NT-proBNP and the diagnosis of heart failure: a pooled analysis of three European epidemiological studies
Abstract
Many studies have shown that the B-type natriuretic peptides (BNP and NT-proBNP) are proven diagnostic markers for heart failure due to left ventricular systolic dysfunction. The manner in which they are to be used is still being unravelled; most single centre studies have chosen the best concentration of the peptide on ROC analysis as their cut-point resulting in numerous different values for both BNP and NT-proBNP appearing in the literature. We report a different approach of defining an age and sex corrected abnormal concentration for NT-proBNP, derived from normal individuals within a large sample of 3051 subjects pooled from three European epidemiology studies and applying that to the entire population to detect HF and LVD. Three thousand and fifty one subjects were studied. Of these 10% (305) had significant LVD and 3.1% (94) had HF. The median concentrations of NT-proBNP (IQR) in normals, those with LVD and in heart failure subjects were 20 pg/ml (10.30), 117.3 pg/ml (28.145) and 269.6 pg/ml (54.323), P<0.001, respectively. The area under the ROC curve for NT-proBNP for the detection of ‘heart failure’ was 0.85 and 0.69 for LVD. NT-proBNP was an independent predictor of the presence of HF on multivariate analysis. An abnormal NT-proBNP was defined as being >95th centile for normals, age and sex corrected, and diagnosed HF with a sensitivity of 75% and a negative predictive value of 99%. In an additional analysis in a breathless subgroup of our population, in 30% a raised NT-proBNP concentration could be explained by HF due to LVD, in another 64% the high BNP level was associated with some other structural of functional cardiac abnormality or renal impairment. We were unable to assign a possible cause to the high NT-proBNP values in 5.9% of this breathless subgroup of the population. An abnormal NT-proBNP concentration is an accurate diagnostic test both for the exclusion of HF in the population and in ruling out LVD in breathless subjects. An elevated NT-proBNP merely indicates the presence of ‘cardio-renal distress’ and should prompt referral for further investigation.
1. Introduction
Many single centre community-based epidemiological and hospital cohort studies have now reported on the efficacy of using B-type natriuretic peptide, either BNP 1–4 or its N-terminal fragment 5–7, in diagnosing chronic heart failure (HF) occurring as a result of left ventricular systolic dysfunction (LVD). Such studies have alluded to the particular usefulness of the peptide in ruling out heart failure or LVD.
Most of the studies which have reported, use as their diagnostic cut-point the optimum concentration of BNP or NT-proBNP achieved on receiver operator characteristic (ROC) analysis. Usually, however, in routine clinical practice a cut-point of a biochemical test reflecting abnormality is chosen and applied to diagnose abnormality.
In this study, we report on the usefulness of NT-proBNP in detecting HF in a large sample of 3051 subjects pooled from three European epidemiology studies, using the approach of taking an ‘abnormal NT-proBNP concentration’ defined by the >95th centile, corrected for age and sex, for normals within this population, and applying it to the whole study group.
2. Methods
The study population consisted of 3051 subjects (age range 25–89 years), pooled from three large European population-based studies of LV dysfunction, which had collected compatible clinical and echocardiographic information. The study was a retrospective meta-analysis of three community based observational studies.
The component studies have all published their methods and results elsewhere 8–10. Briefly the cohort was assembled by combining the following epidemiological cohorts:
The Copenhagen General Practitioner study of 683 patients; North Glasgow MONICA a cross sectional population survey of 1207 and the Regensburg/Augsburg MONICA MI-registry and siblings (n=1191)—the KORA family heart study.
The Copenhagen Study comprised 683 unselected subjects older than 50 years, randomly selected from general practices 10. The mean age was 68 years (range: 50–90) and 383 were male. All subjects completed a HF questionnaire blood pressure (BP) was measured, an ECG recorded and plasma stored for subsequent analysis. All subjects underwent echocardiography and global LV function was determined using a 16-segment wall motion score index.
North Glasgow MONICA was a cross-sectional, geographical random sample of 2000 men and women, with 200 men and 200 women in each decade from 25–74 years, carried out in 1992–1993 9. All had a medical history recorded from questionnaire, blood pressure measured, an ECG recorded and plasma stored. Full two-dimensional and M-mode echocardiography was carried out and global LV function was assessed using the Biplane Simpson's Rule technique for the calculation of the left ventricular ejection fraction (LVEF).
