Heart failure after myocardial infarction: clinical presentation and survival†
Abstract
Objectives:
To characterize the presentation and outcome of patients with heart failure (HF) after myocardial infarction (MI) according to left ventricular ejection fraction (LVEF) and test the hypothesis that the outcome of HF did not change over time.
Background:
Little is known about the presentation and outcome of HF post-MI and how these may have changed over time.
Methods:
Using the Rochester Epidemiology Project, all residents of Olmsted County, Minnesota who experienced an incident MI between 1979 and 1998 were identified; MI and HF were validated using standardized criteria. Subjects were followed through their community medical record.
Results:
Between 1979 and 1998, 1915 patients with incident MI and no prior history of HF were identified. Of these, 791(41%) experienced new onset HF as defined by Framingham criteria during 6.6±5.0 years of follow-up. Forty-seven percent were men, mean age was 73±12 years. Forty-four percent had impaired LVEF, 18% preserved LVEF and 38% had no LVEF measurement within 60 days after the HF event. Median survival after HF onset was 4 years and at 5 years after HF onset, only 45% were alive. Older age, male sex, comorbidity, hypertension and no LVEF assessment were associated with increased risk of death, however, patients with impaired LVEF had the worst outcome. Over time, survival did not improve (HR for year: 1.00; 95% CI 0.99, 1.02; P=0.919) even after adjustment for baseline characteristics.
Conclusion:
In this geographically defined cohort of patients with MI, new onset HF after the MI was frequent. When measured, LVEF was most frequently reduced, consistent with systolic heart failure. Mortality was high and did not decline over time and death was independently associated with male sex, older age, hypertension and comorbidity. It also differed according to LVEF, which was inconsistently ascertained in this setting, potentially representing practice opportunities.
1. Introduction
Hospital discharges for heart failure (HF) have increased by 155% over the last 20 years and 4 790 000 Americans carry a diagnosis of HF 1. In this context, HF has been singled out as an emerging epidemic 2. Although the clinical and public health importance of HF is undisputed, the magnitude and determinants of this problem are not adequately characterized.
The characterization of the HF epidemic requires, in particular, proper understanding of HF outcome. While there is recent evidence that survival of HF improved overall, 3 as it is reported for patients with mixed underlying conditions, the trends in outcome remain challenging to interpret and should be completed, as recently underscored, by analyses of outcomes in specific cohorts of HF with defined etiologies 4,5. Data on the survival of HF in populations with one primary, well-defined underlying condition are scarce, particularly for patients with HF and coronary disease, which is now well established as the major contributor to the etiology of heart failure.
Furthermore, adequate characterization of the survival of HF requires insight into the association of left ventricular ejection fraction (LVEF) and survival. Indeed, LVEF is frequently preserved in left ventricular dysfunction with or without symptoms of HF 6–11. As survival among patients with HF and preserved LVEF is often reported only among patients who underwent LVEF assessment, the resulting survival estimates are potentially biased because patients who undergo LVEF assessment differ from those who do not 12. In this context, among patients developing HF following MI, subsequent survival is not fully characterized; in particular, it is not known whether survival improved over time and the association between LVEF and survival is not documented 13. These recognized gaps in knowledge 4,5 constitute the focus of the present study, which was conducted to characterize the presentation and outcome of patients with HF after MI according to their LV function and to examine whether survival among patients with HF after MI improved over time.
2. Methods
2.1. Study setting
Epidemiologic research in Olmsted County, MN, is possible because the county is relatively isolated from other urban centers and nearly all medical care is delivered to local residents by a limited number of providers. Although a higher proportion of the working population is employed in the health care industry, the characteristics of the population of Olmsted County are similar to those of whites in the United States 14.
Mayo Clinic provides approximately half of the primary care and nearly all specialty care for the community. Olmsted Medical Center and its affiliated hospital along with Mayo Clinic and its two affiliated hospitals provide comprehensive care for the region in every specialty. The potential for epidemiologic research in this community is enhanced by the fact that each provider uses a comprehensive medical record system in which all data collected on an individual are assembled in one place. Thus, details are available on every inpatient and outpatient encounter for each patient, including visits to the emergency department, echocardiography and nuclear medicine results, heart catheterization data, and correspondence. Data are retrievable because Mayo Clinic has maintained extensive indices based on clinical and histologic diagnoses and surgical procedures since the early 1900s 15,16. Since 1966, similar indices have been developed for Olmsted Medical Center providers under the aegis of the Rochester Epidemiology Project. The result is the linkage of medical records from all sources of medical care used by the Olmsted County population. The record linkage system therefore constitutes a unique opportunity to ensure complete ascertainment of post-MI HF, including both inpatient and outpatient episodes.
