Social connection as a critical factor for mental and physical health: evidence, trends, challenges, and future implications
Abstract
Rising concerns about social isolation and loneliness globally have highlighted the need for a greater understanding of their mental and physical health implications. Robust evidence documents social connection factors as independent predictors of mental and physical health, with some of the strongest evidence on mortality. Although most data are observational, evidence points to directionality of effects, plausible pathways, and in some cases a causal link between social connection and later health outcomes. Societal trends across several indicators reveal increasing rates of those who lack social connection, and a significant portion of the population reporting loneliness. The scientific study on social isolation and loneliness has substantially extended over the past two decades, particularly since 2020; however, its relevance to health and mortality remains underappreciated by the public. Despite the breadth of evidence, several challenges remain, including the need for a common language to reconcile the diverse relevant terms across scientific disciplines, consistent multi-factorial measurement to assess risk, and effective solutions to prevent and mitigate risk. The urgency for future health is underscored by the potentially longer-term consequences of the COVID-19 pandemic, and the role of digital technologies in societal shifts, that could contribute to further declines in social, mental and physical health. To reverse these trends and meet these challenges, recommendations are offered to more comprehensively address gaps in our understanding, and to foster social connection and address social isolation and loneliness.
In a joint statement published in January 2024, the governments of the US, Japan, Morocco, Sweden, Kenya and Chile highlighted “the importance of social connection to the health and well-being of individuals, communities and societies”1. This came at the heels of the COVID-19 pandemic, a more than three-year period in which the global population had to isolate, practice “social distancing” and, in many cases, was homebound, all factors contributing to reduced social contact. However, while that global health crisis helped raise awareness of the importance of this issue, scientific evidence was already documenting the significant mental and physical health implications of declining social connection.
Social connection is widely acknowledged to be a fundamental human need2, 3, linked to higher well-being, safety, resilience and prosperity, and to longer lifespan4. Across social species, research demonstrates that social connection is one of the strongest predictors of survival, both early and later in life, through adaptive behavioral and biological mechanisms5, 6. The availability and diversity of social relationships, interactions and networks are critical for health and well-being4, 7, 8. Therefore, it is imperative to understand how new trends involving social connection relate to shifts in important societal outcomes such as mental disorders and physical diseases.
Rising global concerns about a “loneliness epidemic” in public discourse have been accompanied by increased academic research and heightened engagement among communities, institutions and governments. These concerns are being reflected in national and international responses to this “epidemic”. In 2018, the UK appointed a Minister of Loneliness9, establishing a national strategy and awareness campaign. Japan followed by appointing a Minister of Loneliness in 202110. Beginning in 2018, the European Union has produced several reports on loneliness11. In 2023, the US Surgeon General issued an Advisory and a framework for a national strategy on “our epidemic of loneliness and isolation”4. In the same year, the South Korean government took a tangible step, offering monthly stipends to encourage young socially isolated individuals to reintegrate into society12. Outside governments, the World Health Organization (WHO) launched in 2023 a Commission on Social Connection, a three-year effort to raise global awareness and mobilize support in this area13.
These efforts have been prompted by data documenting recent increases in social isolation and loneliness, and decreases in social connection globally4. Factors including modernization in society, economic disparities, the introduction of digital technologies, shifts in civic engagement, growing political divides and radicalization, and others, have been examined as potential contributors to this decline in social connection. Whether this is a social recession, a loneliness epidemic, or a public health crisis, it is clearly a pressing issue.
This is a critical moment to act and bridge the gaps in our collective knowledge to mitigate adverse outcomes. However, there are several challenges to be addressed. Over the years, the relevance of social connection to our health has emerged in various disciplines, leading to a complex and potentially confusing evidence base. This calls for a common language to be established. However, in the process, we risk oversimplifying the issue and falling short of an adequate response. With increasing public and governmental attention, this is a critical time to take stock of the strengths and gaps in the existing evidence, the challenges to be faced, and the implications for the future.
SOCIAL CONNECTION AND MENTAL HEALTH
There is a robust evidence base linking social connection to mental health outcomes. Social connection plays a vital role in preventing mental health problems, maintaining good mental health, and aiding in the recovery from both moderate and severe mental health conditions, while isolation and loneliness have been associated with poorer mental health. Most of this evidence regards depression, with fewer studies considering other mental disorders.
Although most available data are observational and cannot demonstrate causality, there are longitudinal studies that provide more robust evidence to indicate directionality, and recent evidence using Mendelian randomization to establish causal relationships14. In some cases, associations appear to be bidirectional, meaning that there is evidence to suggest that social isolation and loneliness increase the risk for poorer mental health, as well as evidence that poorer mental health increases the risk for isolation and loneliness15.
Depression
There is a strong positive association of social isolation and loneliness with depression from youth to older adulthood. Further, higher social connectedness is protective towards depressive symptoms and disorders16.
When looking at adults of all ages, 18 years and older, data from the US National Health Interview Survey examined the impact of living alone and the availability of social and emotional support on depression17. Adults living alone reported significantly higher depression than those living with others, and this difference held across several sociodemographic factors. Adults never or rarely receiving social and emotional support were twice as likely to report depression, but adults living alone were still more likely to report depression even compared to adults living with others who did not receive social and emotional support17.
Importantly, longitudinal evidence suggests that social isolation and loneliness likely cause or worsen depression over time. For example, a systematic review of 32 longitudinal studies from the general population examined whether subjective feelings of loneliness predicted the onset of a new diagnosis of depression18. Studies followed participants from six months to 16 years, with an average follow-up of 3.5 years. The odds of developing new depression in adults were more than double among those who reported often feeling lonely compared to those rarely or never feeling lonely. While there were more studies among older adults, the findings were consistent among younger age groups, including university students and new mothers.
Using two large datasets – the Psychiatric Genomics Consortium meta-analysis of major depression (N=142,646)19, and the Million Veteran Program (N=250,215)20 – to apply a two-sample Mendelian randomization design, loneliness appeared to cause incident major depression and depressive symptoms14. These analyses were then reversed using loneliness outcome data from the UK biobank. Remarkably, data demonstrated that loneliness causally predicts major depression, but the reverse is also true, with major depression causally predicting loneliness14. This suggests that loneliness is both a cause and a consequence of major depression; thus, public health strategies to reduce loneliness may potentially be effective in preventing the onset of depression and reducing depressive symptoms, and better treatments for depression are likely to reduce loneliness.
The link between social connection and depression has also been examined among patients in medical settings, suggesting potential spillover effects on other clinical conditions. For example, low social support had a significant positive association with antenatal depression, which contributes significantly to maternal physical health21. In a review, 83% of studies found that pregnant women with low social support had greater depressive symptoms16.
The links between social connection and mental health are also relevant within occupational settings. The strain on employees across sectors, particularly those hit hardest during the COVID-19 pandemic – such as health care providers, educators, and other “essential employees” – has brought greater attention to burnout and other mental health concerns. A meta-analysis of studies in health care workers found that a lack of social support significantly contributed to higher risk for acute stress disorder, burnout, anxiety, depression, and post-traumatic stress disorder22.
Cognitive health
Several meta-analyses consistently show that stronger social connection – including social networks (e.g., number of social contacts, frequency of interaction, marital status, living arrangement) and social engagement (e.g., attending social groups; visiting family, friends and neighbors; engaging in voluntary or paid work, participation in cultural or leisure activities) – is associated with better cognitive function, but the evidence is less consistent for perceptions of loneliness.
For example, a meta-analysis including over 2.3 million participants showed that living alone, having a smaller social network, having a low frequency of social contact, and having poor social support were risk factors for dementia, while loneliness was not23. However, other meta-analyses did find that greater loneliness was significantly associated with incident dementia24, 25. Conversely, greater social engagement, including a greater number of social memberships, number of social contacts, and more social participation, may be protective, as these were associated with lower dementia risk23, 26.
