Liver transplantation for hepatocellular carcinoma: Korean experience
Abstract
Hepatocellular carcinoma (HCC) is the second most common cause of male cancer death in Korea, where the major etiology, chronic hepatitis B virus infection, is endemic. With a high incidence of unresectable HCCs and a low cadaveric organ donation rate, the number of adult living-donor liver transplantations (LDLTs) has increased rapidly, by tenfold, over the past 10 years, as an alternative to deceased-donor liver transplantation (DDLT) in Asia, including Korea. Currently, HCC accounts for more than 40% of the indications for adult LDLT as the associated decompensation cirrhosis or unresectable HCC with 2.8% perioperative mortality at our institute. In determining eligibility for LDLT, the Milan criteria, which have a major aim of reducing the wastage of cadaveric liver grafts, still remain the gold standard. Our published results with 168 adult LDLTs show no difference from the results with DDLT for HCC that meets the Milan criteria. However, since a substantial proportion of adult LDLT patients not fulfilling the Milan criteria have been found to survive for longer than expected, and because a live donor organ is a private gift, most LDLT programs in Korea accept HCC patients beyond the Milan criteria, and the reported 3-year survival rates for such patients are approximately 63%. Our new proposal for expanded criteria (Asan criteria; tumor diameter ≤5 cm, number of lesions ≤6, no gross vascular invasion) in LDLT has focused on extending the number limits but keeping the maximum tumor size at 5 cm, because even modest expansion of tumor size limits beyond the Milan criteria adversely affected survival. The overall 5-year patient survival rates were 76.3 and only 18.9% within and beyond the Asan criteria, respectively; these criteria broaden the indications for patient selection and can more accurately identify patients who will benefit from LDLT than the conventional Milan criteria and the University of California at San Francisco criteria. In Asia, where the option for DDLT is minimal or negligible, LDLT with the modest expanded selection criteria will continue to provide a chance of long-term survival for some patients with advanced HCC.
Introduction
Hepatitis B and C viruses (HBV and HCV) are the most common etiologic agents for hepatocellular carcinoma (HCC). More than 80% of HCC occurs in areas where hepatitis B is endemic, and the geographic distribution of HCC largely follows that of HBV 1. Because of the high carrier rate (5–6% of the general population) of HBV in Korea, this country has one of the highest age-adjusted incidences of HCC (41.95 per 100000 in males and 13.84 per 100000 in females), which is the third most common malignancy, with an annual new incidence of more than 11000 cases 2. Because more than 80% of HCCs have developed from underlying cirrhosis, associated with a variable degree of diminished hepatic functional reserve, often with advanced or multifocal HCCs, hepatic resection as a potentially curative treatment is feasible in only 20% of patients at the time of diagnosis. Liver transplantation is, theoretically, an ultimate cure for HCC, achieving total removal of cancerous lesions and underlying cirrhosis. Through most of the 1980s, however, results of liver transplantation for HCC were disappointing, with high recurrence rates and patient survival of only 30% at 3 years, because of the unrestricted selection criteria. This disappointing experience and the persistent lack of cadaveric liver grafts have forced transplant communities to establish restrictive selection criteria (the Milan criteria) with the aim of predicting and improving the posttransplant survival of HCC patients 3. Concerns have also been raised regarding whether the Milan criteria may be too restrictive, thus excluding patients who would have otherwise done well after transplantation. Meanwhile, in Asia, where the supply of cadaveric grafts remains scarce and the incidence of HCC combined with chronic HBV- and HCV-related liver diseases is higher than in Western countries, adult living-donor liver transplantation (LDLT) has been settled upon as a practical alternative to deceased-donor liver transplantation (DDLT) [4, 5]. Since LDLT does not affect the public resource of cadaveric donor organs and since a substantial number of patients who have had LDLT for HCC not fulfilling the Milan criteria have shown acceptable good outcomes, various expanded selection criteria are now applied at most LDLT centers [6-9]. Despite the theoretical survival benefit of LDLT associated with the almost negligible waiting time and the potentially unlimited availability of a donor organ, enthusiasm for LDLT has waned in Western countries, because the procedure is technically demanding with increased surgery-related morbidity in recipients, it is associated with the risk of donor mortality, and it seems to result in a higher HCC recurrence rate than DDLT 10. In this article, we review the controversial arguments of LDLT over DDLT for HCC, and summarize the current practice and outcomes of LDLT for HCC with the application of our expanded selection criteria.