2.2. Data collection
The lists of patients discharged from the hospitals in Olmsted County with diagnoses compatible with MI were obtained from two separate data sources: the Rochester Epidemiology Project index of diagnoses and the Hospital Utilization Review Database, an administrative database of hospitalizations maintained by Mayo Clinic. The target International Classification of Diseases, Ninth Revision (ICD9) codes were 410 (acute myocardial infarction), 411 (other acute and subacute forms of ischemic heart disease), 412 (old myocardial infarction), 413 (angina pectoris), and 414 (other forms of ischemic heart disease). All events coded as 410 and samples of codes 411–414 were reviewed. The sampling fractions were comparable to those used in other studies 15.
Trained nurse abstractors reviewed criteria for residency in Olmsted County and code eligibility for the International Classification of Diseases-Clinical Modification version 9 17. The entire medical record was used to search for previous history of MI in order to ascertain incident status. A computerized algorithm was applied according to standard epidemiologic criteria to assign MI diagnosis based on the information provided on cardiac pain, creatinine phosphokinase (CK) enzyme values and Minnesota coding of the electrocardiogram 15.
Both inpatient and outpatient records were reviewed to ascertain HF during the initial MI hospitalization and follow-up. Details for the selection of the study population are published elsewhere 18. The diagnosis of HF was based on the Framingham criteria 19,20. Nurse abstractors collected data on all inpatient and outpatient HF episodes: patients were included only when the Framingham criteria were fulfilled. To facilitate informal comparisons with other studies and to focus on incident cases of HF after MI, patients with a clinical history of HF in the in- and outpatient setting, if they fulfilled the Framingham criteria before the index MI, were excluded from further analyses 13.
2.3. Determinants of survival after post MI HF
Clinical diagnoses were used for history of hypertension and diabetes mellitus (excluding glucose intolerance, hyperglycemia or hypoglycemia, diabetes insipidus, steroid-induced diabetes, and gestational diabetes). The Charlson Index was used as a indicator of non-cardiovascular comorbidity 21. It contains 19 categories and each category has an associated weight, which is based on the adjusted risk of 1-year mortality. The overall comorbidity score reflects the cumulative increased likelihood of 1-year mortality; the higher the score, the more severe the burden of comorbidity. CK values were transcribed for up to three determinations on the 1st day, and up to two determinations on each of the following 2 days after admission. Information on the presence or absence of a history of trauma or surgery, which might invalidate enzyme values, was recorded. Because CK normal values changed during the study period, peak CK was defined as the ratio of the maximum CK value to the upper limit of normal. This ratio is unitless. Recurrent MI during follow-up was clinically defined based on cardiac pain and increase in CK after review of the entire medical record. We did not use Minnesota coding of the electrocardiogram in patients with recurrent MI. The time between index MI and recurrent MI was prospectively defined as 48 h in addition to a fall and then rise in CK.
Survival post-MI was compared to the expected survival of the Minnesota total population matched by calendar year, age, and sex. The standardized mortality ratio (SMR) was used to compare the two populations. It is the observed number of events divided by the expected numbers of events.
2.4. Left ventricular ejection fraction measurements
Left ventricular ejection fraction (LVEF) measurements were retrieved from the medical record and considered in the analysis if measured within 60 days after the HF event. LVEF was assessed by one or more of the following three methods: transthoracic echocardiography, contrast angiography, and radionuclide ventriculography.
The LVEF was calculated from the ventriculogram by use of the standard area-length ellipsoid formula 22–25, by radionuclide ventriculography with the multiple-gated equilibrium method or by the first-pass technique, 26 and echocardiographic LVEF was determined either by visually estimated LVEF 27,28 or by the modified area–length method 29. Standard clinical procedures for echocardiographic and angiographic determination of LVEF are described in detail elsewhere 30–32.