SOCIAL CONNECTION AND PHYSICAL HEALTH
Robust evidence links social connection, isolation and loneliness to an increased incidence of several physical diseases and to earlier death. The strength of this evidence has been acknowledged in multiple National Academy of Science, Engineering, and Medicine (NASEM) consensus study reports15, 27, scientific statements by professional associations such as the American Heart Association28, and the US Surgeon General Advisory issued in 20234. The evidence can be found in several meta-analyses and systematic reviews that document the overall effects on physical morbidity29-31, and on disease-related as well as all-cause mortality32-43. There are also meta-analyses on clinical outcomes such as response to vaccine44.
This body of evidence led a NASEM consensus study report to conclude that “social isolation is a major public health concern”15. This is noteworthy, since the report was published before the COVID-19 pandemic and there has been a significant volume of research on this topic from 2020 onward.
Physical morbidity
There is a rich and growing body of evidence across a variety of physical health outcomes, including major health indicators such as cardiovascular diseases, stroke and diabetes mellitus.
Cardiovascular diseases are the leading cause of death globally, accounting for roughly one third of all deaths; therefore, factors that increase or decrease this risk can have a major global health impact45. Dozens of studies have found that social isolation and loneliness significantly influence the risk of cardiovascular and cerebrovascular morbidities15, 29.
The culmination of this evidence resulted in a statement published by the American Heart Association in 2022, acknowledging this risk from objective and perceived social isolation28. According to this review of the evidence, there is a clear link of social isolation and loneliness with risk for coronary heart disease and stroke. Among the evidence, a synthesis of data across 16 independent longitudinal studies demonstrates that poor social relationships (social isolation, poor social support, loneliness) were associated with a 29% increase in the risk of incident coronary heart disease and a 32% increase in the risk of stroke29. These findings were consistent across genders.
Low social connection and loneliness have also been associated with a greater risk for hypertension. Indeed, data from the National Social Life, Health and Aging Project suggest that the impact of social isolation on risk for hypertension exceeds that of clinical factors such as diabetes mellitus, pointing to a “causal role of social connections in reducing hypertension” in older age46.
Diabetes mellitus is a leading source of disability, lost productivity, mortality, and lower quality of life, affecting nearly half a billion people worldwide, with a significant global economic burden on individuals, health care systems, and countries47. Studies have repeatedly shown that social connection (e.g., family support and involvement) can positively influence the management and overall health of individuals with type 1 and 2 diabetes. Large population studies also demonstrate the influence of social connection on the incidence of type 2 diabetes. For example, people with smaller social networks were more likely to have been recently diagnosed with type 2 diabetes, to have previously been diagnosed with this condition, and to have diabetic complications48, 49.
However, gender differences have been found along different indicators of social connection. Low social participation was linked to pre-diabetes and complications among women but not men, while living alone increased the likelihood of previously diagnosed type 2 diabetes and its complications in men but not in women48, 49. These findings were independent of glycemic control, quality of life, and cardiac risk factors.
Diabetic outcomes may be due to better self-care among those who are more socially connected. For example, in a meta-analysis of 28 studies, social support was significantly associated with better self-care, particularly glucose monitoring, and was stronger among those with type 2 than type 1 diabetes50. Improving diabetic outcomes via social connection can have cascading public health implications, given that diabetes mellitus often leads to other health outcomes, including heart disease, kidney failure, blindness, amputation and dementia.
There is also evidence to suggest that poor social connection is associated with worse outcomes among those who are already ill. For example, heart failure patients who self-reported high levels of loneliness had a 68% increased risk of hospitalization, a 57% higher risk of emergency hospital visits, and a 26% increased risk of outpatient visits compared with patients reporting low loneliness51. In a meta-analysis of 13 studies on heart failure patients, poor social connection was associated with a 55% greater risk of hospital readmission52. This was consistent across both objective and perceived social isolation, living alone, lack of social support, and poor social network. These data suggest that improving social connection among those who are sick can improve medical outcomes.
Mortality
Several reviews of the evidence, including a NASEM scientific consensus study, have concluded that some of the strongest evidence linking social connection, isolation and loneliness to health-relevant outcomes is that concerning mortality15. Large population-based epidemiological studies have tracked initially healthy populations over time, for years and often decades, documenting that those who are more socially connected live longer35, 38, 41, 42, while those who experience social deficits (isolation, loneliness, living alone, poor-quality relationships) are more likely to die earlier, regardless of the cause of death33, 36, 37, 39, 40, 43. Although social isolation has been implicated as a risk factor for death by suicide53, most meta-analyses on mortality exclude suicide as a cause of death.
Based on meta-analytic data, one estimate suggests that the association between social connection and survival may be as high as 50%42, while isolation is associated with 32% and loneliness with 14% increased risk for earlier death33. While estimates vary to some extent, they may be conservative, given that many reviews and meta-analyses often exclude studies that focus specifically on deaths due to unnatural causes such as unintended injuries, violence or suicide. While there are more studies and stronger effects on cardiovascular-related deaths (e.g., myocardial infarction, stroke) and cancer-related deaths (e.g., leukemia, lymphomas, breast cancer)41, more research is still needed on these, in addition to other disease-related causes of death.
Over the years, the number of studies, the rigor of methodology, and the size of samples have all increased substantially, replicating the finding that social connection decreases the risk of premature mortality and providing stronger confidence in this evidence. For example, longitudinal data from the UK Biobank regard nearly half a million people, reducing the likelihood of random error54. These data demonstrate that social isolation significantly increases risk for earlier all-cause mortality, overall and consistently across subgroups (i.e., males and females, young and older, health and unhealthy, various ethnicities), even after adjusting for a robust set of lifestyle, socioeconomic, biological, and health risk factors55.
Several meta-analyses and systematic reviews have documented similar findings across different ways of examining the issue, including social relationships broadly, social networks, social contact frequency, marital/partnership status, marriage dissolution, social isolation, loneliness, and living alone32, 43. While the magnitude of the effect varies to some extent across studies and depending on which aspect of social connection is being examined, the evidence points to the same general conclusion: indicators of greater social connection are associated with reduced risk, while indicators of social deficits are associated with greater risk for premature mortality.
THE RELATIVE INFLUENCE OF ISOLATION AND LONELINESS
When predicting the risk of future disease, does the subjective (loneliness) or the objective (isolation) aspect matter most? The English Longitudinal Study of Ageing, conducted in nearly 5,400 adults over the age of 50, followed for an average of 5.4 years, found that loneliness was associated with an increased risk for cardiovascular disease (coronary heart disease and stroke), but did not find the same outcomes for social isolation56. On the other hand, the UK Biobank, a large-scale research effort collecting data on nearly half a million people, followed for an average of 7.1 years, found that both isolation and loneliness were associated with an increased risk of acute myocardial infarction and stroke57. However, the impact of social isolation remained significant after adjusting for other risk factors, while the effect of loneliness was attenuated. Both isolation and loneliness were significant predictors of cardiovascular outcomes; however, the relative importance seemed to be stronger for objective isolation.
Research is increasingly looking at the relative importance of isolation and loneliness, and considering multiple outcomes simultaneously. Growing evidence suggests that loneliness has a stronger impact on mental health outcomes, while isolation has a stronger impact on physical health outcomes31, 58. For example, a large national prospective study, examining the effects of social isolation and loneliness on 32 physical, behavioral and mental health outcomes, demonstrated that both were independent predictors, but isolation had a stronger effect on mortality while loneliness had a stronger effect on mental health outcomes58.
PATHWAYS AMONG SOCIAL AND HEALTH FACTORS
The evidence on the protective effects of being socially connected and the risk associated with social disconnection is often studied and discussed separately. However, these conditions intersect in meaningful ways. This includes direct and indirect, bidirectional and cyclical, as well as additive and multiplicative effects. Much of the evidence to date has focused on establishing the direct and indirect effects. A simplified model of these pathways is illustrated in Figure 1.