Role of living-donor liver transplantation for hepatocellular carcinoma at the Asan Medical Center
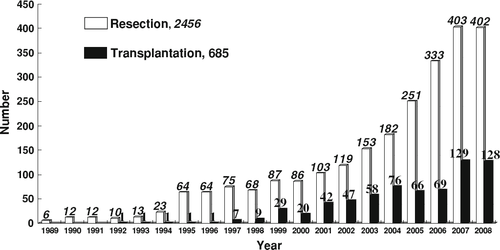
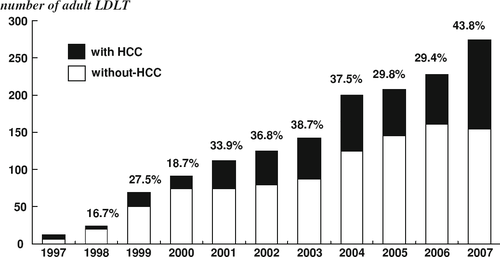
Because of the high prevalence rate of HBV infection in Korea, the number of patients with HCC is substantially higher than that in Western countries. Despite the fact that our institute was founded only in June 1989, it has grown to be one of the largest-volume centers of hepato-biliary-pancreatic surgery and liver transplantation in the world, accumulating 2456 resections and 685 transplantations for HCC until 2008 (Fig. 1). Liver resection is still the first therapeutic option to be considered in HCC patients, even though the HCC in most of them (>80%) is associated with underlying cirrhosis [11, 12]. But the major drawbacks of resection are its low applicability (<20%) due to the patients' limited hepatic functional reserve and advanced tumor diseases, and the progressive deterioration of the underlying cirrhosis and the high intrahepatic recurrence rate after resection. Liver transplantation has been a widely accepted therapeutic option for unresectable HCC associated with cirrhosis. In Asia, the need to resort to live-donor liver donation arose as a natural response to the critical shortage of cadaveric organs and a growing demand for liver transplantation in this region, where the incidence of HBV-related end-stage liver disease and HCC accounts for 75% of the world cases 1. Recent advances in adult LDLT, especially using a right-lobe graft, have overcome the barrier of the deficient graft-recipient weight ratio, and have produced a remarkable change in the role of liver transplantation for HCC. There are 25 liver transplantation centers in Korea, and the Asan Medical Center performs more than 40% of all cases. Since the initiation of adult LDLT for HCC in 1997, the numbers of both resection and transplantation cases have been increasing rapidly, as shown in Fig. 1. From August 1992 to April 2008, 1806 adult patients underwent liver transplantation by means of LDLT (1575 cases) and DDLT (231 cases). HCC accounted for 35.1% of adult LDLTs (553 of 1575 cases) and 22.5% of DDLTs (52 of 231 cases), respectively. As living-donor hepatectomy has been performed with minimal morbidity, and no mortality 13, and the outcome of LDLT for HCC patients within the Milan criteria is comparable to that of benign liver disease, the option of LDLT for HCC patients is increasingly being chosen by medical professionals and the general public. The proportion of patients who undergo LDLT for HCC is increasing, and HCC has recently accounted for more than 40% of the indications for adult LDLT (Fig. 2). Nonetheless, the critical factor that limits the important role of LDLT is the availability of a suitable voluntary donor. According to the Hong Kong group's experiences, there were no voluntary living donors for more than 50% of the adult patients who required LDLT, and their donor selection criteria further limited the use of LDLT in 16% of the patients 14. Our exclusion criteria for a right-lobe live donation are: remnant liver volume <30–35%, steatotic change of the liver more than 10%, and donor's age more than 55 years. The options of dual LDLT, a donor-exchange program between ABO-incompatible groups, and the recent application of ABO-incompatible adult LDLT has increased the applicability of adult LDLT to more than 60% if the patient's family has potential live donors.