The Regensburg/Augsburg study consisted of 609 myocardial infarction (MI) patients and 552 siblings, from a population-based MI register (MONICA Augsburg) 8. The study was carried out in 1996–1997 (1–10 years after MI). All subjects had socioeconomic data recorded and a medical questionnaire, echocardiography—both M-mode and two-dimensional, BP measured, ECGs recorded and plasma stored.
2.1. Pooled cohort methods and definitions
All subjects had standard demographics, questionnaire information as to symptoms of breathlessness, previous medical history, drug therapy, BP measurements and coded ECGs available and plasma which had been stored at −70 °C.
2.2. Echocardiography
Two centres had a LVEF calculated by Simpson's Rule, the other had a LVEF derived from a wall motion score index. LV systolic dysfunction was defined as a value ≤the 2.5th centile for ‘normals’ within each population.
Other echocardiographic variables such as left ventricular hypertrophy (LVH), LV mass and valvular abnormalities were collated.
2.3. NT-proBNP
The NT-proBNP was measured by an ELISA (microtitre plate)-Roche Diagnostics. An abnormal NT-proBNP was defined as an age–sex corrected value >95th centile for normals. The age cut points were chosen at <70 and >70 years.
2.4. Definitions
For the derivation of normal ranges for LVEF and NT-proBNP, ‘normal’ subjects were defined as having no history of cardiovascular disease, the absence of cardiovascular medication, a normal ECG, and a measured blood pressure of ≤140 systolic and ≤90 mmHg diastolic.
Chronic heart failure (HF) was defined as a LVEF ≤2.5th centile for the normal range of each centre and symptoms of dyspnoea and/or loop diuretic therapy.
2.5. Statistics
The concentrations of NT-proBNP are expressed as medians with the interquartile ranges (IQR) in parentheses. Differences in concentration between the natriuretic peptides in those with and without significant left ventricular dysfunction and heart failure were tested using the Kruskal–Wallis test. A multiple logistic regression model was employed to determine the independent predictors of heart failure. Variables included in the model were age, a history of ischaemic heart disease (IHD)-angina or MI, hypertension, diabetes, and the NT-proBNP concentration(logarithmically transformed values). Receiver operator characteristic (ROC) curves were constructed to determine the sensitivity and specificity of NT-proBNP throughout the range of concentrations to detect LVD. The area under the ROC curve (AUC) was estimated according to the method of Hanley and McNeill 11. It provides a measure of the overall diagnostic accuracy of the test. P values <0.05 were considered to be statistically significant.
3. Results
The total number of subjects in the pooled analysis was 3051, 1678 (55%) were male. The mean age was 56.2±13.2 (S.D.). Eighteen percent (549) of the population fulfilled the criteria for ‘normal’, 6.7% (204) had diabetes mellitus, 43% (1312) were hypertensive and 23.4% (714) had evidence of a previous MI.
The prevalence of significant LVD in the study population was 10% (305), 3.1% (94) had heart failure, i.e. were on a loop diuretic and/or had cardiac dyspnoea on questionnaire and had significant LVD.
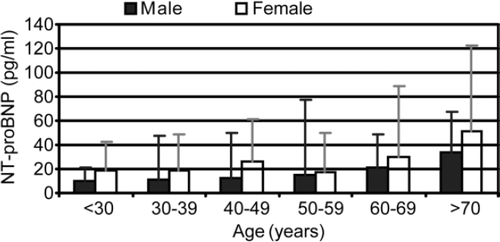
Fig. 1 shows the median concentrations of NT-proBNP (pg/ml) in ‘normal individuals’ by age and sex. It can be seen that the concentrations rise with age and are higher in women than in men. The 95th centile values chosen to define a NT-proBNP value as being ‘abnormal’ in subsequent analyses were >88 pg/ml for women <70 years, >123 pg/ml in women >70 years, >49 pg/ml in men <70 years and >67 pg/ml for men over 70 years.
The median concentration of NT-proBNP (IQR) in normal subjects was 20 pg/ml (10.30), and in those with LVD was 117.3 pg/ml (28.145), P<0.0001. The concentrations were highest in those with heart failure at 269.6 pg/ml (54.323), P<0.001 when compared to normal subjects.
Fig. 2 shows the receiver operator characteristic curves for NT-proBNP for the detection of ‘heart failure’ and ‘LVD’. The AUCs were 0.85 and 0.69, respectively.
