and predictors of ERP in Asian populations. In addition, the correlation between ERP and Brugada ECG has never been studied in an area endemic for BS. The aim of this study was to examine the prevalence and predictors of ERP in young healthy Thai males in northeastern Thailand. The association between ERP and Brugada ECG in Thailand was also studied.
2 Materials and methods
2.1 Study population
The study population included healthy male subjects between 20 and 45 years of age from the Health Check-Up Clinic at Srinagarind Hospital, Khon Kaen University, Thailand, and from the health check-up medical services at factories and military training camps. Enrolled subjects showed sinus rhythm on a 12-lead standard ECG. The study took place between June 2011 and May 2012. The exclusion criteria were any comorbid diseases; a history of cardiac arrhythmias or cardiac syncope/arrest; taking any medications associated with electrocardiographic ST-T changes (e.g., beta-blockers, sodium channel blockers, beta-adrenergic agonists, sympathetic stimulants); and abnormal ECG findings including complete right bundle branch block, left bundle branch block, ventricular pre-excitation, atrial fibrillation, atrial flutter, and premature ventricular contraction.
2.2 Electrocardiographic measurement
After obtaining informed consent, all subjects underwent 12-lead standard ECGs with digital filters in the supine position. A paper speed of 25 mm/s and a calibration of 20 mm/mV were used for a more precise reading, and data were stored electronically for further analysis. ECG recording was performed by experienced cardiac nurses. After the standard ECG recordings, 6 high intercostal leads were obtained: −V1, −V2, −V3, −2V1, −2V2, −2V3. The −V1, −V2, and −V3 leads were placed at the third right intercostal space (ICS), the third left ICS, and one ICS above the location of the standard V3 lead, respectively [7]. The −2V1, −2V2, and −2V3 leads were placed at the second right ICS, second left ICS, and two ICSs above the location of the standard V3 lead, respectively (Table 1). All ECG recordings were evaluated by three independent reviewers. Diagnoses of ERP and the Brugada ECG pattern were made when there was agreement between at least two of the three investigators regarding the classification of these ECG abnormalities.
| Methods | V1 | V2 | −V1 | −V2 | −V3 | −2V1 | −2V2 | −2V3 |
|---|---|---|---|---|---|---|---|---|
| Standard placement | 4th ICS right | 4th ICS left | NA | NA | NA | NA | NA | NA |
| High intercostal leads | NA | NA | 3rd ICS right | 3rd ICS left | One ICS above standard V3 | 2nd ICS right | 2nd ICS left | Two ICS above standard V3 |
- NA: not applicable; ICS: intercostal space.
We measured the R wave in V5/6 and the S wave in V1 (Sokolow–Lyon index, mV) on the standard ECG. Other ECG parameters included heart rate, QRS duration, and QTc duration. The presence or absence of an ERP pattern in the inferior/lateral leads was assessed. The J-point elevation and ST-segment elevation 80 ms after the J point in the inferior/lateral leads were measured from the upper leading edge. If there were two possible J points, the second was used. Only V1 and V2 were used to evaluate the presence or absence of the Brugada ECG pattern, which was then classified as type 1 or non-type 1. In the high intercostal ECGs, the presence or absence of a Brugada ECG pattern was also assessed and similarly classified.
2.3 Definition of ERP and Brugada ECG
ERP was defined as: (1) a prominent notch or slur on the down-sloping portion of the QRS complex, known as a J-deflection, and a J-point elevation ≥0.1 mV; (2) a diffuse upward ST-segment concavity concordant with the QRS complex and a positive T wave in the same lead; and (3) at least 2 consecutive inferior (II, III, aVF) or lateral (I, aVL and V4–6) leads [1]. Cases were classified according to the location of the ERP-positive lead as inferior, lateral, or both. Examples of ERP at the inferior leads are shown in Fig. 1, and a Brugada ECG type 1 in the high intercostal leads is shown in Fig. 2.
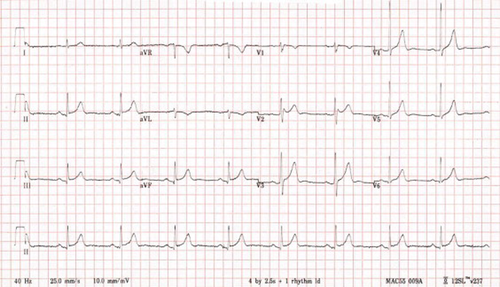
Early repolarization pattern >0.1mV in two inferior leads (III and aVF).