Are the results of LDLT comparable to those of DDLT for HCC?
The use of adult LDLT eliminates the prolonged waiting time and decreases the waitlist mortality in patients with HCC in Asia. However, questions are still raised by some groups regarding the higher recurrence rate of HCC after LDLT than after DDLT, even in patients meeting the Milan criteria, and the risk and voluntarism of living donors [10, 15]. Possible explanations for the higher rate of HCC recurrence among patients who have undergone LDLT relate to the loss of the selection effect of waiting patients with more aggressive tumors by putting them on a fast track to transplant; a less optimal cancer operation brought about by greater manipulation of the recipient liver prior to transplant to obtain greater length of hepatic artery, portal vein, and bile duct, as well as preservation of the native vena cava; and the angiogenesis-associated phenomenon attributed to the rapid regeneration of a small-for-size liver graft. However, application of the Milan and University of California at San Francisco (UCSF) criteria to LDLT has resulted in patient survival outcomes very similar to those following DDLT, as shown in high-volume multicenter cohorts from Japan and Korea [16, 17]. Moreover, the prognostic powers of the Milan and UCSF criteria were reported to be the same in both DDLT and LDLT 17. From August 1992 to December 2002, 1085 cases of adult LT (744 LDLT and 341 DDLT) were carried out at 4 institutions in Korea (Asan Medical Center, Catholic University, SamSung Medical Center, and Seoul National University) 17. This case number accounted for 90% of Korean nationwide LTs during the study period. HCC was diagnosed preoperatively or found incidentally in the explanted livers of 312 adult patients (28.8%). In the 312 adult patients, viral infection was associated with liver cirrhosis in 310 (99.4%) patients [hepatitis B, n = 283 (90.7%); hepatitis C, n = 19 (6.1%); both hepatitis B and C, n = 8 (2.6%)]. A nonviral cause was alcoholism [n = 2 (0.6%)]. The pretransplant status in these recipients, according to the Child-Turcotte-Pugh (CTP) classification, was shown to be class A [n = 33 (10.6%)], class B [n = 83 (26.6%)], and class C [n = 196 (62.8%)]. In 39 patients HCC had been found incidentally. Of the 273 patients who had preoperatively diagnosed HCC, 61 (22.3%) did not receive any anti-HCC treatment before LT because of poor liver function or prescheduled LDLT. There were 2 cases of retransplantation due to primary nonfunction of the first graft (DDLT to DDLT, n = 1; DDLT to LDLT, n = 1). Fifty-three of the 75 patients in the DDLT group (70.7%) and 173 of the 237 in the LDLT group (73.0%) met the Milan criteria on the basis of explant pathology (Table 1). The perioperative mortality of DDLT in Korea still remained at more than 18% in this study. The scarcity of cadaveric liver grafts has resulted in a relatively high prevalence of severe early graft dysfunction because of the tendency of accepting most cadaveric grafts and the extremely low opportunity of retransplantation. The overall 3-year survival rate was 61.3% after DDLT and 73.2% after LDLT (Table 1). The 2-year recurrence-free survival rate was 81.6% after DDLT and 79.9% after LDLT (P = 0.884) after the exclusion of 38 perioperative mortalities and 39 patients in whom HCC had been found incidentally (Table 1). All of the HCC recurrences occurred only in the preoperatively diagnosed HCC patients. The patients who met or exceeded the Milan criteria showed 3-year survival rates of 89.9 and 66.4% after DDLT, and 91.4 and 62.6% after LDLT. Our results with DDLT and LDLT in regard to HCC recurrence in recipients within the Milan criteria were comparatively similar not only to the original results of DDLT 3 but also to the Japanese results of LDLT 16. This may imply that the selection criteria of HCC patients for DDLT can be equally applicable to LDLT, considering the donor ethics in adult LDLT.
