Use of NT-proBNP in routine testing and comparison to BNP
Abstract
Objectives:
B-type natriuretic peptide (BNP) is a strong diagnostic predictor of left-ventricular (LV)-dysfunction. Recently, the aminoterminal portion of pro-BNP (NT-proBNP) has been introduced, which could be even more sensitive because of its longer half-life. The aim of this study was to evaluate the new marker NT-proBNP within a large, heterogeneous population of patients with suspected cardiovascular disease at risk of cardiovascular dysfunction and to compare it with the established diagnostic parameter BNP.
Subjects and methods:
NT-proBNP and BNP were measured in 339 hospitalised patients undergoing diagnostic angiography (median age 66 years, 244 male vs. 95 female).
Results:
Median values of NT-proBNP increased with worsening LV-dysfunction and higher NYHA class. The area under the receiver operator characteristics curve (AUC) of NT-proBNP for detecting severe systolic dysfunction or for detecting any systolic LV-dysfunction was 0.83 and 0.77, respectively. The latter improved (AUC=0.81) when patients with clinically relevant heart disease like valvular dysfunction were included, independent of the haemodynamic values. Compared to BNP, NT-proBNP tended to be more accurate in identifying lesser degrees of LV-dysfunction.
Conclusions:
Even after optimisation of target criteria, there was still a substantial overlap of NT-proBNP values between patients with and without relevant heart disease. Therefore, NT-proBNP is not suitable as a screening test for LV-dysfunction in the community. Nevertheless, because of its good negative predictive value, NT-proBNP could be an easy and effective tool to rule out severe systolic LV-dysfunction in high risk patients. No clinically significant advantage of BNP testing could be found.
1. Introduction
B-Type natriuretic peptide (BNP) is secreted mainly in the left ventricle in response to elevated wall tension 1. Many publications describe BNP as an excellent marker of left ventricular (LV) function and a simple and effective tool to detect heart failure or LV-dysfunction 2–5. Recently, the aminoterminal part of pro-BNP (NT-proBNP) was introduced, which is secreted in equivalent proportion to BNP. Because of its longer half-life, a higher sensitivity to detect early stage LV-dysfunction was supposed for NT-proBNP 6.
Most studies of NT-proBNP as a screening parameter for LV-dysfunction have either enrolled a small number of highly selected patients or have only assessed severe systolic LV-dysfunction by echocardiography in a community-based setting. The aims of the present study were first, to evaluate NT-proBNP as a marker of LV-dysfunction in a large, unselected population of patients with suspected cardiovascular disease. Secondly, we were interested in analysing the relationship of NT-proBNP to other cardiac diseases. Therefore, NT-proBNP was correlated with invasively determined haemodynamic variables and diagnoses. Thirdly, sensitivity and specificity of NT-proBNP were analysed in comparison to BNP.
2. Methods
2.1. Patients
Three hundred and thirty-nine consecutive hospital in-patients who underwent diagnostic cardiac catheterisation for clinical reasons were enrolled in our study. During cardiac catheterisation, left ventricular end-diastolic pressure (LVEDP) and mean pulmonary-arterial pressure (MPAP) were assessed if indicated. Also, the end-diastolic volume (EDV), the end-systolic volume (ESV) and the ejection fraction (EF) were determined angiographically by standard methods as described previously 7.
2.2. Natriuretic peptide measurements
The venous blood samples were drawn on the day before the catheterisation from clinically stable patients and were collected in EDTA containing tubes. Patients were rested supine for at least 30 min.
The samples were centrifuged within 1 h. One aliquot of the plasma was used for the NT-proBNP measurement (Elecsys proBNP, Roche Diagnostics, Germany), carried out on a Elecsys-2010 bench top analyser. Another aliquot was stored at −20 °C. These second aliquots were stored for 2 weeks and then used for the Shionoria BNP assay (CIS, Schering, Germany). The assays were done in accordance with the producer's manual.
2.3. Statistics
The analyses were done with the statistical analysis software SPSS 10.0 for windows. Variables were expressed as median with the minimum and the maximum value. Differences in the medians were compared by the Mann–Whitney-U test and the Kruskal–Wallis test if there were more than two subgroups, respectively. A P-value of <0.05 was considered statistically significant.
The correlation coefficients were calculated by the linear model of Pearson. Receiver operating characteristics (ROC) plot analysis was used to compare the diagnostic utility of both natriuretic peptides. The threshold for NT-proBNP and BNP was determined retrospectively by the ROC coordinates for a maximum sensitivity of >90% and minimal loss of specificity.
