Cardiogenic shock after primary percutaneous coronary intervention: Effects of levosimendan compared with dobutamine on haemodynamics
Abstract
Background:
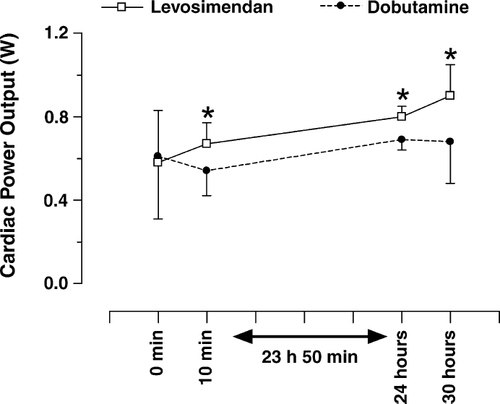
Levosimendan is a new calcium sensitizer with positive inotropic properties. Cardiac power output (CPO) has been shown to be instrumental in the diagnosis of cardiogenic shock (CS) and is an important determinant of outcomes.
Aims:
To evaluate the haemodynamic effects of levosimendan compared to dobutamine in acute myocardial infarction (AMI) patients revascularised by primary percutaneous coronary intervention (PCI), who developed CS.
Methods and results:
Twenty two consecutive AMI patients revascularised by PCI, who developed CS, were randomly assigned to levosimendan (24μg kg−1 bolus plus 24-h continuous infusion 0,1μg kg−1 min−1) or dobutamine (initial dose 5μg kg−1 min−1, with a maximum dose adjustment in order to reach the desired haemodynamic effect). Evaluations were performed from baseline to 30h. The primary end-point was an increase ≥30% in CPO, after 24h of therapy. The baseline clinical and haemodynamic characteristics were similar in both groups. Levosimendan had a consistently better effect on CPO than dobutamine, while the decrease in PCWP was similar.
Conclusion:
The primary objective of our study was achieved better by the end of the 24h infusion of levosimendan than by dobutamine.
1. Introduction
Cardiogenic shock (CS) is the main cause of death in patients hospitalised for acute myocardial infarction (AMI) 1. In patients with acute myocardial ischaemia requiring inotropic support, only a very limited number of pharmacological approaches are available: catecholamine and phosphodiesterase inhibitors improve contractility but they may have potentially deleterious effects because they increase myocardial energy consumption and underlying ischaemia, and they may even produce myocardial necrosis, cardiotoxicity and arrhythmia 2.
Levosimendan belongs to a new group of inotropic agents developed for cardiovascular therapy, which enhance the sensitivity of the myofilaments to calcium 3. Clinical studies, in healthy volunteers and in patients with decompensated heart failure (HF), have confirmed the positive inotropic, vasodilatory and haemodynamic properties of intravenous levosimendan 4567, which may explain the lower risk reported in previous studies of heart failure 5. These characteristics suggest that levosimendan might be beneficial in CS, especially when it complicates AMI 8.
Cardiac power (CPO), an indicator of cardiac contractility and ventricular-vascular coupling, represents the pumping power of the heart, i.e. the amount of energy from the heart available in the systemic vasculature to maintain vital organ perfusion. It is a novel haemodynamic measure, based on the classical physical laws of fluids (power=flow×pressure), where CPO is derived from the product of cardiac output and mean arterial pressure (MAP) 9. Tan et al. showed that the resting CPO for haemodynamically stable average sized adults is approximately 1W 10. However, during stress or exercise, the cardiac power reserve can be recruited to increase the heart's pumping ability up to 6W. Recent studies have shown that CPO is a significant predictor of short-term and long-term outcomes in patients with chronic and acute congestive HF and also in CS 11,12.
The purpose of the present study was to assess the acute haemodynamic effects, particularly on CPO, of intravenous levosimendan compared with intravenous dobutamine in patients with ST segment elevation myocardial infarction (STEMI), revascularised by primary percutaneous coronary intervention (PCI) and who subsequently developed CS secondary to severe left ventricular systolic dysfunction.