| DDLT | LDLT | P value | |
|---|---|---|---|
| No. of patients | 75 (24%) | 237 (76%) | |
| Age (mean ± SD, years) | 49 ± 7 | 50 ± 8 | 0.599 |
| Sex | 0.595 | ||
| Male | 60 (80%) | 196 (82.7%) | |
| Female | 15 (20%) | 41 (17.3%) | |
| Child-Turcotte-Pugh classification | 0.005 | ||
| A | 4 (5.3%) | 29 (12.2%) | |
| B | 13 (17.3%) | 70 (29.5%) | |
| C | 55 (73.4%) | 138 (58.3%) | |
| Serology | 0.458 | ||
| Hepatitis B | 68 (90.7%) | 215 (90.7%) | |
| Hepatitis C | 6 (8%) | 13 (5.5%) | |
| Hepatitis B and C | 0 | 8 (3.4%) | |
| None | 1 (1.3%) | 1 (0.4%) | |
| Pathologic tumor stage | 0.767 | ||
| T1 | 34 (45.3%) | 116 (49.0%) | |
| T2 | 25 (33.3%) | 96 (40.5%) | |
| T3 | 16 (21.3%) | 25 (10.5%) | |
| T4 | 0 | 0 | |
| Milan criteria | 0.694 | ||
| Within | 53 (70.7%) | 173 (73%) | |
| Beyond | 22 (29.3%) | 64 (27%) | |
| Perioperative mortality | 14 (18.7%) | 24 (10.1%) | 0.048 |
| Overall 3-year survival rate | 61.3% | 73.2% | 0.043 |
| 2-year recurrence-free survival rate | 81.6% | 79.7% | 0.884 |
- HCC hepatocellular carcinoma, DDLT deceased-donor liver transplantation, LDLT living-donor liver transplantation. Pathologic tumor stage was classified as T1, T2, T3, and T4 according to the new pathologic staging system (American Joint Committee on Cancer/International Union Against Cancer, 6th edition)
Expanded indication criteria of LDLT for HCC at the Asan Medical Center
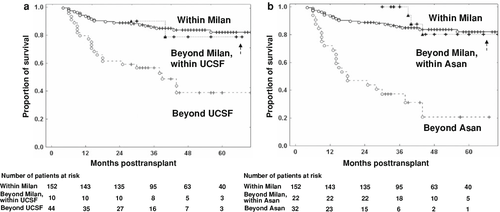
Over the past decade, there has been considerable improvement in the outcome of liver transplantation for HCC, which is attributed almost entirely to better patient selection rather than better surgery or adjuvant therapy 18. The results of the application of the conventional Milan selection criteria have been validated by many centers and are the basis of the current organ allocation policies affording priority to patients with HCC on the DDLT waiting lists in Western countries. Unfortunately, up to 70% of patients with HCC are diagnosed at advanced stages of the disease, and are not suitable candidates for transplantation by the Milan criteria. There has recently been a significant amount of debate in this area, with many arguing that the Milan criteria are too restrictive and the criteria can be expanded without increased HCC recurrence or decreased patient survival 19. Because a live donor graft is a dedicated gift that is directed exclusively to a particular patient, there is no need for an objective allocation system based on a prioritization scheme. LDLT is virtually the almost only option for patients with HCC in Asian countries, where deceased donors are limited 5, and for patients exceeding the Milan criteria in Western countries 6. In a study by Todo et al. 16 of 316 LDLTs for HCC from 49 centers in Japan, the Milan criteria were adopted by only one-third of the transplant programs. However, because early HCC recurrence after LDLT may evoke long-duration psychosocial discouragement to the living donor, it is imperative to improve recipient's survival outcomes by the exclusion of patients who are a high-risk group for HCC recurrence after LDLT. Hence, LDLT for HCC could be propagated more, gaining the confidence of the patients, and more HCC patients would be able to benefit from this potentially curable treatment. The gold standard for the selection of HCC patients for DDLT and LDLT has been the use of the Milan criteria, and the UCSF criteria are regarded as an acceptable guideline. In a single-center experience with 221 HCC patients (29 incidental HCCs and 2 combined HCCs were excluded) who underwent adult LDLT from February 1997 to December 2004 9, 168 patients (76.0%) and 178 patients (80.5%) met the Milan and UCSF criteria, respectively, on the basis of pretransplant imaging (Table 2). During the first 5 months after LDLT, 15 of the 221 HCC patients died of LDLT-related or posttransplant-procedural complications, and this resulted in an in-hospital mortality rate of 6.8%. The pretransplant status of the 221 patients according to the CTP classification was: 11.8%, class A; 32.6%, class B; and 55.6%, class C. According to the MELD score, 27.6 and 6.8% of