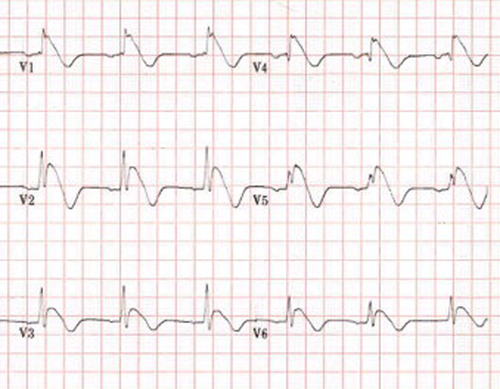
Significant coved-type ST elevation at all six high intercostal leads (−V1, −V2, −V3, −2V1, −2V2, and −2V3) compatible with a type 1 Brugada ECG pattern. The leads shown in the figure corresponded to the six high intercostals leads mentioned above. The ECG was run with a paper speed of 25mm/s and calibration of 10mm/mV.
Brugada ECG patterns were classified as type 1 and non-type 1, as shown in 3, 4 [10]. The J-point elevation on a Brugada ECG must be greater than or equal to 0.2 mV [10].
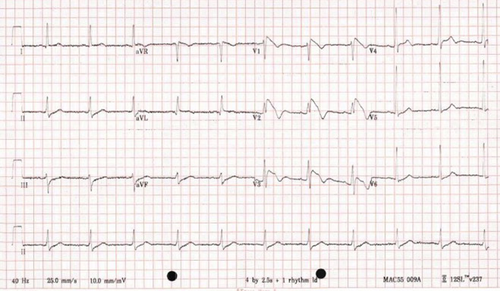
Typical type 1 Brugada ECG evidenced by prominent coved ST-segment elevation >2mm followed by a negative T wave at V1 and V2 [11].
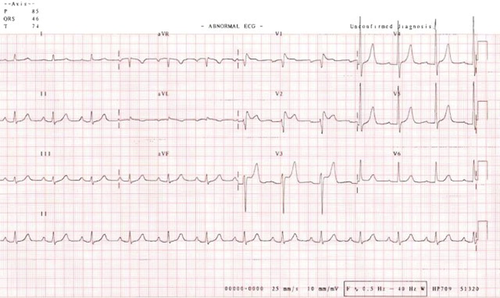
Non-type 1 Brugada ECG evidenced by a >2mm J-point elevation, a >1mm ST segment elevation, and a saddleback appearance followed by a positive T wave at V1 and V2 [11].
2.4 Statistical analysis
Data were expressed as the mean (standard deviation) or percentage (%). Subjects were divided into two groups: those with a J-point elevation ≥0.1 mV and those with a J-point elevation <0.1 mV or absent. Differences between these two groups were compared. Significant clinical factors were included in a multivariate logistic regression analysis to identify independent factors associated with having a J-point elevation greater than or equal to 0.1 mV. Analytical results are presented in terms of crude odds ratios, adjusted odds ratios, their 95% confidence intervals, and p-values. A subgroup analysis was also performed to compare clinical factors between cases with a J-point elevation ≥0.1 mV and those with a J-point elevation <0.1 mV. Statistically significant differences between means and proportions were tested by descriptive statistics, and a p-value <0.05 was considered statistically significant.
2.5 Ethical approval
The study complied with the Helsinki Declaration and was reviewed and approved by the Khon Kaen University Human Research Ethics Committee (HE#541040, approved on May 9, 2011).
3 Results
During the study period, 322 healthy male volunteers were enrolled. Of those, 40 were excluded due to high blood pressure (n=32), a history of syncope (n=2), an age over 45 years (n=1), premature ventricular contraction (n=2), Wolff–Parkinson White syndrome (n=1), atrial fibrillation (n=1), and complete right bundle branch block (n=1). Of the 282 subjects ultimately included in the analysis, 29 (10.3%) had ERP.
Subjects with ERP had a significantly lower body weight and body mass index (BMI), lower systolic blood pressure, lower diastolic blood pressure, a slower heart rate, a shorter QTc duration, and a higher Sokolow–Lyon index than those without ERP (Table 2). All 6 significant factors were included in the multivariate logistic analysis for ERP. Only the Sokolow–Lyon index was an independent factor for ERP, with an adjusted odds ratio of 1.090 (95% confidence interval: 1.027, 1.159), as shown in Table 3.