2. Patients and methods
2.1. Study patients
Between January 2003 and December 2004, 180 patients with STEMI were treated in our hospital with primary PCI. Twenty six of these patients (14%) developed CS secondary to severe left ventricular systolic dysfunction after primary PCI. CS was diagnosed according to published criteria 13. Of these 26 eligible patients, 4 were excluded as follows, sustained ventricular tachycardia (n=1), right ventricular infarction (n=2) and haemodynamically significant ischaemic mitral regurgitation (n=1). Exclusion criteria were: right ventricular infarction; cardiac tamponade; heart rate ≥120bpm; sustained ventricular tachycardia or ventricular fibrillation within the 2 previous weeks; ventricular septal rupture; haemodynamically significant mitral regurgitation; other haemodynamically significant valvular or congenital heart diseases; antecedents of heart failure; antecedents of myocardial infarction, cerebral stroke or other major hospitalisation within 3 months; use of inotropic, calcium antagonist or antiarrhythmic drugs, except digoxin, within the previous seven days; second- or third-degree atrioventricular block; adult respiratory distress syndrome or significant pulmonary disease; septic shock; body mass index ≥32kg/m2; end-stage renal failure; liver cirrhosis; enrollment in other studies within the previous six months; pregnancy; and clinically overt thyrotoxicosis.
The study followed the principles of the Declaration of Helsinki and of the World Medical Assembly. The protocol was approved by the institutional ethics board, and documented informed consent was obtained from each patient. This was a randomised, open-label, parallel group study. Patients were assigned to levosimendan or dobutamine treatment, in a 1:1 ratio.
2.2. Protocol
Each patient was monitored haemodynamically by percutaneous cannulation of the right internal jugular vein using a pulmonary artery Swan-Ganz thermodilution catheter. Arterial blood pressure was measured using an indwelling arterial catheter inserted into the radial artery. Baseline heart rate, MAP, mean pulmonary arterial pressure and pulmonary capillary wedge pressure (PCWP) were recorded at end expiration, three times within a 5min period using the bedside patient monitor. Measurements were made by two research team members who were blinded to treatment allocation. Values were similar, with a variance of less than 10%. Additional measurements were performed 10min and then 1, 4, 8, 12, 24 and 30h after the drug administration began.
Levosimendan treatment began with a loading dose given as an infusion of 24μg kg−1 over 10min, followed by a continuous infusion of 0.1μg kg−1 min−1. Dobutamine treatment began with a continuous infusion of 5μg kg−1 min−1, there was no loading dose. If an adequate response (defined as an increase in CPO of at least 30%) was not achieved after 2h, the infusion rate of dobutamine was doubled until the desired haemodynamic response was achieved. Infusions were maintained at a constant rate for 24h, unless dose-limiting events occurred or if the patient had a major cardiovascular event or serious adverse reaction. If any of the following dose-limiting events occurred: symptomatic hypotension; systolic blood pressure <75mm Hg; or tachycardia (heart rate>140bpm for at least 10min or increased by >25bpm) the infusion was interrupted for 30–60min or until the dose-limiting event had resolved.
2.3. Treatment regimens
All patients were recruited in the Coronary Care Unit. Once CS had been diagnosed, patients were randomised to receive either intravenous levosimendan or dobutamine. Additional medication (furosemide, sodium nitroprusside, nitroglycerine, digitalis) was administered at stable doses during the study.