patients showed scores of 20–29 points and 30 or more points, respectively. Graft-recipient weight ratios ranged from 0.56 to 1.53% (median 0.97%; Table 2). The overall 5-year patient survival rates were 76.0 and 44.5% in patients within and beyond the Milan criteria, respectively; and these rates were 75.9 and 36.4% in patients within and beyond the UCSF criteria, respectively. These data indicated that a nonnegligible number of HCC patients who did not meet those criteria survived for longer than expected. The UCSF criteria, which expanded the maximal tumor size to 6.5 cm for a single lesion, have yielded survival rates comparable to those of the Milan criteria 20. A recent report from an international registry of 1206 HCC patients demonstrated that patients with a single HCC lesion 5.1–6.0 cm in diameter had recurrence-free survival rates equivalent to those of patients with a single tumor 3.1–5.0 cm in diameter 21. In contrast, we observed a lower recurrence-free survival when the tumor diameter exceeded 5 cm in patients with a single HCC (Fig. 3). The 3-year recurrence-free survival rate was 79.0% in patients with a single tumor between 3.5 and 5.0 cm in diameter, but the rate dropped to 20.0% in those with a tumor between 5.1 and 6.5 cm in diameter. Although this difference in recurrence-free survival rates may not be statistically significant due to the small numbers of the enrolled patients (<15 in each group), it is necessary to reevaluate the significance of the maximum tumor size of more than 5 cm in patients with a single HCC. Vascular invasion is associated with the size of the tumor nodule. Characteristically, microscopic vascular invasion involves 20% of tumors 2 cm in diameter, 30–60% of nodules of 2–5 cm, and up to 60–90% of nodules >5 cm in size 22. Two large retrospective studies confirmed that tumors more than 5 cm had a high rate of posttransplantation recurrence, largely because of the association with vascular invasion and poor differentiation [23, 24]. Tumor size may have a more significant impact on recurrence than tumor number, and many new proposals for expanded criteria, including a few in LDLT, have focused on extending the number limit but keeping the maximum tumor size at 5 cm. The Kyoto group reported the results of LDLT in 125 patients with HCC, showing that patients with up to 10 tumors <5 cm in diameter and with a protein induced by vitamin K antagonist (PIVKA) II value <400 mAU/ml enjoyed a 5-year survival of 86.7%, whereas those exceeding these criteria had a 5-year survival of 34.4% 8. The Kyushu group reported a series of 60 patients who underwent LDLT for HCC, in whom the number of tumors did not correlate with the prognosis, but only patients with a tumor diameter of more than 5 cm had a significantly poor prognosis 25. The Tokyo group applied the so-called “5–5 rule” by limiting LDLT to patients with up to 5 nodules with a maximum diameter of 5 cm. The recurrence-free 3-year survival of patients who met the criteria was 94 versus 50% in those patients exceeding the 5–5 rule 7. We found that the independent risk factors for HCC recurrence were largest tumor diameter more than 5 cm, tumor number more than 6, and gross vascular invasion. On the basis of these results, we set the eligibility criteria of LDLT for HCC patients as largest tumor diameter 5 cm or less, tumor number 6 or less, and no gross vascular invasion 9. Of 206 patients who survived the LDLT procedure, 174 (84.5%) met these 3 conditions, 24 (11.7%) met 2, 6 (2.9%) met 1, and 2 (1%) met none. When one of these 3 conditions was not met, there was a definite decrease in the survival rate (Fig. 4). The overall 5-year patient survival rates were 76.3% for those within our expanded criteria and only 18.9% for those beyond our expanded criteria. Although the determination of a definite cutoff value for tumor number requires scrupulous analyses with greater numbers of patients, the presence of numerous (>10) small HCC lesions was associated with a very high risk of recurrence. Interestingly, we have rarely encountered multiple large HCC lesions without gross vascular invasion in the