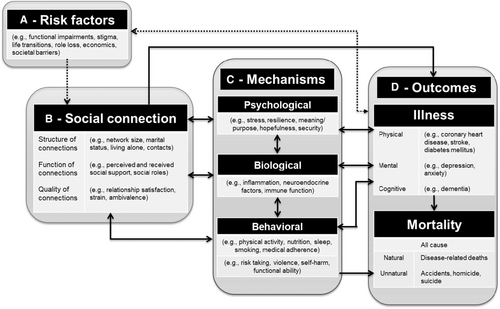
Among the growing body of literature on social connection and health, studies often focus on establishing a directional influence of some aspects of social connection (represented as B in the figure) on various health or mortality outcomes (represented as D). Further work has examined the mechanisms (represented as C) that provide plausible psychological, biological and behavioral explanations for these effects59-64.
Several reviews and meta-analyses document the evidence pointing to psychological pathways such as perceived stress60, 65; behavioral pathways such as sleep66, physical activity and smoking67; and biological factors such as inflammation68. Studies further examine the risk factors (represented as A in the figure) that can potentially compromise one's social connection.
The associations of primary interest in research have been between B and D, with B treated as the predictor variable and D as the outcome variable. Subsequent research has treated C as mediator variables and A as risk factors. However, associations are likely far more complex.
Many factors examined as plausible pathways (represented as C in Figure 1) are also notable outcomes, often treated as clinical endpoints. For example, social isolation and loneliness have been linked to poorer nutritional/eating behaviors considered harmful to health, including low fruit and vegetable intake, and poorer overall diet quality69. There is also evidence that those who are socially isolated are less likely to get preventive screenings, such as a mammogram70.
A synthesis of 122 empirical studies examined the effects of differences in social connection on medical adherence71. Higher social connectedness, particularly social support, has been linked to better medical adherence across several physical diseases, especially hypertension72, 73 and type 2 diabetes mellitus74, 75. Similarly, other factors such as stress can be both an endpoint and a mechanism by which social connection influences morbidity and mortality.
The directionality, or bidirectionality, of these associations may be relevant. While those linked to mortality are unidirectional (i.e., end-of-life stops any further influence), nearly all other pathways may be bidirectional. While there is robust evidence of directional effects (i.e., those less socially connected are more likely to develop poorer health conditions), the reverse can also be true (i.e., poorer health also predicts a greater risk for social isolation and loneliness). The relevant mechanisms are both plausible and supported by evidence. Poorer physical health can also contribute to both greater isolation or loneliness and poorer mental health, creating complex bidirectional associations.
These associations may also be cyclical. Poor social connection can dysregulate our physiology and behavior in ways that put us at risk of developing poorer health. Poorer health may reduce people's willingness, ability or access to connect socially, resulting in greater isolation, which in turn impedes their ability to manage their illness, leading to worse prognoses.
We also need to understand the complexity of the factors contained within the model and how that can potentially result in additive and multiplicative effects. For example, co-occurring deficits of social connection (e.g., living alone, small social network, low levels of social support, and loneliness) may contribute to biological, psychological and behavioral pathways, potentially magnifying the risk to health. Furthermore, like many behavioral and lifestyle risk factors that can influence multiple chronic health conditions, the evidence similarly points to poor social connectedness leading to greater risk (and greater social connectedness reducing risk) for multiple health conditions. Thus, it is probable that poor social connection can increase the risk of comorbidities among physical, mental and cognitive health conditions. This is consistent with data from the Health and Retirement Study which demonstrate that social isolation was significantly associated with 32 indicators of physical, behavioral and psychological health outcomes58.
STRENGTHS AND GAPS IN THE EVIDENCE
The scientific evidence base for the health relevance of social connection is robust, with consistent findings emerging over the past few decades, reinforced across several scientific disciplines (e.g., epidemiology, neuroscience, sociology, medicine, psychology), and using a variety of methodological approaches (e.g., longitudinal, cross-sectional, experimental).
Several meta-analyses and systematic reviews document converging evidence linking social connection, isolation and/or loneliness to psychological, cognitive and physical health. Together, these include hundreds of studies with millions of participants. While most data are observational, there is substantial prospective evidence to establish the temporality of effects42, and evidence to support a gradient or dose-response effect46.
There is also experimental evidence in humans and animals to support a potential causal association. For example, experimentally housing animals in isolation versus socially leads to poorer outcomes, including the development of tumors, stroke, impaired healing, and death5. Animal models have also validated potential molecular, cellular, immunological and behavioral effects for human social disconnection3. These experimental studies further map causal associations between social perception, neural activity, immunological function, and health3.
In humans, randomized controlled trials (RCTs) experimentally test the potential benefits of social interventions. For instance, a meta-analysis of 106 RCTs found that patients who received psychosocial support in addition to treatment as usual had 20% increased odds of survival than those in the control group who received only standard medical treatment76. Although there was variability across types of support interventions, the findings were consistent across patients being treated for cardiovascular diseases, cancer and other conditions.
Drawing causal inferences among factors known to influence health is essential to determine etiology and prevention efforts. However, randomization is not always appropriate in the context of understanding isolation, loneliness, and social connection. Furthermore, although the RCT study design is considered the gold standard for causal inference, it is also criticized because RCTs often have homogeneous and small sample sizes due to inclusion/exclusion criteria, limiting generalizability to real-world application. Thus, additional methods are needed to draw causal inferences for public health. While causal inference is challenging and much debate exists, several models that provide promising support for a causal relationship between social connection and health have been applied.
The Bradford Hill guidelines are among the most widely adopted criteria for drawing causal inferences among variables unsuitable for randomization. These guidelines emphasize nine criteria: strength of association, consistency, specificity, temporality, biological gradient, plausibility, coherence, experiment, and analogy77. Reviews of the evidence on social connection and health have found support for nearly all the Bradford Hill criteria78-80. The only criterion not met was specificity, indicating that exposure to the potential cause (social connection) is associated with multiple outcomes rather than a particular outcome and no others. However, smoking also would not meet this criterion for causality, since it results in many health outcomes as well (e.g., cardiovascular disease, cancer). Indeed, Bradford Hill and proponents of these guidelines have noted that meeting all criteria is unnecessary; rather, the more evidence to support the criteria, the stronger the likelihood of causality77, 78. Nonetheless, critiques of the Bradford Hill guidelines point to the need for more sophisticated analyses.
Additional promising evidence exists to support potential causal associations beyond the Bradford Hill criteria. Drawing causal inferences may be appropriate from sophisticated regression analyses of longitudinal observational data81, applying a data-integration framework82, and Mendelian randomization83. While few studies focusing on indicators of social connection and health have employed these methods, those that do are supportive14. Thus, reviews of this evidence have concluded that the cumulative evidence supports the likelihood of a causal association between better social connection and better health5, 78, 80.
Despite considerable strengths in the evidence, several notable gaps remain in our knowledge. Some gaps became glaringly apparent during the COVID-19 pandemic, when the scientific community struggled to answer basic questions for the broader public, such as: How much socializing is needed for health benefits? How soon do adverse mental and physical health consequences emerge when we lack social connection? Is there equivalence between in-person and remote means of socializing? What can we do to reduce loneliness? Indeed, there are likely many more questions for which we do not have adequate or firm answers at the moment.