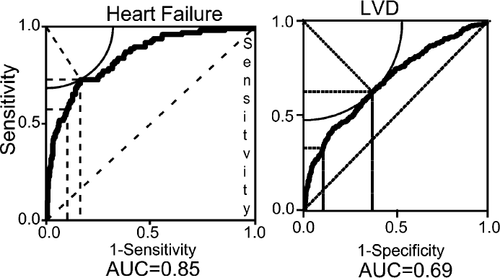
Table 1 lists the independent predictors of heart failure in the multiple logistic regression analysis. It can be seen that NT-proBNP was a strong predictor of the presence of HF—every log unit increase in concentration was associated with an odds ratio of 2.6 for the presence of heart failure.
| Independent predictors of heart failure | ||
|---|---|---|
| Factor | Odds ratio | P value |
| Age (10) | 1.46 | 0.0029 |
| NT-proBNP (log unit) | 2.6 | 0.0001 |
| HT | 2.06 | 0.02 |
| IHD | 3.9 | 0.0001 |
| DM | 2.2 | 0.006 |
| Sex (m) | 0.67 | 0.14 |
- a The odds ratio (OR) for age refers to a 10 year increment. The OR for NT-proBNP is for a log unit increment in concentration. HT refers to the presence of hypertension, IHD to a history of angina or/and MI, DM indicates the presence of diabetes mellitus.
Applying our age–sex corrected 95th centile cut-points to define abnormal values for NT-proBNP to detect abnormality resulted in the peptide having a 75% sensitivity, 79% specificity, 10% positive predictive value and 99% negative predictive value for the diagnosis of heart failure. The test characteristics for the diagnosis of LVD were; a sensitivity of 48%, a specificity of 80%, a positive predictive value of 21% and a negative predictive value of 93%.
We carried out an additional analysis in the subgroup of our total population who reported a history of cardiac dyspnoea on their questionnaire or medical history. Table 2 shows the causes of an abnormal NT-proBNP in these individuals. The categories are mutually exclusive and were assigned in descending order from the top of the table. In 30%, the raised concentration can be explained by heart failure due to LVD. However, it can be seen that, e.g. nearly 20% of subjects post MI, without LVD have a raised NT-proBNP concentration. We were unable to assign a cardiac structural, functional or renal cause to the high NT-proBNP values in 5.9% of this breathless subgroup of the population.
| Risk factor | n (%) | Cumulative n (%) |
|---|---|---|
| Heart failure | 67 (30.3) | 67 (30.3) |
| LVH | 28 (12.7) | 95 (43.0) |
| ↑ LVEDD | 12 (5.4) | 107 (48.4) |
| Valve abnormality | 1 (0.5) | 108 (48.9) |
| Pulmonary hypertension | 2 (0.9) | 110 (49.8) |
| MI | 43 (19.5) | 153 (69.2) |
| Angina | 17 (7.7) | 170 (76.9) |
| HT | 21 (9.5) | 191 (86.4) |
| CV Medication | 5 (2.3) | 196 (88.7) |
| DM | 2 (0.9) | 198 (89.6) |
| Pulmonary disease | 3 (1.4) | 201 (91.0) |
| Renal dysfunction | 4 (1.8) | 205 (92.8) |
| Hx of cardiac disease | 3 (1.4) | 208 (94.1) |
| Remainder | 13 (5.9) | 221 (100) |
- a The table cells are mutually exclusive in descending order from the top. LVH=significant left ventricular hypertrophy on echocardiography, increased LVEDD= and LVEDD>5.6 cm, Valve Abnormality=equals an echocardiographic valve abnormality of at least moderate severity, pulmonary hypertension was defined as a pulmonary systolic pressure of >30 mmHg derived from the tricuspid regurgitant jet on Doppler echocardiography, MI=a history of myocardial infarction, CV medication=the subject was taking cardioactive medication, DM=diabetes mellitus, pulmonary disease=a medical history of COPD, use of inhalers or an FEV1<50% predicted., renal dysfunction=serum creatinine value greater than the upper limit of normal for the centre involved, Hx of cardiac disease=any other cardiac history except MI and valve disease.
In this breathless subgroup, there were 22 false negative cases where the NT-proBNP value was below the age–sex corrected normal value but the subject had significant LVD. The mean age of this group was 61 and the mean LVEF was 38%. Sixteen of the 22 subjects were taking cardioactive medication. Of those who were not on any cardioactive drug which could have lowered NT-proBNP, the ejection fractions of the individuals were very near the limits of normality for their centres: One patient was from Glasgow with a LVEF of 33% (2.5th centile for Glasgow=34%) and five were from Copenhagen, three of whom had LVEFs of 40% (2.5th centile=40%). The two remaining patients from Copenhagen had LVEFs of 35%, one was a 78-year-old woman with a NT-proBNP of 107 pg/ml (upper limit of normal 123 pg/ml) and the other was a 67-year male with a NT-proBNP of 47 pg/ml (upper limit of normal 50 pg/ml).