shrunken cirrhotic liver. Because gross vascular invasion into portal and hepatic vein shown by pretransplant imaging has a great impact on both HCC recurrence and patient survival, the presence of gross vascular invasion could not be accepted for LDLT. A comparison of patient survival rates based on the Milan, UCSF, and Asan criteria showed that the overall 5-year patient survival rates were 76.0 and 44.5% within and beyond the Milan criteria, respectively; 75.9 and 36.4% within and beyond the UCSF criteria, respectively; and 76.3 and only 18.9% within and beyond the Asan criteria, respectively (Fig. 4). Although these 3 sets of criteria had similar prognostic power, our expanded selection criteria demonstrated the highest discriminatory power that was defined as the difference in recurrence or survival predictability between HCC patients within and beyond the criteria, emphasizing eligibility for the exclusion of high-risk patients. Of our 221 HCC patients who underwent LDLT between February 1997 and December 2004, 84.5% met the Asan criteria, while 76.0 and 80.5% met the Milan and UCSF criteria, respectively. Therefore, the Asan criteria accepted 10% more HCC patients for LDLT than the Milan criteria and 5.5% more patients than the UCSF criteria. By the application of our expanded criteria, 22 (10%) of the 221 HCC patients could benefit from long-term survival, comparable to that of patients transplanted within the Milan criteria. Thus, our expanded criteria for the LDLT eligibility of HCC patients broaden the indications for patient selection and can more accurately identify patients who will benefit from LDLT.
| Parameter | Value |
|---|---|
| Age (years, mean ± SD) | 51 ± 7 |
| Sex, n (%) | |
| Male | 175 (79.2) |
| Female | 46 (20.8) |
| Serology, n (%) | |
| Hepatitis B | 206 (93.2) |
| Hepatitis C | 15 (6.8) |
| Child-Pugh classification, n (%) | |
| Class A | 26 (11.8) |
| Class B | 72 (32.6) |
| Class C | 123 (55.6) |
| MELD score, n (%) | |
| Median (range) | 16 (3–40) |
| <10 | 32 (14.5) |
| 10–19 | 113 (51.1) |
| 20–29 | 61 (27.6) |
| ≥30 | 15 (6.8) |
| Living donor liver graft, n (%) | |
| Right liver graft | 125 (56.6) |
| Left liver graft | 51 (23.1) |
| Dual grafts | 44 (19.9) |
| Graft-recipient weight ratio, n (%) | |
| Median (range) | 0.97 (0.56–1.53) |
| <0.8 | 42 (19) |
| 0.8–1.0 | 95 (43) |
| >1.0 | 84 (38) |
| Selection criteria by pretransplant imaging | |
| Milan | |
| Within | 168 (76.0%) |
| Beyond | 53 (24.0%) |
| UCSF | |
| Within | 178 (80.5%) |
| Beyond | 43 (19.5%) |
| Asan | |
| Within | 189 (85.5%) |
| Beyond | 32 (14.5%) |
- LDLT living-donor liver transplantation, MELD model for end-stage liver disease, UCSF University of California at San Francisco

Meanwhile, the debate surrounding the applicability of the expanded criteria for liver transplantation in patients with HCC still remains, because limitations of the current selection criteria are based solely on the morphological staging system by pretransplant radiological imaging. Tumor grade and microvascular invasion as surrogate markers of the biological behavior of HCC can only be evaluated at the time of histological examination of the explanted liver or pretransplant tumor biopsy; hence, the clinical utility of these parameters is limited. Several groups have shown that parameters of tumor biology, such as vascular invasion and tumor differentiation, may significantly influence outcomes after hepatic resection and liver transplantation for HCC. Accurate pretransplant prediction of these parameters of histopathological tumor aggressiveness might lead to a reasonable expansion of the selection criteria and/or avoid the unnecessary exclusion of transplant candidates, with regard to acceptable size and numbers of HCC nodules. Preoperative assessment of serum alpha-fetoprotein (AFP) and PIVKA II levels, and positron emission tomography (PET) using 18F-fluorodeoxyglucose (FDG), are currently proposed as additional noninvasive tools for predicting biological tumor behavior such as microvascular invasion and posttransplant tumor recurrence in liver transplant candidates with HCC [8, 26-28].