While there are many strengths in our current body of evidence, gaps in this evidence may become barriers or limit our ability to translate this evidence into practice. To address these gaps more comprehensively, Table 1 provides an overview of some of the strengths and challenges currently existing in the evidence base, further pointing to where future efforts may be prioritized.
| Strengths of evidence | Challenges | Priority needs |
|---|---|---|
| Converging evidence across scientific disciplines | Variability in conceptualization and measurement | A multi-factorial approach is needed. |
| Many validated assessment tools |
Variability in assessment tools limits comparisons across time, or different samples. Validated instruments may not be generalizable to other cultures, settings, and contemporary modes of socializing. |
Consistency of assessment to establish prevalence rates and track trends. Improve or create new measures that are valid, reliable and acceptable. |
| Dose-response of social connection across the lifespan | Most research and attention are on extreme risk and older adults. | A focus across the risk trajectory (including prevention) and across ages is needed. |
| Converging evidence across social connection components | Fewer studies examine multiple components in the same sample. |
Further evidence of potential independent, additive and synergistic effects is needed to assess risk more precisely. Further evidence is needed on how each factor may differentially influence different kinds of outcomes. |
| Evidence on mortality is consistent across causes of death, country of origin, gender, and health status | Fewer studies include or differentiate: comprehensive health outcomes, low- and middle-income countries, marginalized groups, varying modalities of socializing (e.g., in-person, remote, non-human). | Basic research to fill these gaps is needed. |
| Robust evidence of mortality and objective health consequences |
Weaker and mixed evidence on effective strategies to mitigate risk (weaker methodologies were employed; most interventions are individually focused; most interventions are targeted at those most severely affected). Less is known about other non-health outcomes. |
Evidence-based solutions: rigorous evaluations allowing for strong inference; interventions across the socio-ecological model; prevention and mitigation of risk earlier on in the risk trajectory. Evidence on more diverse outcomes (e.g., economic, civic engagement, education, incarceration). |
EXAMINATION OF TRENDS
Examining trends in prevalence rates, awareness and research on social connection, isolation and loneliness offers valuable insights into the trajectory of societal dynamics and the evolving evidence base. Tracking prevalence rates allows us to understand the scale of these phenomena, informing translation to application and practice. Concurrently, heightened or lack of awareness reflects the perceived importance of the significance and motivation to act upon social factors for mental and physical health.
These trends are both shaped by the evolving landscape of research and may reflect an uneven knowledge base. Collectively, they illuminate the evolving intersection between societal shifts, individual experiences, and the scientific understanding of the intricate connections between social dynamics and health outcomes. Staying attuned to these trends is essential for developing targeted interventions and policies that effectively address the challenges posed by social connection, isolation and loneliness in contemporary society.
Trends in society
Societal trends over the past several decades indicate that, as a population, we have become less socially connected and more isolated, and that a high proportion of the population is lonely.
Based on the available data, loneliness has generally shown little improvement over the last few decades, and may be getting worse. For example, a massive synthesis of 345 studies on emerging adults (ages 18-29), who completed the UCLA Loneliness Scale between 1976 and 2019, found that average loneliness levels linearly increased annually across the 43 years84. Furthermore, a meta-analysis of data from 113 countries concluded that a substantial proportion of the population in many countries experiences problematic levels of loneliness85.
According to the Gallup Global State of Connection survey, nearly a quarter (24%) of the global population reports feeling “very lonely” or “fairly lonely”, although there was variability across countries86. Of the 29 countries where at least one third of the population felt lonely, 22 were in Africa, four were in the Middle East, and three in South Asia. This also demonstrates that loneliness is not just a wealthy Western country issue, and may even be more severe in other areas of the world. However, inconsistent measurement tools and scoring methods have led to vastly different prevalence estimates. Notably, prevalence rates often favor one indicator (e.g., loneliness) over others, yet indicators may interact in meaningful ways. Thus, the prevalence of those who lack social connection in one or more ways may be far larger than any estimate of a single indicator.
Loneliness trends provide an incomplete picture of the state of social connection, and we must look at the other ways in which individuals and communities may lack connection. For example, data from the American Time Use Survey, regarding how Americans spend their day, demonstrate that, over the past two decades, Americans have spent more time in isolation and less time with household and non-household family members, friends, community engagement, and companionship87. Although the COVID-19 pandemic exacerbated these trends, social isolation was increasing, and engagement with family, friends and others (co-workers, neighbors, acquaintances) was declining for years prior to the pandemic. This is consistent with other trends, such as those documenting a decline in social capital and participation in religion88, 89, and changes in family structure (e.g., decline of extended families, rise of single-occupancy households)90 – many of which are seen globally.
Contemporary society in much of the world is evolving rapidly, likely contributing to our current trends and having important implications for the direction of the trends going into the future. Rapid shifts that may be relevant to social and population health include the increasing aging population, widespread adoption of remote working, increased automation, economic strain and inequity91, migration and mobility, mental health crisis among youth, rise in xenophobia, civil and political unrest, and environmental crises, all of which may potentially exacerbate trends concerning social connection.
These trends of declining social connection, combined with the evidence on the bidirectional associations with mental and physical morbidities, point to an urgent need to take action. Because multiple factors have been contributing to these trends, building over decades, simply returning to pre-pandemic levels of connection or reducing time on social media may only bring limited benefits.
Trends in scholarly attention
There are also striking trends in the scientific study of the topic. The surging interest in social isolation and loneliness is reflected in research, as demonstrated by the substantial increase of studies on this topic over recent years, potentially providing greater understanding and justification for action. Thus, understanding how loneliness and isolation have been studied over time may provide additional insight.
To examine publication trends, we first used the PubMed by Year search tool. Because of the diverse literature on social, mental and physical health outcomes, the search was limited to two social variables (loneliness and social isolation) and two health outcomes (depression and mortality). We further scanned additional scientific databases (including PsycINFO for depression) using the same social and health variables. The searches were limited to articles published in peer-reviewed academic journals between 1972 and 2023. The mortality search terms included “social isolation” OR “loneliness” AND “death and dying” or “mortality” or “mortality rate” or “mortality risk”. The depression search terms included “social isolation” OR “loneliness” AND “major depression”. PsychINFO also allows narrowing search by methodology: thus, we further used the search parameters “empirical”, “quantitative”, “longitudinal”, “prospective”, “retrospective”, and “clinical trial”.
All studies using those search terms were bracketed into time periods to determine how many articles populated by our search terms were published within each period. Studies published in the past two decades (2004-2023) were demarcated into 2-year periods (2004-2005, 2006-2007, 2008-2009, etc.), while studies published in 1972-2003 were grouped (31 years). Figure 2 graphically presents the number of studies on isolation and loneliness over the years.
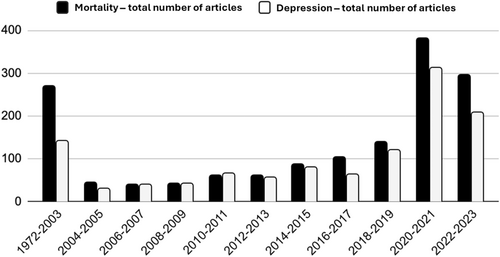
Data suggest an exponential increase in the scientific study of social isolation and loneliness. Over the past two decades, the number of relevant articles has grown, with significant increase since 2020. For example, the number of papers published in each subsequent two years since 2020 exceeds the number of studies from 1972 to 2003 combined. However, it is unclear whether scientific interest in other indicators of lacking social connection is similarly surging.
Trends in awareness
Several factors may presumably contribute to greater awareness of the importance of social connection and related aspects of lacking connection (i.e., social isolation and loneliness). These include scientific advancement, social media, government initiatives, the COVID-19 pandemic, and advocacy.
Significant advances in scientific research over the past few decades, especially in the last 5-7 years, may have shed light on the scale of the problem and provided greater confidence in scientific findings. Advancements in social technologies and the widespread use of social media platforms may have played a dual role in awareness. Increased experience of feelings of loneliness associated with that use, and the facilitation of awareness campaigns, discussions and support networks related to health and well-being may occur simultaneously92.
Government initiatives may have also played a role in greater awareness. Countries have recognized the urgency of the issue and appointed Ministers, formulated policies, and developed strategies to address loneliness and isolation, and highlight social connection as a priority. Awareness efforts have also been undertaken by national and international civil society organizations, coalitions, and networks that have emerged as powerful advocates7. These include the UK Campaign to End Loneliness, the Canadian Genwell Project, Australia's Ending Loneliness Together, and the annual Global Loneliness Awareness Week. These collective efforts aim to raise awareness, promote community engagement, and foster a culture of connection.
Unfortunately, trends in public awareness appear to be limited to only certain outcomes. A large survey of US and UK adults published in 2018 found that, when the public was asked to rank various factors contributing to a longer life (e.g., not smoking, exercising, limiting alcohol, maintaining a healthy weight), social connection was amid these factors, but it was rated among the lowest in importance, significantly underestimating its impact relative to effect sizes reported in the scientific literature93.