| Features | No or J-point elevation <0.1mV N=253 | J-point elevation >0.1mV N=29 | p-Value |
|---|---|---|---|
| Age, years | 28.1 (8.7) | 25.4 (8.1) | 0.069 |
| Weight, kg | 65.0 (12.2) | 60.3 (8.8) | 0.037 |
| Height, cm | 169.5 (5.7) | 170.0 (6.1) | 0.727 |
| Body mass index, kg/m2 | 22.7 (4.1) | 20.9 (3.0) | 0.008 |
| Systolic blood pressure, mmHg | 115.9 (11.7) | 108.5 (11.3) | 0.004 |
| Diastolic blood pressure, mmHg | 72.4 (9.0) | 68.5 (6.5) | 0.009 |
| Heart rate, bpm | 64.8 (13.6) | 56.4 (10.6) | 0.001 |
| QTc duration, ms | 406.3 (27.3) | 391.8 (29.3) | 0.004 |
| QRS duration, ms | 93.3 (10.0) | 92.2 (9.5) | 0.597 |
| Sokolow–Lyon index, mV | 2.5 (0.7) | 2.9 (0.8) | 0.005 |
| Family history of SUD, % | 14.0 (5.8) | 0 | 0.374 |
- SUD: sudden unexplained death; data presented as mean (standard deviation) or number (percentage).
| Variables | Univariate odds ratio (95% confidence interval); p-value | Adjusted odds ratio (95% confidence interval); p-value |
|---|---|---|
| Age | 0.959 (0.909, 1.011); 0.122 | 1.031 (0.954, 1.114); 0.441 |
| Body mass index | 0.845 (0.729, 0.978); 0.024 | 0.933 (0.792, 1.098); 0.405 |
| Systolic blood pressure | 0.945 (0.910, 0.981); 0.003 | 0.956 (0.902, 1.022); 0.121 |
| Diastolic blood pressure | 0.959 (0.920, 0.999); 0.046 | 1.005 (0.936, 1.080); 0.892 |
| Heart rate | 0.950 (0.920, 0.982); 0.002 | 0.968 (0.926, 1.013); 0.159 |
| Sokolow–Lyon index | 1.080 (1.022, 1.139); 0.005 | 1.090 (1.027, 1.159); 0.005 |
| QTc | 0.980 (0.965, 0.995); 0.009 | 0.993 (0.977, 1.010); 0.428 |
There were 129 subjects who had some J-point elevation. In 100 of these subjects (77.5%), the J-point elevation was <0.1 mV. The remaining subjects were those with ERP. These subjects had a significantly lower systolic blood pressure (mean of 108 vs. 114 mmHg) and a greater proportion of elevations detected by lateral leads (93.1% vs. 59%) (Table 4).
| Features | J-point elevation <0.1mV N=100 | J-point elevation >0.1mV N=29 | p-Value |
|---|---|---|---|
| Age, years | 26.2 (8.2) | 25.2 (7.9) | 0.561 |
| Weight, kg | 65 (15) | 60 (8) | 0.087 |
| Height, cm | 169 (5) | 170 (5) | 0.345 |
| Body mass index, kg/m2 | 22.7 (5.0) | 20.8 (2.9) | 0.053 |
| Systolic blood pressure, mmHg | 114 (13) | 108 (11) | 0.026 |
| Diastolic blood pressure, mmHg | 71 (12) | 69 (7) | 0.394 |
| Heart rate, bpm | 61 (11) | 57 (11) | 0.087 |
| QTc duration, ms | 400 (27) | 392 (29) | 0.170 |
| QRS duration, ms | 93 (10) | 91 (9) | 0.334 |
| Sokolow–Lyon index, mV | 2.7 (0.7) | 2.9 (0.7) | 0.178 |
| Family history of SUD, % | 5 (5) | 0 | 0.587 |
| Lead location | <0.001 | ||
| Inferior lead | 19 (19) | 1 (3.4) | |
| Lateral lead | 59 (59) | 27 (93.1) | |
| Inferolateral lead | 22 (22) | 1 (3.4) |
- SUD: sudden unexplained death; data presented as mean (standard deviation) or number (percentage).
The Brugada ECG pattern was found in 39 (39%) individuals with a J-point elevation <0.1 mV in the inferolateral leads and in 11 (37.9%) individuals with ERP (Table 5). Ninety percent of subjects in both groups exhibited a non-type 1 pattern. The Brugada ECG pattern was commonly found in lateral ERP. The associations between the locations and types of Brugada ECG pattern are shown in Table 6. Brugada ECG in ERP subjects mostly occurred in the lateral leads and was defined as non-type 1 (Table 6). After the placement of high intercostal leads in subjects with ERP, the frequency of Brugada ECG increased dramatically in those with and without ERP with particular increases in non-type 1 pattern subjects (Table 5).