4. Discussion
This large multi-centre study has confirmed the usefulness of NT-proBNP in the diagnosis of heart failure due to LV systolic dysfunction. In particular, it reiterates that the main diagnostic efficacy of this test lies in its high negative predictive value making it a good rule out test for the exclusion of heart failure. This work adds to the current literature which has demonstrated the utility of NT-proBNP in diagnosing heart failure in single-centre studies 5–7. A multi-centre diagnostic study has been reported for BNP 12 but it concentrated on patients presenting with acute dyspnoea whereas this work shows that NT-proBNP is capable of diagnosing chronic heart failure in a multi-centre setting.
This study, however, is the first to our knowledge to apply an abnormality cut-point for NT-proBNP based on an age and gender corrected 95th centile value derived from a large number of normal men and women from the same study populations who were subjected to the same rigorous investigations as those who subsequently turned out to have cardiovascular disease. It is arguably very important to take this approach as it can be seen from our work and that of others that both NT-proBNP and BNP increase in concentration with advancing age and are higher in men than women 13,14.
Our work also extends the concept that an elevation in the plasma concentration of B-type natriuretic peptide is a non-specific marker of cardio-renal distress 15,8. Less than one third of breathless subjects from our population who had a high NT-proBNP had heart failure due to systolic dysfunction. We did not formally measure diastolic function in our study so we are unable to comment on those who might have had diastolic heart failure. However, we were able to accurately comment on a number of cardiac structural abnormalities; over 10% of breathless subjects with a high NT-proBNP had left ventricular hypertrophy on echocardiography but no LVD and nearly one fifth had a previous MI without demonstrable LVD by the technique we used. 1.8% of those with an elevated NT-proBNP concentration, who did not have any cardiac structural or functional abnormality had impaired renal function. These findings reinforce the point that finding a high B-type natriuretic peptide concentration in a breathless patient merely indicates the presence of ‘cardio-renal’ distress and should prompt further cardiac investigation, which should include echocardiography and measurement of renal function.
Extrapolating from our data to using NT-proBNP to facilitate the diagnosis of heart failure in breathless subjects, many might be disappointed at the low yield. However, in 94% of subjects we were able to assign some structural or functional cardiac or renal abnormality, worthy of further clinical evaluation, which could have explained the high value. This finding should prompt us, in implementing this test into clinical practice, to set up appropriate diagnostic strategies to further investigate the ‘hyper-BNP-aemia’ found.
In seeking to use B-type natriuretic peptide diagnostically many have been concerned about ‘false negative’ values. In this study, we had the opportunity to examine in detail those breathless individuals with LVD who had a low NT-proBNP value. The majority of these patients were on cardio-active medication, which could have lowered the level. As such, clinically we might be reassured that these subjects were known to have a significant cardiac problem and were receiving appropriate medication. The others who were untreated had LV function assessments, which were close to the lower limit of normal values for the participating centres. We also should remember that subjects with a low BNP/NT-proBNP concentration have a good prognosis 16,17.
This study has a number of limitations which should be considered especially when extrapolating the findings to a clinical setting. It comprised three cross-sectional population-based studies with large numbers of ‘healthy’ subjects and small numbers with HF/LVD. Our breathless subgroup may not be representative of patients presenting with dyspnoea to a GP as we used ‘surrogate’ measures for symptoms, i.e. breathlessness from questionnaires. Our ability to exhaust the findings of cardiac structural and functional disease in our population was also limited by our need for a non-invasive approach using echocardiography. A more complete and accurate picture would no doubt be achieved using CMR.
Nevertheless, this large multi-centre population-based study confirms that NT-proBNP is of value in excluding heart failure in the population and in ruling out LV systolic dysfunction in breathless subjects. We now have to embark upon applying the results clinically with the newer rapid assays for B-type natriuretic peptide, which make their use in diagnosis feasible. However, we still have many questions to answer. Will using BNP/NT-proBNP diagnostically be cost-effective= How we will use them—by applying an abnormal cut point as we would advocate from our work or an optimum ROC value= Studies to address these issues will hopefully report soon and help inform us of how best to fit B-type natriuretic peptide into our diagnostic armamentarium for heart failure.