Due to a variety of factors occurring since that survey was published – i.e., the COVID-19 pandemic, national awareness campaigns, and increased prevalence within the population – public perception of the health relevance of social connection was expected to increase. However, 2023 data from the UK and a nationally representative sample of US adults demonstrate that there has been essentially no change94. Despite increases in public discourse on social isolation and loneliness, the importance of these and other aspects of social connection for health and survival are still underestimated among the public.
Implications from these trends
Overall, these trends point to a large and potentially increasing scale of those lacking social connection, and parallel trends suggest increasing attention within scholarship on the consequent impact on health. Yet, the public perception of risk does not align with either the increasing scale or evidence of the magnitude (effect sizes) for health. This suggests that increased education and awareness of the health relevance is needed.
Discrepancies between the scientific evidence and public perception may have significant implications. First, public perception may significantly influence how resources are allocated and prioritization of various issues within public health agendas95. If the public does not perceive social connection and markers of its deficit (e.g., loneliness and social isolation) as relevant to health93, funding and efforts may not be directed towards addressing them adequately, despite their demonstrated impact on health outcomes4, 15. Second, public perception influences individual behaviors and societal norms. If social connection is not widely recognized as a protective factor, and loneliness and isolation as serious health risks, individuals may be less likely to change their own behavior or support others experiencing loneliness or isolation96. This may perpetuate social disconnection and exacerbate the problem.
Finally, accurate awareness of the health implications among the public may facilitate destigmatizing the issue and promoting help-seeking behavior97. When people view loneliness and isolation as a personal rather than a health issue, they may be less inclined to seek support and resources to address these challenges. Aligning public perception with the evidence on the importance of social connection is essential to shaping effective policies, nurturing more connected and supportive communities, and promoting health.
CHALLENGES
The WHO defines health as “a state of complete physical, mental and social well-being, not merely the absence of disease or infirmity”98. Considering this definition, social well-being is a critical element of health that has been underappreciated and raises several challenges that we must address.
If physical and mental health are more than the absence of physical or mental illness, we should be taking a similar approach to social health. However, recent attention appears primarily focused on indicators of social deficits, specifically social isolation and loneliness. Yet, our collective and individual capacity as humans to think, feel, engage with others, pursue livelihoods, and experience fulfillment is intrinsically tied to our health – physical health, mental health and social health. The active encouragement, safeguarding and recovery of social health are crucial priorities for individuals, communities and societies globally.
Key challenges include developing a common language, identifying and activating appropriate and effective approaches, and adapting to societal changes. These challenges are also interconnected. Developing a common language is essential to understanding the underlying contributors, predicting outcomes, and measuring changes in risk and protection. Understanding these challenges helps us develop better approaches to preventing and mitigating risk, and adapt these approaches as society evolves.
A common language
Given the array of terms used in the scientific literature, one potential barrier to prioritization within health settings is lack of precision in terminology. It is clear that we need a common language, but the term “loneliness” may fall short. Loneliness is often used as a catch-all term outside academic scientific contexts, but it is defined and measured more narrowly within the scientific literature. While definitions of loneliness vary somewhat, there is broad consensus that it is distinct from social isolation7, 99.
Loneliness is a subjective, unpleasant feeling based on the discrepancy between one's desired and actual level of social connection100. It is most often distinguished from social isolation as a separate but related construct7. While isolation and loneliness can coexist, they differ in meaningful ways. Social isolation is objectively being alone, having few relationships or infrequent social contact. Thus, social isolation is objective, while loneliness is subjective. Although both social isolation and loneliness can be involuntary, isolation may be chosen101. Both are indicators of lacking social connection, but there are many indicators of social connection and, thus, many indicators of social connection deficits8. Social disconnection and loneliness are not equivalent43, and this has implications for measurement and assessment, intervention, policy, and more.
Across scientific disciplines, several constructs have emerged as relevant. Table 2, although not comprehensive, highlights some of the most widely used terms represented in the research and identified in the US Surgeon General Advisory4. Pinning down definitions is challenging, given that the same term has been used to refer to different things, while different terms are used to describe the same thing among studies. Some terms, such as social capital, lack a clear consensus on definition102, 103.
| Term | Definition |
|---|---|
| Loneliness | A subjective distressing experience that results from perceived isolation or inadequate meaningful connections, where inadequate refers to the discrepancy or unmet need between an individual's preferred and actual experience. |
| Social capital | The resources to which individuals and groups have access through their social connections. The term is often used as an umbrella for both social support and social cohesion. |
| Social cohesion | The sense of solidarity within groups, marked by strong social connections and high levels of social participation, that generates trust, norms of reciprocity, and a sense of belonging. |
| Social connectedness |
The degree to which any individual or population might fall along the continuum of achieving social connection needs. |
| Social connection | A continuum of the size and diversity of one's social network and roles, the functions that these relationships serve, and their positive or negative qualities. |
| Social disconnection | Objective or subjective deficits in social connection, including deficits in relationships and roles, their functions and/or quality. |
| Social infrastructure | The programs (such as volunteer organizations, sports groups, religious groups, and member associations), policies (such as public transportation, housing and education), and physical elements of a community (such as libraries, parks, green spaces, and playgrounds) that support the development of social connection. |
| Social isolation | Objectively having few social relationships, social roles, group memberships, and infrequent social interaction. |
| Social negativity | The presence of harmful interactions or relationships, rather than the absence of desired social interactions or relationships. |
| Social networks | The individuals and groups a person is connected to and the interconnections among relationships. These “webs of social connections” provide the structure for various social connection functions to potentially operate. |
| Social norms | The unwritten rules that we follow which serve as a social contract to provide order and predictability in society. The social groups we belong to provide information and expectations, and constraints on what is acceptable and appropriate behavior. Social norms reinforce or discourage health-related and risky behaviors (lifestyle factors, vaccination, substance use). |
| Social participation |
A person's involvement in activities in the community or society that provides interaction with others. |
| Social support | The perceived or actual availability of informational, tangible and emotional resources from others, commonly one's social network. |
| Solitude | A state of aloneness by choice that does not involve feeling lonely. |
Why is this important? These terms refer to related but distinct constructs. Reviews of this evidence find that these measures are not highly correlated empirically8, 104. Thus, when we only measure one of these, we cannot assume that we are capturing the full scope of how social factors influence health.
We need a common language. “Social connection” has been offered as an umbrella term to encompass these distinct but related terms4, 8, 15, 105. From this perspective, the myriad of diverse concepts in the scientific literature can be organized into three key themes or components: structure, function and quality. The first component, structure, represents the human need to have others in our life and is often measured by the size and variability of relationships within a network, being part of groups, and regular social interactions. It is the foundation upon which the other components of social connection are built. The second component, function, recognizes that these connections serve essential functions or purposes. Namely, connections can be relied upon for support to meet various needs and goals. Functions are often measured by the interchange of support that is received or perceived to be available, which can be emotional, informational or tangible, and can help us navigate life's challenges. The bulk of the studies within the scientific literature have primarily examined indicators of these structural or functional components. However, a growing body of research is assessing and recognizing the importance of the quality of social relationships, networks and interactions. Thus, the third component, quality, refers to our connections' positive and negative aspects. High quality is often measured by the level of satisfaction or intimacy, whereas low quality includes social negativity such as conflict, strain or ambivalence.
While Figure 3 is helpful in identifying these core conceptual themes, individual measurement approaches may overlap to some degree between social connection components. Furthermore, specific assessment tools may appear to align clearly within one component, but contain items that overlap with other components104. Generally, high levels of each of these components have been linked to better health and lower levels of poorer health. To more comprehensively understand underlying causes, predict outcomes, and measure risk, we need to consider the distinct contributions of the structure, function and quality of social connection.