Changes in hemodynamic variables from baseline to 30h were calculated for each patient, with measurements at 1, 4, 8, 12, 24, and 30h. The following measurements were available: cardiac output (CO) (L/min) and cardiac index (CI) (L/min m2), calculated by applying an adapted Fick's method standard formula with an oxygen consumption index calculated according to age, sex, and body surface area 14. CPO (W) was calculated as CO×MAP×K, where K is the conversion factor (K=2.22×10−3) 15. MAP (mm Hg) was calculated as [(Systolic blood pressure−diastolic blood pressure)/3]+diastolic blood pressure. Systemic vascular resistance (SVR) (dyn s/cm5) was calculated by the equation: 80×(MAP−Central Venous Pressure)/CO. Stroke work (SW) (g m) was calculated as (MAP−PCWC)×0.0136×stroke volume. SW index (g m/m2) was determined by SW/body surface area. Left Ventricular SW (kg m/min) was calculated as (MAP−PCWP)×CO×0.0136. Left Ventricular SW Index (kg m/minm2) was calculated as (MAP−PCWP)×CI×0.0136. Left ventricular ejection fraction (LVEF) was assessed by two-dimensional echocardiography using the biplane Simpson's rule 16. Echocardiograms were read in random order with no patient identifiers. The measurements of LVEF were made at baseline and 6h after withdrawal of the levosimendan or dobutamine infusion.
The prospectively defined primary objective was a 30% or greater increase in CPO, after 24h of therapy.
2.4. Statistical analyses
Data were statistically processed and analyzed using the SPSS 10.0.1 software package for PC (Analytical Software, Chicago, IL, USA). Descriptive statistics were presented as mean±Standard Deviation (SD) for continuous data and as percentages for categorical data. Fisher's exact test was used to compare all group proportions. Haemodynamic changes were compared before and after each treatment using unpaired Student's t-test. A p value≤0.05 was considered statistically significant.
3. Results
Twenty two patients, aged between 21 and 85 years, admitted to the Coronary Care Unit with STEMI, and who were successfully revascularised with a primary PCI procedure, developed CS within the following 24h. In all cases a TIMI 0–1 flow grade was present in the artery responsible for infarction (ARI) prior to PCI. Following PCI a TIMI flow grade 3 was re-established in the ARI, with residual stenosis of less than 30%. Sixteen patients had anterior localization and 6 patients had infero-lateral localization of STEMI. Eleven patients were assigned to treatment with levosimendan and 11 to dobutamine.
Baseline clinical and haemodynamic characteristics were similar between the treatment groups (Table 1). The time from onset of symptoms to first balloon inflation was similar for both groups (330min [SD±60] in the levosimendan group vs. 280min [SD±75] in the dobutamine group; p=0.09) as was the time from the start of the procedure to the opening of the vessel (30min [SD±12] in levosimendan group vs. 26min [SD±11] in dobutamine group; p=0.42). There was no significant difference in the percentage of stents implanted during PCI (levosimendan group 88% vs. dobutamine group 90%; p=0.34). None of the patients developed multiple organ failure. There were no re-infarctions or cerebrovascular accidents in either group. Baseline haemodynamic measurements were obtained once CS was diagnosed, and in all cases after performing PCI. The use of intra-aortic counterpulsation balloons (IABP) for the treatment of CS was at the discretion of the treating physician in each case. An IABP was only used in one case in the levosimendan treatment group.
| Levosimendan (n=11) | Dobutamine (n=11) | p value | |
|---|---|---|---|
| Age, years | 65±12 | 63±11 | 0.68 |
| Male (%) | 86 | 75 | 0.20 |
| Smokers (%) | 50 | 45 | 0.12 |
| Hypertension (%) | 31 | 35 | 0.29 |
| Diabetes mellitus (%) | 23 | 30 | 0.52 |
| Anterior location of infarct (%) | 85 | 64 | 0.06 |
| Artery responsible for the infarct | |||
| Anterior descending (%) | 85 | 64 | 0.06 |
| Circumflex (%) | 0 | 7.2 | 0.18 |
| Right coronary (%) | 15 | 28.8 | 0.07 |
| Multi-vessel disease (%) | 49 | 40 | 0.48 |
| CO (L/min) | 3.52±1.05 | 3.59±0.79 | 0.86 |
| CI (L/min m2) | 1.7±0.4 | 1.8±0.3 | 0.51 |
| PCWP (mm Hg) | 25±4 | 28±6 | 0.18 |
| MAP (mm Hg) | 75±8 | 77±9 | 0.58 |
| HR (bpm) | 85±16 | 86±12 | 0.87 |
| SVR (dyn s/cm5) | 1725±450 | 1690±350 | 0.84 |
| SW (g m) | 28.16±14.47 | 27.81±16.50 | 0.95 |
| SWI (g m/m2) | 16.37±8.30 | 16.16±9.25 | 0.95 |
| LVSW (kg m/min) | 2.393±1.41 | 2.392±1.47 | 0.99 |
| LVSWI (kg m/min m2) | 1.391±0.72 | 1.390±0.75 | 0.99 |
| CPO (W) | 0.58±0.25 | 0.61±0.30 | 0.80 |
- a Data are presented as mean value±SD.