3. Results
Baseline characteristics of the 339 study subjects are shown in Table 1. The cardiological diagnoses are listed in Table 2.
| Number or median | Min–Max* | |
|---|---|---|
| Age (years) | 66 | 24–88 |
| Gender (male/female) | 244/95 | |
| NYHA class I/II/III/IV | 70/221/46/2 | |
| Sinus rhythm/atrial fibrillation or flutter (n=332a) | 292/40 | |
| Brain natriuretic peptide (BNP, pg/ml n=149a) | 38 | 1–1217 |
| Aminoterminal pro–brain natriuretic peptide | 281 | 10–66 441 |
| (NT-proBNP, pg/ml) | ||
| End-diastolic volume (ml, n=334a) | 181 | 73–652 |
| End-systolic volume (ml, n=334a) | 41 | 6–548 |
| Ejection fraction (%, n=338a) | 76 | 13–95 |
| Mean pulmonary arterial pressure | 25 | 12–53 |
| (MPAP mmHg, n=26a) | ||
| Left ventricular end-diastolic pressure | 16 | 2–43 |
| (mmHg, n=336a) |
- * : min: minimal value, max: maximum value, a: these variables were not available for all 339 patients.
| Cardiovascular disease | Number | (%) |
|---|---|---|
| Stable coronary artery disease | 194 | 58 |
| Myocardial infarctiona | 29 | 8 |
| Congenital and/or valvular disease | 38 | 11 |
| Non-ischemic cardiomyopathy | 11 | 3 |
| Inflammatory heart disease | 7 | 2 |
| Peripheral vascular occlusive disease/Aortic aneurysm | 3 | 1 |
| Hypertensionb | 37 | 11 |
| Rhythm disordersc | 8 | 2 |
| Non-cardiovascular diagnosis | 12 | 4 |
| All | 339 | 100 |
- a : defined by increased cardiac specific enzymes and infarct related ECG changes, b: without above shown diseases, c: without structural heart disease.
3.1. Haemodynamics
Values of NT-proBNP were significantly elevated in individuals with reduced EF (<60%), elevated LVEDP (>12 mmHg) or elevated EDV (>220 ml) compared with participants without these features (all P<0.01). As shown in Table 3, the correlation of NT-proBNP with these measures of LV-function was significant but weak (P<0.05). The best correlation coefficients found were 0.44 and −0.47 for ESV and EF.
| Log NT-proBNP | |
|---|---|
| Serum creatinine | 0.27 |
| Log of brain natriuretic peptide (BNP) | 0.90 |
| Age | 0.31 |
| Left ventricular end-diastolic pressure | 0.36 |
| End-diastolic volume | 0.29 |
| End-systolic volume | 0.44 |
| Mean pulmonary-arterial pressure | 0.32 |
| Ejection fraction | −0.47 |
- a Log: Logarithm, all correlations P<0.05.
3.2. NYHA class and LV-dysfunction
Patients were categorized by New-York Heart Association (NYHA) classification for the severity of their exercise limitation at admission. With rising NYHA classes, the NT-proBNP values increased significantly (Fig. 1a). However, the median of NT-proBNP values of patients reported as NYHA class I was not significantly different from subjects classified as NYHA II.
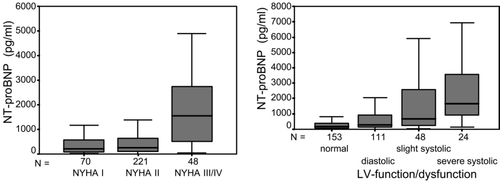
The population was divided in four groups according to their LV-function (Fig. 1b): patients with normal LV-function, patients with diastolic dysfunction, patients with slight systolic and patients with severe systolic dysfunction. With worsening LV-function, the median values of NT-proBNP increased significantly (P<0.05), but with a large overlap between categories
3.3. Diagnostic performance
Table 4 shows the area under the ROC curve (AUC) value for NT-proBNP for the detection of LV-functional abnormalities. Patients with severe systolic LV-dysfunction (n=24) were defined by EF<40%, subjects with any systolic LV-dysfunction (n=72) were defined by EF<60% and finally probands with a systolic or diastolic LV-dysfunction (n=183) were defined by EF<60% or LVEDP>16 mmHg. The AUC rose with increasing LV-dysfunction. As NT-proBNP cut-offs were defined to achieve optimum sensitivity, the negative predictive values were high.
| Left ventricular dysfunction | AUC (95% CI) | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | NT-proBNP cutoff (pg/ml) |
|---|---|---|---|---|---|---|
| Severe systolic (EF<40%) | 0.83 (0.75–0.9) | 91.7 | 60.8 | 15 | 99 | 368.7 |
| Severe systolic or heart disease* | 0.83 (0.78–0.88) | 91.3 | 43 | 41 | 92 | 159.5 |
| Systolic (EF<60%) | 0.77 (0.71–0.83) | 90.3 | 37.2 | 28 | 93 | 152.4 |
| Systolic or heart disease* | 0.81 (0.77–0.86) | 90.6 | 44.3 | 50 | 89 | 150.9 |
| Diastolic/systolic | 0.71 (0.65–0.76) | 88.5 | 37.8 | 63 | 74 | 103.5 |
| (EF<60%/LVEDP>16 mmHg) | ||||||
| Diastolic/systolic or heart disease* | 0.77 (0.72–0.82) | 88.3 | 40.8 | 72 | 67 | 98.3 |
- * relevant heart disease independent of haemodynamics, which means according to categories of Tables 1 and 2: atrial flutter or fibrillation, myocardial infarction or congenital and/or valvular disease, AUC: area under the ROC (receiver operator characteristics) curve, CI: confidence interval, NT-proBNP: aminoterminal part of pro-brain natriuretic peptide, EF: ejection fraction, LVEDP: left-ventricular end-diastolic pressure.