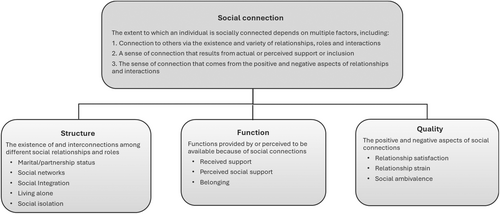
Data across multiple scientific disciplines have linked various social connection indicators to health outcomes8. Strong structure, function and quality of social connection may be considered optimal for health. On the contrary, when all three are low, this would be associated with high to severe risk. However, there may be unevenness in the extent to which any individual experiences the three components of social connection. The descriptions in Table 3 help illustrate the disaggregation across these components and their relation to various risk profiles. Nonetheless, there is likely further complexity of risk, given that many indicators within each component of social connection are on a continuum and may have synergistic effects. For example, longitudinal data from nearly half a million people, followed for an average of 12.6 years, demonstrated that low levels on both structural and functional indicators of social connection resulted in a significantly higher risk for cardiovascular disease mortality (hazard ratio, HR=1.63), compared to low levels on structural (HR=1.27) or functional (HR=1.17) components alone54.
| Risk level | Structure | Function | Quality | Description |
|---|---|---|---|---|
| Optimal-low risk | High | High | High | Large and varied social network, with regular social contact with people who can be relied upon for support and assistance when needed. These include deep and meaningful relationships characterized by caring and compassionate interactions. |
| Low-moderate risk | High | High | Low | Large and varied network, with regular contact among people who can be counted upon for support. However, these relationships are strained and/or lack depth, and interactions are void of caring or compassion. |
| High | Low | High | Large and varied network, with regular social contact with meaningful and high-quality relationships. However, these are not able or available to provide support or assistance when needed. | |
| Low | High | High | Small social network and infrequent contact. However, the limited social contact is among those who can be relied upon for support, perhaps strangers or volunteers. Nonetheless, it is caring and compassionate. | |
| Moderate-severe risk | High | Low | Low | Large and varied social network, and regular contact with others. However, they cannot be relied upon for support. These are strained relationships and interactions, with a lack of caring and compassion. |
| Low | High | Low | Small social network and limited social contact with others. Support is available and provided by others, perhaps by strangers or volunteers; however, it lacks depth, is accompanied by strain, or lacks caring and compassion. | |
| Low | Low | High | Small social network and limited social contact with others. It is not possible to rely upon others for support. However, the limited social contact is caring and compassionate. | |
| Severe risk | Low | Low | Low | Small social network and little social contact. There is no one to rely upon. What little social contact does occur is strained or lacks caring and compassion. |
Conceptually, loneliness may represent the signal or symptom of unmet social needs. However, loneliness does not represent low levels across all three social connection components. Comparisons demonstrate these distinctions. For example, meta-analyses that establish the effect size for the aggregate measures of social connection on mortality were significantly larger than the effect size for loneliness43, 105. Thus, loneliness is not the same as lacking social connection.
Measurement
Another challenge related to the need for a common language is the lack of consensus on measurement104. The most widely used measurement tools have helped to build a robust evidence base, but may have limitations when applied to other settings. For instance, most measurement tools were developed in Western countries, prior to the widespread shift to digital and remote means of socializing. Measurement not only needs to be predictive of the outcomes of interest, but must also be feasible to use. Notably, what is feasible may differ in different contexts, such as research, clinical settings, population surveillance, and evaluation of the effectiveness of interventions. Currently there is no measure that is multi-factorial, validated, and feasible or adapted to become feasible across settings.
Given the multi-factorial conceptualization of social connection7, 80, a considerable challenge is developing a feasible multi-factorial measure. Not all social connection components are typically assessed, because this would take too much time. Due to time and space constraints, assessments in medical settings and population surveillance may only assess one indicator; however, this approach will likely result in risk assessment errors. For example, if an individual is assessed on an indicator of the structural component of social connection (e.g., frequency of social contact) and found to have high levels, we may assume that this person is at low risk. However, this assessment may miss low levels on the other two components (e.g., low social support, poor quality relationships), which may put the individual at risk. Similarly, we might assume that this person is at low risk if scores are low on an assessment of loneliness, yet the person may have little or no social contact with others. Furthermore, if an individual is low on one component, we may be missing potential protection associated with high levels on the other components. Thus, one's overall social risk profile may be incomplete because of the limited scope of assessments.
Effective intervention and prevention strategies
The next major challenge is reducing risk through effective intervention and prevention strategies. Social connection is complex, with various factors contributing to its increase or decrease, directly and indirectly8. Generally, social connection occurs naturally among individuals and within communities. However, when it does not, intervention becomes necessary to reduce risk. Direct actions, programs or initiatives can be implemented to increase social connection or decrease forms of social disconnection intentionally.
Key challenges include: a) the capacity to develop and evaluate intervention strategies; b) the difficulties to understand what works best for whom in what context; and c) the limited scope of existing strategies, and the need to ensure the full scope of social connection across the socio-ecological model, sectors of society, and life course.
Developing and evaluating interventions
The evidence supporting the positive effects of social connection is far more robust and methodologically rigorous than the evidence supporting the effectiveness of interventions aimed at creating it when it is not occurring naturally, or at reducing social disconnection. However, this challenge (i.e., more substantial evidence of health risks compared to treatments to eliminate these risks) is common among many health issues. The National Institutes of Health estimate that therapeutics for any condition take, on average, 10-15 years to develop, because 95% of new therapeutics fail106. With the increased urgency to address the crisis of social isolation, loneliness and social disconnection, we cannot take a “something is better than nothing” attitude, assuming that all approaches will be helpful.
Rigorous evaluations are needed. However, the resources and capacity to develop and evaluate interventions are limited – particularly for interventions conducted outside academic institutions. Rigorous methodologies are often not utilized, resulting in a low-quality body of evidence107, 108. To strengthen this evidence, the Multiphase Optimization Strategy (MOST) approach has been utilized for other health issues and could similarly be applied to this area109. The MOST framework is an iterative implementation method that uses empirical information about component effects within real-world constraints to develop, evaluate and optimize interventions110.
Understanding what works for whom in what context
There is a growing body of evidence examining the effectiveness of interventions, including multiple meta-analyses and reviews of the evidence108, 111-116. Interventions vary in terms of their social connection focus (e.g., loneliness, social isolation, school connectedness, social skills, social support, neighborhood cohesion); setting (e.g., home, clinic, community, school, whole of society policies); delivery (e.g., self-directed, peer group, family or caregiver, professional, volunteer); modality (e.g., in-person, phone, virtually); sub-population group (e.g., older adults, children, disabled, university students, veterans, new parents), and many other characteristics.
Interventions also vary in their timing and duration (e.g., once or repeated, hours to years); their outcomes (e.g., social, health, performance); their target (e.g., general population, high-risk populations); and goals (e.g., prevention, mitigation, treatment). Effectiveness may depend on the specific characteristics of the targeted population, the type and intensity of the intervention, and its length15. This variation creates a considerable complexity. We highlight here the interventions with the most promising body of evidence.
Loneliness interventions
There is now a sizable body of research examining interventions focused specifically on reducing loneliness. Systematic reviews and meta-analyses generally find that these interventions are associated with significantly reduced loneliness and improved social support. For example, an umbrella review of 211 studies, including seven different types of interventions, examined their effectiveness in reducing loneliness116. They were befriending programs, technological interventions, meditation/mindfulness, animal therapy or robopets, social cognitive training, social skills training, and social support. Of these intervention types, social support, social cognitive training, and meditation/mindfulness significantly decreased loneliness.
Among loneliness interventions designed to target specific age-based sub-populations, there are meta-analyses of evidence for those focused on young people, university students, and older adults. A meta-analysis of 39 studies (including 25 RCTs) focused on loneliness in children and adolescents found that it could be reduced, with no significant differences between various types of interventions115. A systematic review of 37 interventions among university students found that bringing students together for an activity or to socialize, in-person or virtually, helped reduce feelings of loneliness117. Meditation/mindfulness benefited those who preferred not to join groups. Other reviews identify several effective interventions for reducing loneliness and increasing social connection in older adults, including social support groups, technology-based interventions, and community-based activities118, 119.
Overall, based on the current evidence, no intervention type (e.g., changing maladaptive social cognitions, enhancing social skills, providing psychoeducation, supporting socialization, increasing opportunities for social interaction) seems to be superior to the others. The majority of this evidence has been classified as low to critically-low quality116.