- b CI = cardiac index; CO = cardiac output; CPO = cardiac power output; HR = heart rate; LVSW = left ventricular stroke work; LVSWI = left ventricular stroke work index; MAP = mean arterial pressure; PCWP = pulmonary capillary wedge pressure; SVR = systemic vascular resistance; SW = stroke work; SWI = stroke work index.
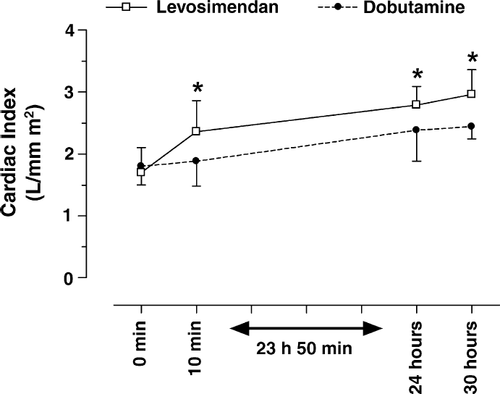
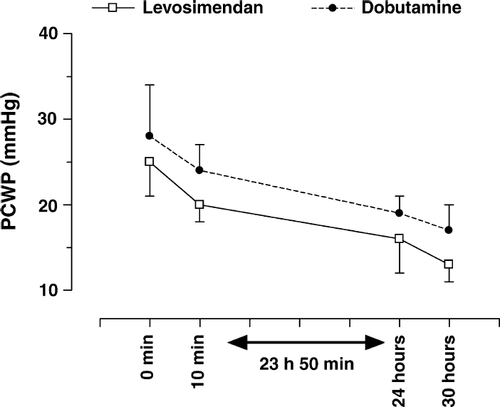
The effect on CI and CPO during the 24-h period of treatment was consistently better with levosimendan than with dobutamine (Figs. 1 and 2). After 24h of levosimendan infusion, PCWP decreased by about 25% compared to baseline. A similar decrease was observed in the dobutamine treatment group (Fig. 3).
Both levosimendan and dobutamine increased heart rate by a modest and similar amount (6.7bpm [SD±3.2] vs. 5.8bpm [SD±2.9]; p=0.49). No further change in systolic blood pressure was noted in either group and neither had serious side effects requiring early withdrawal of the study drug infusion.
There were no statistically significant differences in baseline LVEF between the two groups measured in the acute phase of myocardial infarction (29% [SD±2] vs. 30% [SD±3]; p=0.36). However, at the end of the 24-h treatment period LVEF was significantly better in the levosimendan-treated group (55% [SD±8%] vs. 45% [SD±6%]; p=0.003).
4. Discussion
The main finding of our study was that, when CS secondary to severe left ventricular systolic dysfunction complicated successful primary PCI revascularisation in STEMI patients, levosimendan improved cardiac reserve pumping and increased both CI and CPO significantly more than dobutamine at the doses studied, despite efforts to equalise the effect on CI and CPO by adjusting dobutamine administration when necessary. These improvements persisted for at least 24h. Additionally, PCWP reduction was similar with both levosimendan and dobutamine. This may have some important prognostic repercussions for the treatment of patients with CS. Therefore, levosimendan treatment of patients with CS could be considered a valuable therapeutic tool in this clinical setting.