If patients had more than one LVEF measurement, the value closest to the HF event was used in this analysis. Patients in whom more than one method was used on the same date were assigned a value for LVEF according to the following hierarchy: (1) echocardiographic LVEF; if not available then (2) left heart catheterization LVEF; if not available then (3) radionuclide ventriculographic ejection fraction as previously described 33. HF with preserved LV systolic function was defined as LV ejection fraction (LVEF) greater than or equal to 50%.
2.5. Statistical analyses
The data are presented as frequency or mean±S.D. Associations between post-MI HF with LVEF assessment and several baseline characteristics were tested with Pearson's χ2 tests for categorical variables and analysis of variance for continuous variables. Kaplan–Meier survival plots were compared using log-rank statistics. Proportional hazards regression was used to examine the association between baseline characteristics and death. Results of the final selected model were summarized by presenting the hazard ratio (HR) and corresponding 95% confidence intervals (CI). We tested for interaction between age, sex, LVEF status and year of HF and used quadratic terms for identification of non-linear associations of time to death and year of HF and age. A P value <0.05 was selected for statistical significance. The variables were selected hierarchically based on clinical judgment and published data for entry in the models. We used the statistical package SAS® version 8.2.
This study was approved by the Mayo Foundation Institutional Review Board.
3. Results
3.1. Population and baseline characteristics
Between 1979 and 1998, 2171 patients were hospitalized with incident MI in Olmsted County. Among these, 256 had experienced one episode of HF before the MI and were excluded from further analysis. Thus, the cohort analyzed in the present study included 1915 patients with incident MI and no prior history of HF. Of these, 791 (41%) experienced new onset HF as defined by Framingham criteria during 6.6±5.0 years of follow-up after MI.
With regards to the timing of the HF episode in relation to the index MI, 59% of HF episodes occurred within 30 days post-MI, 68% within 1 year post-MI and 32% thereafter. A total of 9% of the episodes of HF occurred within 1 year post MI but beyond the first month post-MI. On average, 62% of patients with new onset HF post MI underwent an assessment of LVEF within 2 months after the HF episode and this proportion did not change during the last decade (P for trend=0.16)
The clinical characteristics of the 791 patients with post MI HF are presented in Table 1. Among these, 303 (38%) had no LVEF measurement, 143 (18%) had preserved LVEF and 345 (44%) had impaired LVEF. Compared to patients with LVEF measurement, patients without LVEF measurement were older. Patients with HF after MI and impaired LVEF were more likely to be male compared with those patients without LVEF measurement and those with preserved LVEF.
| No LVEF | Preserved | Impaired | P-value | |
|---|---|---|---|---|
| measurement | LVEF | LVEF | ||
| Number of subjects (%) | 303 (38%) | 143 (18%) | 345 (44%) | |
| Age at HF | 75±11 | 71±12 | 72±12 | <0.001 |
| Male sex | 135 (45%) | 57 (40%) | 182 (53%) | 0.017 |
| History of hypertension before MI | 187 (62%) | 91 (64%) | 205 (60%) | 0.683 |
| History of diabetes before MI | 73 (24%) | 39 (27%) | 81 (24%) | 0.674 |
| No comorbidity at index MI | 170 (56%) | 80 (56%) | 217 (63%) | 0.152 |
| Peak CK ratio | 6.1±5.5 | 5.6±5.5 | 7.3±7.1 | 0.011 |
3.2. Survival after heart failure
After the onset of HF, the median survival was 4 years. At 1 year after the onset of HF, survival was 72% and at 5 years 45%. The SMR was 3.1 (95% CI: 2.9, 3.4), P<0.001). Survival differed according to LVEF assessment as shown in the unadjusted Kaplan Meier survival curves presented in fig. Fig. 1. There was no statistical difference in survival of patients with impaired LVEF compared to patients without LVEF assessment (P=0.11). Among patients without LVEF assessment, the median survival was 3.4 years whereas the median survival among patients with preserved and impaired LVEF was 5.8 years and 3.9 years, respectively.