Interventions in clinical settings
Given the robust evidence of the medical relevance of social connection, addressing isolation and loneliness in clinical settings among patients may improve health outcomes. Early evidence pointed to greater survival among cancer patients who participated in social support groups along with standard treatment compared to standard treatment alone120. Since then, various types of programs have been developed to help support patients across different medical conditions, but with mixed outcomes. Nonetheless, when the body of the evidence was examined as a whole via meta-analysis, including 106 RCTs, medical patients randomized to receive some type of psychosocial support intervention in addition to standard medical treatment had a 20% increased survival, and 29% increased survival time compared to patients who only received standard treatment76.
While there was considerable variability in the effects among the interventions, on average, providing patients with psychosocial support was as effective in increasing survival as many standard medical interventions, including smoking cessation and lifestyle interventions. Thus, not only do high levels of naturally occurring social connection increase one's lifespan, but providing interventions to support patients in medical settings also seems to increase survival. This evidence suggests, consistent with NASEM recommendations, that addressing the social needs of patients by integrating this component into existing treatment within the health care system may be a promising approach15, 121.
Social prescribing
Social prescribing involves referring patients outside the medical setting to community-based services and activities to address social, emotional and practical needs. An integrative review of the evidence found that social prescribing has generally favorable effects in reducing social isolation and loneliness. However, the quality of the evidence was mixed and generally weak methodologically118. The interventions were diverse and heterogeneous in design and implementation, relied on self-report, and often lacked adequate controls.
While social prescribing is a promising approach gaining popularity, further research is needed, including RCTs and meta-analyses, as multiple other systematic reviews provide a weak or mixed picture122-124. More robust evidence is needed to understand how strong the effects are for individuals, sub-populations and communities regarding loneliness, isolation and social connectedness, and to identify the most effective approaches for different populations.
Technology-based or virtual interventions
Technology-based or virtual interventions – such as online social networking, video conferencing, messaging apps, and virtual companions or pets – are implemented with the aim of reducing social isolation or loneliness among specific populations. Systematic reviews of the evidence found that technology-based interventions were effective in reducing loneliness among older adults and individuals with mental health issues111, 125, 126.
The WHO has developed an evidence and gap map for technology-based interventions for reducing social isolation and loneliness among older adults127. This includes 200 studies and 97 systematic reviews. Most interventions utilized video conferencing and calls, though assistive robots and virtual pets were also common.
The effectiveness of digital interventions may vary depending on the specific population and the type of technology used. Caution should be used, given that some studies found no effectiveness and, in some cases, negative outcomes. For example, data from the National Social Life, Health and Aging Project found that, despite increases in remote modes of contact with others, individuals still experienced loneliness, depression and decrease in happiness128.
While some technology-based interventions may be promising, not all effectively reduce social isolation or loneliness. More research is needed to fully understand their effectiveness, for which groups, and how they can be optimally implemented.
School connectedness
There is strong evidence that interventions aimed at increasing school connectedness, or the feeling of belonging and engagement within the school community, can positively impact student outcomes, from academic achievement to reduced suicidality129-131. In one review, classroom management approaches were associated with improved school connectedness among students, including teacher caring and support, peer connection and support, student autonomy and empowerment, management of classroom social dynamics, teacher expectations, and behavior management132.
Research has shown that students who feel more connected to their school are more likely to attend class regularly, have higher grades and test scores, are less likely to engage in risky behaviors (e.g., substance abuse, violence), and have better health133-136. Classroom practices that build strong, supportive and trusting relationships help reduce patterns that inappropriately exclude some groups of kids132.
Policy
There is growing interest in the role of policy as an intervention, with many calls to enact pro-social policies, or policies to address isolation and loneliness4, 137-139. Policies are explicit guidelines which provide a framework for decision-making; are enforced by groups, organizations or governments; and can directly or indirectly impact social connection. Similar to the Health in All Policy approach that recognizes the health implications across sectors (e.g., education, employment, health, nutrition, housing, transportation)140, a “Social in All Policy” approach should recognize the social relevance of policies across sectors80, 138.
Policies can directly influence social contact (e.g., policies on visitation or family member involvement in medical care), or can focus on changing other kinds of outcomes (e.g., economic, environmental) that substantially influence social connection (e.g., policies on neighborhood zoning, bussing routes, remote work).
Reviews of existing policies cover social and emotional learning curricula in schools130, 141; state-level farmer wellness programs142; expansion of telehealth services to provide mental health services in schools143; and workplace policies that include shorter total work hours and earlier end of the workday, enabling workers to attend to family responsibilities and achieve greater work-life harmony144. There is existing US legislation, including the Older Americans Act of 1965, which was amended in 2020, to address social isolation and loneliness.
Many policies are being introduced with the intent to facilitate social connectedness. However, given the scale and magnitude of public health implications, they need to be evaluated for effectiveness like any other intervention.
Targeted vs. broad approaches
Another major challenge is whether to focus solutions on people most severely affected or broadly on the population. When social connection needs are not met, the mental and physical health consequences are broadly found across age and other demographics. However, isolation and loneliness are unequally distributed across the population. Groups that experience marginalization – i.e., lesbian, gay, bisexual, transgender, queer and/or questioning (LGBTQ+) people, racial minorities, migrants, those with disabilities91 – and life circumstances that may or may not co-occur with aging (e.g., functional or sensory impairments) are disproportionally affected. Thus, a significant challenge is whether to focus efforts more broadly or these groups.
One perspective is that prioritization should be given to the most vulnerable populations and addressing their needs. By focusing on specific populations, such as marginalized or underserved communities, efforts can be directed toward reducing health disparities and ensuring that resources reach those who need them the most145. Many sources recommend tailoring interventions to address specific needs, barriers and enablers within these groups, in order to increase the effectiveness of these interventions15, 146. This approach may be a more efficient use of limited resources, funding and personnel. Moreover, it is easier to measure the impact of targeted approaches, as they are narrowly defined and address a smaller population. However, identifying and targeting people “at-risk” may potentially pathologize and stigmatize such groups further and place the burden of change on the individual. Thus, it has been argued that we should focus on the factors that put people at risk instead of group membership147.
Another perspective is that we should focus efforts across the population to have larger shifts, rather than just targeting a small portion of the population77. Broad approaches can lead to systemic changes in policy, environment, and societal norms, laying the foundation for long-term health improvements. Implementing broad interventions might also benefit from economies of scale, reducing the cost per individual reached compared to targeted interventions.
Both targeted and broad approaches are necessary, starting with broad measures to address general issues, while using targeted interventions to address specific needs within the population. However, targeted approaches should be focused on the factors associated with risk (e.g., marginalization) rather than group membership, to avoid further stigmatization. Universal approaches may help prevent social disconnection, whereas more targeted approaches may be needed for those who are already isolated, lonely, or socially disconnected in other ways for prolonged periods or at severe levels. A hybrid strategy can leverage the strengths of both approaches to maximize public health outcomes.
Limited scope of existing approaches
Despite the growing body of research focused on interventions, the scope of solutions is limited in several ways. The Systemic approach Of Cross-sector Integration and Action across the Lifespan (SOCIAL) framework points to gaps and opportunities in solutions across the socio-ecological model, sectors of society, the life course, and prevention80.
Evidence points to underlying root causes across the socio-ecological model (e.g., individual, interpersonal, community, institution, society)8, yet most interventions are being deployed at the individual level148. A scoping review of interventions for older adults, including evidence from 30 countries, found that the majority of interventions only measured loneliness, and only three societal-level interventions were found149.
The health care sector, including both clinical and community health settings, is most often the target of interventions and programs. However, we need to expand our approaches across sectors to engage the whole of society. No one sector of society is likely to be able to address this issue. The “Social in All Policy” approach138 recognizes the health and social implications across sectors and “systematically takes into account the health implications of decisions, seeks synergies, and avoids harmful health impacts in order to improve population health and health equity”150.