| J-point elevation <0.1mV N=39 | J-point elevation ≥0.1mV N=11 | p-Value | |
|---|---|---|---|
| Standard leads | 12 (31%) | 2 (19%) | 0.705 |
| Type 1 | 3 | 0 | |
| Non-type 1 | 9 | 2 | |
| High intercostal leads | |||
| (−V1, −V2) | 36 (88%) | 11 (100%) | 0.573 |
| Type 1 | 1 | 1 | |
| Non-type 1 | 35 | 10 | |
| High intercostal leads | |||
| (−2V1, −2V2) | 39 | 11 | |
| Type 1 | 4 | 1 | |
| Non-type 1 | 35 | 10 |
| J point elevation <0.1mV (N=100) | J point elevation ≥0.1mV (N=29) | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Inferior (n=19) | Lateral (n=59) | Inferolateral (n=22) | Inferior (n=1) | Lateral (n=27) | Inferolateral (n=1) | ||
| Brugada ECG | 8 (43%) | 28 (48%) | 3 (14%) | 0 | 11 (41%) | 0 | 0.692 |
| Type 1 | 1 (6%) | 3 (5%) | 0 | 0 | 1 (4%) | 0 | 0.958 |
| Non-type 1 | 7 (37%) | 25 (43%) | 3 (14%) | 0 | 10 (37%) | 0 | 0.786 |
4 Discussion
The rate of ERP in young, healthy men in northeastern Thailand was 10.3%. This is higher than the rate reported in the US (3.3–6.1%) [12]. In the US report, the mean age of the study population was 45 years, which was older than the age of subjects in our study. Another report from the UK with a mean patient age of 25 years indicated an ERP prevalence of 15.2%, which is comparable with this study [13]. Thus, the prevalence of ERP may be high in younger subjects and low in older subjects.
Our ERP subjects differed significantly in a number of ways from those with a low or no J-point elevation. As also reported by others, ERP subjects had slower heart rates and shorter QTc durations [14] (Table 2). Other important factors in the univariate logistic analysis included body weight, BMI, systolic blood pressure, diastolic blood pressure, QTc duration, and the Sokolow–Lyon index. Lean subjects may have a high Sokolow–Lyon index. After adjusting for confounders and other factors, BMI was not an independent factor, while the Sokolow–Lyon index was the only independent risk factor for ERP, with an adjusted odds ratio of 1.090 (Table 3). A previous report also found that the Sokolow–Lyon index was a predictor of ERP [12]. Our study population differed from previous study populations in some important respects; our study enrolled only healthy subjects who were assumed to be at low risk of cardiac arrest by virtue of their age, while subjects in the Framingham and H2K studies had comorbidities, such as hypertension [12].
Most ERPs in this study were detected by lateral leads in young, healthy men that were considered to be at low risk for cardiac arrest [15]. Brugada ECG was found in 11 of 29 subjects in the ERP group (37.9%), mostly in the lateral leads of ERP ECGs. The Brugada ECG pattern was found in only 2 of these subjects (6.9%) using standard ECGs, and both had the non-type 1 pattern (Table 5). When high intercostal leads were used, the Brugada ECG pattern was found in 11 subjects (37.9%), most of whom had the non-type 1 pattern. The degrees and lead locations of type 1 Brugada ECG were comparable between subjects with ERP and subjects with a J-point elevation of less than 0.1 mV in the inferolateral leads (Tables 5 and 6).
In the present study, ERP was detected mostly by the lateral leads, and one-third of subjects showed the non-type 1 Brugada ECG pattern upon high ICS lead placement. Both lateral ERPs and non-type 1 Brugada ECGs are considered benign and have a low risk of sudden death [15]. These subjects, however, should be aware of developing the type 1 Brugada ECG pattern, which could increase the risk of a serious arrhythmia in subjects taking class 1 anti-arrhythmic agents or psychotropic drugs and in those with an electrolyte abnormality. In addition, these subjects may have a higher risk of developing BS in the future, and close follow-up as well as avoidance of modulating factors is recommended.
Genetic studies and drug-induced Brugada ECGs were not available for subjects in this study. This limitation may need to be explored in future studies to investigate genetic correlations with ERP as well as ECG changes induced by anti-arrhythmic medications. ERP may be inherited and may be associated with sudden death. This was a cross-sectional study with no data on long-term outcomes. ECGs in our study were performed in the daytime. Therefore, data on daily fluctuations and circadian variations of ERP were limited.
5 Conclusions
The ERP rate in young, healthy men in northeastern Thailand was 10.3%. A higher Sokolow–Lyon index was the only independent factor associated with having ERP. Subjects with ERP should be examined using high intercostal leads to uncover a possible Brugada ECG.
Conflict of interest
None declared.
Acknowledgments
This study was supported by TRF grants from the Senior Research Scholar Grant, Thailand Research Fund grant number RTA5580004, and the Higher Education Research Promotion and National Research University Project of Thailand, Office of the Higher Education Commission, Thailand, through the Health Cluster (SHeP-GMS), Khon Kaen University. The authors gratefully thank Prof. James A. Will (University of Wisconsin, USA) for his kind review of the manuscript.