CS complicating AMI is associated with high morbidity and mortality rates 1,17. The SHOCK trial showed that the most effective management strategy is early revascularisation, which significantly decreased the CS mortality rate compared to initial aggressive medical therapy 18. However, despite appropriate intervention, CS continues to be associated with a high short-term mortality rate 19. The patients enrolled in our study had myocardial infarction, revascularised with optimal PCI and later developed CS requiring additional inotropic support. This characteristic differentiates them from the patients included in the SHOCK trial.
The use of mechanical circulatory assist devices like IABP, parenteral vasopressors and inotropic agents, has long been the main therapeutic strategy proposed in CS, and plays an important role in the management of these patients 20. In our study, the use of IABPs — which was at the discretion of the physician treating the patient — was practically non-existent (only one patient in the levosimendan group).
Several randomised double-blind trials have demonstrated the superior clinical and haemodynamic efficacy of intravenous levosimendan compared with intravenous dobutamine or placebo in patients with decompensated HF 567. Even though some of these trials included patients with acute HF 5,6, little is known about the use and efficacy of intravenous levosimendan in acute HF and CS 8,21. The favourable effects of levosimendan on myocardial oxygen consumption have been confirmed in patients undergoing surgical or percutaneous revascularisation 21,22. In a recent study of a small number of patients with myocardial infarction and CS treated with levosimendan 23, we observed that levosimendan exerted positive inotropic and cardioprotective effects. The levosimendan doses used in our study were in the range recommended in HF treatment 3.
Recent studies have shown that CPO is instrumental in the diagnosis of CS 12 and an important determinant of outcomes in patients with CS 10 and chronic HF 24. In patients with chronic HF, cardiac power reserve is significantly diminished and this is strongly correlated with outcome 11,24. In acute HF, most of the cardiac pumping potential is acutely recruited in order to sustain life. Hence, cardiac power measurements at rest, in patients with acute HF, represent recruitable reserves available more accurately, and reflect the severity of the patient's condition. Williams et al. 25 found that CPO was the strongest prognostic predictor of survival in patients with CS. Survivors were those patients who responded to inotropic therapy and showed adequate cardiac reserve (CPO>1W). Absence of myocardial contractile reserve suggests that the patient is unlikely to have enough viable myocardium 25. The primary objective of our study was achieved better at the end of the 24h infusion of levosimendan than of dobutamine. This may suggest that levosimendan improves cardiac reserve better than dobutamine.
The underlying mechanism causing CS in our patients is an important issue: as they may have an extensively stunned myocardium which could recover in due to course after revascularisation, given sustained inotropic support. Myocardial stunning is characterized by reversible myocardial dysfunction which recovers after some delay 26,27. Myocardial stunning can occur in diverse clinical circumstances, such as early reperfusion with thrombolysis or PCI 28, and in a clinical setting it can give rise to a state of cardiac failure — and even CS — with prognostic repercussions on morbidity and mortality. The recovery in ejection fraction seen in our patients supports this hypothesis, but it is also important to note that the particular pharmacodynamics of levosimendan 3,5 might exert a more positive effect than dobutamine in the recovery of myocardial stunning 23.
4.1. Study limitations
This study does have some limitations. The trial was randomized and open-label, so comparisons to currently available inotropic therapies for this condition with regard to efficacy and especially safety must be interpreted with caution. Another limitation of the study is that these favorable preliminary data are from a small series of patients. Although withdrawal of the levosimendan infusion was not necessary in any of the patients, this study was not designed to assess the safety of the drug.
4.2. Conclusions
For the first time, this study shows that in the context of acute ischaemic heart disease, levosimendan improved CPO in AMI patients who developed CS following PCI. Our results are encouraging and suggest that levosimendan could be a better choice than dobutamine as inotropic therapy for patients with CS. However, further investigation is warranted and levosimendan cannot be generally recommended for these patients unless these preliminary data are confirmed by a controlled, randomised double-blind study in a larger series of patients.