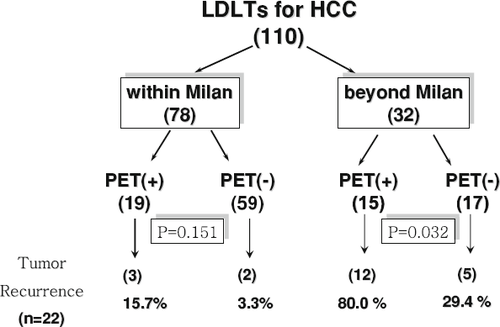
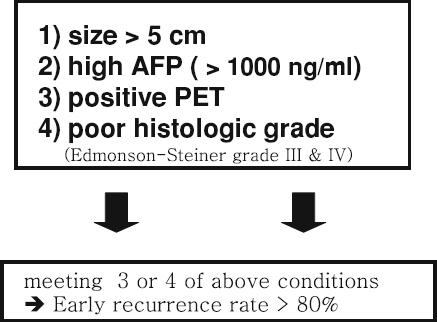
We performed a retrospective analysis to determine the prognostic value of preoperative 18F-FDG-PET in adult LDLT patients, with respect to its power for predicting aggressive tumor biology such as posttransplant tumor recurrence. Between January 2003 and December 2005, 110 (MELD score < 20) of 192 LDLT recipients associated with HCC were investigated with preoperative whole-body PET scans for the detection of extrahepatic metastases (Fig. 5). Of the 110 patients, 78 and 32 were within and beyond the Milan criteria, respectively. Nineteen of the 78 patients within the Milan criteria had positive (+) PET scans (24.4%), while 15 of the 32 patients beyond the Milan criteria had (+) PET scans (46.9%). The 2-year tumor recurrence rates were 3.3% in the PET (–) HCC patients, compared to 15.7% in the PET (+) HCC patients within the Milan criteria. In the HCC patients beyond the Milan criteria, the 2-year tumor recurrence rates were 29.4% in the PET (–) patients, compared to 80.0% in the PET (–) patients (Fig. 5). These results indicate that the association between tumor recurrence rate and a positive PET finding in HCC patients beyond the Milan criteria was significant (P = 0.032), and PET (+) patients were found to have an overall higher risk of tumor recurrence than those with PET (–) findings. Pretransplant 18F-FDG-PET scan could be an additional parameter for the evaluation of tumor aggressiveness and a useful diagnostic tool for better decision-making about whether or not to exclude patients with advanced HCC as liver transplant candidates. The incorporation of tumor size more than 5 cm, serum AFP more than 1000 ng/ml, PET (+), and poor histological grade by pretransplant tumor biopsy into a scoring system as selection criteria for excluding HCC patients for LDLT could help to identify the patient group at very high risk of HCC recurrence in our study (Fig. 6). If 3 or all 4 of these conditions were met, the 1-year tumor recurrence rate would be expected to be >80%.
Conclusion
The high incidence of HCC and the scarce organ donation rate from deceased donors in Asia have led to a distinctive pattern of indications and strategies in the application of liver transplantation. Although the promotion of deceased organ donation is encouraged in our society, LDLT will still keep on increasing as the dominant strategy for the treatment of HCC in cirrhotic patients. The crucial prerequisite for applying this procedure is minimal morbidity risk and no mortality to the healthy live donor, and donor voluntarism. We found that the prognostic validity of the Milan criteria for DDLT could be equally applicable to LDLT for patients with HCC. Our overall results of LDLT for HCC under our expanded selection criteria were found to be acceptable. Tumor size more than 5 cm was shown to carry a high risk of recurrence due to the high rate of vascular invasion; however, tumor numbers of 6 or less did not affect the recurrence rate. The expanded indication for LDLT in terms of tumor number was therefore justified. In addition, serum AFP and PIVKA II levels, and FDG-PET scans, as parameters of the biological behavior of tumors, will help in decision-making about the inclusion or exclusion of LDLT candidates with HCC beyond the current expanded selection criteria.