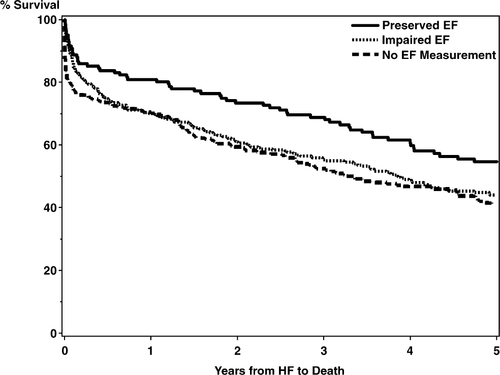
Determinants of survival among patients with HF after MI are presented in Table 2. Univariate analyses showed that the risk of death was 57% higher among patients without LVEF assessment, 35% higher among patients with impaired LVEF, and 53% higher among patients with comorbidities. The risk of death was also increased with increased age and history of hypertension.
| HR (95% CI) | P-value | |
|---|---|---|
| Univariate analysis | ||
| Ejection fraction | 0.001* | |
| No EF measurement | 1.57 (1.22, 2.01) | |
| Impaired EF | 1.35 (1.05, 1.73) | |
| Year of HF | 1.00 (0.99, 1.02) | 0.791 |
| Age at HF | 1.04 (1.03, 1.05) | <0.001 |
| Male | 0.96 (0.82, 1.14) | 0.651 |
| Years from MI to HF | 1.01 (0.99, 1.04) | 0.980 |
| Comorbidity | 1.53 (1.29, 1.81) | <0.001 |
| Recurrent MI | 1.06 (0.90, 1.25) | 0.500 |
| History of hypertension | 1.36 (1.15, 1.63) | <0.001 |
| Creatine kinase | 0.222** | |
| CK tertile 2 | 1.11 (0.90, 1.37) | |
| CK tertile 3 | 0.89 (0.72, 1.09) | |
| Multivariate analysis | ||
| No EF measurement | 1.36 (1.06, 1.76) | 0.018 |
| Impaired EF | 1.38 (1.07, 1.77) | 0.012 |
| Year of HF | 1.00 (0.98, 1.02) | 0.919 |
| Age at HF | 1.04 (1.03, 1.05) | <0.001 |
| Male | 1.38 (1.15, 1.65) | <0.001 |
| Comorbidity | 1.32 (1.11, 1.56) | 0.002 |
| History of hypertension | 1.30 (1.09, 1.55) | 0.004 |
- * P-value from the likelihood ratio chi-square statistic with 2 degrees of freedom.
- ** P-value from the likelihood ratio chi-square statistic with 3 degrees of freedom. Reference level for CK is tertile 1.
The final multivariate model did not detect any association between the year of HF and death, whereas all univariately associated determinants remained independently associated with increased risk of death. In the adjusted model, male sex was associated with a 38% increase in the risk of death while hypertension was associated with a 30% increase in the risk of death.
No trend towards improved survival of patients with post MI HF over time was detected either univariately (P=0.791) or after adjustment (P=0.91).
4. Discussion
In this geographically defined cohort of patients with incident MI, new onset HF after the index MI was frequent. When measured, LVEF was most frequently reduced, consistent with systolic heart failure. Mortality was high and did not decline over time and death was independently associated with male sex, older age, hypertension and comorbidity. It also differed according to LVEF, which was inconsistently ascertained.
4.1. Survival after heart failure
The prognosis of HF is poor with recently reported survival estimates of 50 and 10% at 5 and 10 years, 34 but few population-based data are available on secular trends on the prognosis of HF 6,35,36. Yet, appropriate description of patients’ characteristics and trends in outcome is a key component of the investigation of the HF epidemic. More recent clinical trials of patients with moderate HF, such as the V-HeFT III 37 and the ELITE trials 38, have demonstrated lower mortality rates compared with clinical trials from the late 1980s as did trials on advanced HF 39,40. Administrative data from the Henry Ford Health System 34, and data from Olmsted County 6 and early data from the Framingham Heart Study 19 are in odds with these favorable trends towards lower mortality, suggesting that selection factors inherent to clinical trial designs may in part explain these discrepancies. However, recent data from the Framingham Heart Study indicate that survival after HF improved in more recent years 3.
The aforementioned studies are heterogenous as they inconsistently rely on standardized case definitions, often focus on inpatient HF without including cases occurring in the outpatient setting. As cases of clinical HF may change in severity over time and reflect diverse underlying disease processes, trends in outcome are difficult to interpret in such studies. Indeed, the need to examine survival within specific disease entities leading to HF was recently underscored 4,5.
The data presented herein are obtained in a rigorously ascertained cohort of incident MI without prior history of HF and rely on standardized definitions of HF, including both in and out-patient cases thereby resulting in a well-defined cohort of HF in the setting of overt validated coronary disease. While hypertension was prevalent in this cohort as it is in the general population, all cases of HF occurred subsequent to the MI. This temporal relationship highlights the importance of coronary disease in the genesis of HF. Nonetheless, the association between hypertension and survival underscores the importance of adequate blood pressure control after MI.