In clinical practice, LV-dysfunction may not be the only cause of heart failure. We therefore extended the target population to the diagnoses myocardial infarction, atrial flutter or fibrillation and relevant valvular heart disease in addition to the above defined LV-dysfunction (Table 4). Thereby the AUC and accordingly the specificity and positive predictive value of NT-proBNP increased.
3.4. Comparison with BNP
BNP was available in a subgroup of 149 patients. The corresponding logarithmic NT-proBNP and BNP values correlated highly significant (r=0.9, P<0.001, Fig. 2). The absolute values of NT-proBNP were by median factor 7.9 higher than the BNP values. There was no difference in this factor within subgroups defined by the degree of LV-dysfunction.
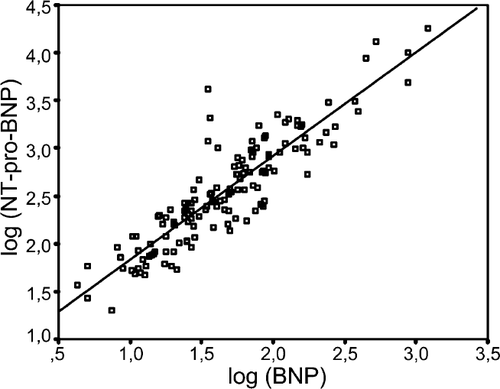
There was no difference for AUC for BNP and NT-proBNP in detecting severe or any systolic LV-dysfunction within these 149 probands. However, the AUC for detection of systolic or diastolic LV-dysfunction tended to be higher for NT-proBNP (Table 5).
| LV-Dysfunction | AUC (95% CI) | |
|---|---|---|
| NT-proBNP | BNP | |
| Severe systolic | 0.87 (0.77–0.96) | 0.87 (0.75–1.00) |
| Systolic | 0.72 (0.62–0.81) | 0.72 (0.62–0.82) |
| Diastolic/systolic | 0.74 (0.66–0.82) | 0.71 (0.63–0.80) |
4. Discussion
This is the first study to prospectively evaluate NT-proBNP as a serum marker of cardiac function in a large, heterogeneous patient population with invasively confirmed anatomic and haemodynamic diagnoses. Many NT-proBNP or BNP studies have included only small numbers of patients, focused on selected patients (for example only patients post myocardial infarction) or excluded patients because of renal failure or valvular disease 5,8–11. The results of these studies cannot readily be transferred to the general population because the high co-morbidity and its effects on natriuretic peptides are not considered. In our study, we included 339 consecutive patients referred for diagnostic cardiac catheterisation. This constitutes a heterogeneous sample consisting of patients with stable as well as unstable coronary heart disease, patients with sinus rhythm or atrial fibrillation and patients with valvular dysfunction as well as inflammatory heart disease.
In the present study, we used a detailed classification of LV-dysfunction, defined by a combination of EF and LVEDP. As expected, NT-proBNP values increased with worsening LV-dysfunction. Nevertheless, there was a great overlap of NT-proBNP values between the different LV-function groups, especially for lesser degree dysfunction. The diagnostic performance indicated as AUC for NT-proBNP was 0.83 for detection of a severe systolic dysfunction, which is comparable with other large scale studies 4,12. The AUC for detection of any systolic LV-dysfunction or systolic or diastolic dysfunction was 0.77 and 0.71, respectively. Even after inclusion of a third haemodynamic variable (EDV) for the definition of LV-dysfunction, the AUC was still not ideal (data not shown).
There are few data comparing BNP and NT-proBNP and these results are controversial 10,13. Our comparison of the diagnostic performance of the natriuretic peptides showed a trend for NT-proBNP to be more accurate in identifying patients with diastolic LV-dysfunction. This could be attributed to the larger half life of NT-proBNP. However, due to the small study population these results must be regarded as preliminary.
Taken together, even after optimisation of target criterions, there was still a large overlap between subgroups leading to low specificity and positive predictive values of NT-proBNP. This result is in accordance with previous studies. Because of its good negative predictive value, NT-proBNP and BNP tests could be used effectively to exclude a relevant systolic LV-dysfunction within a high-risk cardiovascular population. Clinically significant differences between NT-proBNP and BNP could not be detected.