Other determinants of survival in patients with HF after MI included male sex that is not predictive of mortality in univariate analysis but is predictive in multivariate. In this case, the association with sex was unmasked after adjusting for age. Sixty-five percent of the women in this cohort are 75 years or older while only 38% of the men are 75 years or older. Without accounting for age, there is no difference in the sexes because the older women die as frequently as the younger men. However, when adjusted for age, men are 32% more likely to die than women. However, the present data extend preexisting knowledge about HF survival by indicating that among patients, who develop HF after MI, survival is poor, and contrary to what was observed among series of HF with mixed etiologies 3, did not improve over the two decades of the study period. Of note, the sample size of the present study is analogous to that of the Framingham Heart Study, which recently reported that survival improved among patients with HF from all causes ascertained with the same criteria as those used herein 3. The present data complement this seminal report by indicating that, among a cohort of comparable size, survival of HF occurring after MI did not improve over time. This suggests in turn that the difference in survival trends between the two studies could reflect differences in the cause of HF with a major role of coronary disease in the present cohort.
4.2. Evaluation of LVEF
To this end, timely ascertainment of LVEF is important to guide management 41,42. Yet, a substantial number of patients with HF post-MI had no measurement of LVEF and this proportion remained constant over the last decade of the study. Other studies underscored that LVEF is under-ascertained in HF 7,43 and the present data extend these reports by indicating that, when HF occurred for the first time after MI, LVEF was not measured in a sizable proportion of the cases, which remained constant in more recent years. As the management of patients benefits from LVEF assessment 44,45 and ACC/AHA guidelines recommend the use of echocardiography with Doppler to evaluate patients with HF 46, these patterns of practice identify opportunities for enhanced care 45,47.
Among cases with LVEF ascertainment, several studies reported that up to half of the cases of HF have preserved LVEF 48,49 leading to the classification of HF into systolic or diastolic HF. There are inherent difficulties in substantiating unequivocally the diagnosis of diastolic heart failure as cardiac catheterization or Doppler echocardiography which can document elevated filling pressures in the absence of reduced LVEF are not routinely performed in practice in all patients with HF in community studies. Thus, the identification of diastolic heart failure remains often exclusionary based on signs and symptoms of HF in the absence of systolic HF. Within this framework, in the present cohort, the frequency of HF with preserved LVEF was 29%, notably smaller than reported in series of HF combining all etiologies 48,49. This difference likely reflects the characteristics of HF occurring in the setting of overt CHD as opposed to mixed etiologies and may explain the difference in survival trends between that present study and other reports. This in turn underscores the importance of studying HF in well-characterized populations, while including cases without measurement of LVEF.
4.3. Strengths and limitations
These results provide important insights into trends in HF survival in the setting of definite coronary disease. The rigor of case ascertainment is in support of the strong internal validity of the present data. Indeed, these apply to a rigorously ascertained cohort of incident MI without prior HF and rely on standardized definitions of HF, including both in and outpatient cases thereby resulting in a well-defined cohort of HF occurring in the setting of overt coronary disease.
Some potential limitations, however, should be kept in mind. While the population of Olmsted County is becoming more diverse, the generalizability of these data to racial and ethnic groups that are not adequately represented in the county studied may be limited and thus the study should be replicated in other racial and ethnic groups.
Our data did not indicate any improvement of survival of HF post MI in the past two decades. While we cannot exclude that a small trend of limited clinical significance may have been missed, the data do not suggest any clinically meaningful improvement in survival and therefore complement existing knowledge on survival of HF of mixed etiologies.
5. Conclusion
In this geographically defined cohort of patients with incident MI, new onset HF after the index MI was frequent. When measured, LVEF was most frequently reduced, consistent with systolic heart failure. Mortality was high and did not decline over time and death was independently associated with male sex, older age, hypertension and comorbidity. It also differed according to LVEF, which was inconsistently ascertained in this setting, potentially representing practice opportunities.
Acknowledgements
We thank Kay Traverse, RN and Susan Stotz, RN, for their assistance with data collection, Jill M. Killian and Ryan A. Meverden for assistance with statistical analyses.