Social connection is vital at every stage of life, yet most solutions are focused later in life111, 151. The evidence of a dose-response effect of social connection on biomarkers of health across stages of life46, and the importance of early social environment5, highlights the need for efforts to address this issue across life. Social isolation during childhood, for instance, is associated with increased cardiovascular risk factors in adulthood, such as increased blood glucose levels, high blood pressure, and obesity152.
As is the case with most health issues, primary, secondary and tertiary prevention approaches are needed to address social isolation and loneliness. Unfortunately, few interventions focus on helping the society become more socially connected. Prevention efforts may have many longer-term benefits, such as avoiding costly interventions later, reducing disease burden, and improving quality of life153.
Efforts to gather and synthesize data, and to identify evidence gaps, are underway. These and similar efforts aim to help create centralized resources to single out evidence-based interventions effective in reducing social isolation and loneliness, or increasing social connectedness. However, without sustained funding, there will be difficulties to evaluate the evidence supporting their effectiveness.
IMPLICATIONS FOR THE FUTURE OF MENTAL AND PHYSICAL HEALTH
The world is beginning to recognize the vital importance of social connection to the health and welfare of countries. Considering the trends that have led to concerns of a public health crisis of social disconnection, we must proactively evaluate the long-term implications if these conditions do not improve or perhaps continue to worsen. Two of the most pressing concerns that have the potential to worsen trends are the unknown long-term consequences of the COVID-19 pandemic and the rapidly evolving technological landscape of society.
Long-term implications of the COVID-19 pandemic
During the COVID-19 pandemic, social developmental processes were significantly disrupted, with potentially critical long-term health implications. Socialization during early life plays a crucial role in shaping a child's development and long-term health154. Early socialization provides the foundation for healthy relationships (e.g., learning to communicate, cooperate, negotiate, share), emotional well-being (e.g., learning empathy, expressing emotions), cognitive development (e.g., information processing, critical thinking, problem-solving), self-identity (e.g., self-confidence, self-esteem), ability to navigate cultural norms and values, and overall physical health155.
Early life experiences with caregivers, peers, schools and communities are all key contributors to the early social environment that ensures longer-term well-being and survival156-160. However, the pandemic severely limited socialization for roughly three years, during this critical developmental period, for infants, young children and adolescents. Since it is well documented that early social experiences significantly predict later social, mental and physical health136, 161, 162, the long-term health implications of the pandemic may be disproportionately borne for an entire generation.
There may also be longer-term consequences among adults, due to widespread behavioral adaptation that may be sustained over time. The massive adoption and implementation of tools to cope with reduced social contact (e.g., remote work, contactless delivery services, streaming entertainment services, telehealth, automation) came with significant advantages, including increased flexibility, autonomy, convenience, safety, and in some cases cost-effectiveness163-167.
These advantages have led to preferences that may limit our social contact – particularly with co-workers and weak-ties. Reductions in social contact with both may be critical factors for future health, given the significance of workplace relationships168, 169 and the evidence on the importance of weak-ties170, 171. While these preferences are obviously not universal, a large portion of the population values such conveniences. Even if they are not preferred, they are often incentivized by lower costs166. For example, roughly half of patients preferred in-person visits and half preferred a video visit, but 23.5% switched to a video visit if the cost was lower172. What was once initiated or scaled to help us cope with isolation, is now what may be reinforcing isolation, with potential long-term implications for exacerbating existing levels of social disconnection and corresponding health consequences.
The widespread behavioral adaptation to spending more time alone, or not leaving the house, may contribute to a societal shift that normalizes social isolation. This is increasingly being depicted in cultural narratives of a “social-battery” that is drained by socializing, and the benefits of “self-care”, “me-time”, and solitude. While there is evidence of some benefits of solitude173, the evidence is quite heterogeneous, and benefits appear limited to short-term bouts of solitude, not chronic time alone174, 175. There is instead – as we have seen – robust empirical evidence of the harmful effects of social isolation on mental and physical health outcomes, and increased risk for premature mortality. If time spent alone is praised and encouraged, while the risks of social isolation are diminished within public discourse, the consequences to health are likely to be magnified.
The pervasive experience of social isolation and loneliness during the pandemic also fueled self-proclaimed “experts” and influencers who pushed common-sense approaches to wellness, and in some cases misinformation176, 177. Coupled with a growing distrust in institutions, including science, this may lead to confusion on what is credible. When local community organizations and the general public are skeptical or distrust science, government, and each other, this may increase social disconnection and stifle the development and acceptance of effective interventions and programs to reduce isolation and loneliness.
Technological advancements
The rapid evolution of digital technologies has already demonstrated co-occurring shifts in socializing. Much has been written about the mental and physical health implications of the use of social media92, 178-183. Similar rapid developments and widespread adoption are occurring with artificial intelligence (AI) and large language models (LLM) tools, that have the potential to similarly result in both benefits and harms, but to an exponentially larger extent.
The long-term consequences of AI are yet unknown, but predictions often fall into either a utopian or dystopian outlook for the future, both of which have implications for social health and policy184. From a utopian perspective, AI will be the cure to the “loneliness epidemic”, with 24/7 access to emotional support for all, and increased automation will free up more time for leisure. From a dystopian perspective, AI will replace human interaction, and diminish trust in others due to blurred lines between fact and fantasy. Moreover, several jobs will no longer require humans, resulting in a lack of meaning and purpose in life, and perhaps even the risk of a downfall of humanity altogether185.
Some of the potential short-term benefits that already have some limited evidence involve AI-powered virtual companions or chatbots that can engage in conversation and provide immediate emotional support186, and 24/7 access to mental health support as well as increased accessibility among those experiencing barriers (e.g., language, privacy concerns, social anxiety) to in-person therapy. However, increased isolation may occur if there is over-reliance on AI interaction and emotional support and forming attachments to AI companions187, 188. Generative AI may also magnify our own biases, leading to information echo chambers that further isolate us from others189, 190.
Generative AI is neither inherently good or bad for health and humanity. Our current decisions and actions will starkly impact the trajectory of our future, extending across all sectors of society184.
Recommendations to reverse trends
Several countries are beginning to take steps to promote social connection, and the global COVID-19 pandemic crystalized and accelerated the urgency to act and to coordinate efforts. Table 4 provides a set of recommendations for national strategies to foster social connection and address social isolation and loneliness.
| Policy and strategy |
Make social connection a priority in policy agendas of governments and other organizations. Establish a national strategy and leadership at all levels to track, advance and coordinate policies and programs across agencies or units. Assemble an inter-agency, cross-sector coalition to assess and address social implications across all policies and programs. Establish a centralized resource or database for evidence-based interventions and policies. |
| Integration within the health system |
Prioritize social connection in prevention and integration into treatment in clinical settings. Assess and track risk within the electronic medical records. Adequate training, resources and support for health care providers. |
| Healthy digital environments |
Establish greater transparency and cooperation to independently evaluate drivers of connection and disconnection. Increase accessibility (access, affordability, knowledge) to digital tools and environments with demonstrated benefits. Establish safeguards (laws, regulations, guidelines, autonomy) to reduce risk associated with harmful elements. |
| Evidence, evaluation, measurement |
Creation of a global social connection index to allow for comparisons across nations. Establish consistent national measure of social connection, for population surveillance at a national level. Establish a national research and policy center/institute to coordinate cross-sector collaboration in research. Establish Grand Challenges in Social Connection Research, and funding to sustain efforts to address them. |
| Education and awareness |
Establish public-facing national awareness campaigns, ensuring accurate and inclusive messages based on high-quality evidence. Establish National Health Guidelines for Social Connection (similar to dietary guidelines). Include social connection in public-facing health educational resources (websites) of major health organizations. Integrate social connection into formal health education curriculum across all educational settings (primary, secondary, post-secondary, higher education, continuing learning, advanced and continuing education for health professionals). Establish age-appropriate formal education curriculum and practices to foster social connection skills. |
| Norms and culture |
Media, arts and entertainment, local and national leaders, and others in positions of influence, can model positive behaviors that facilitate connection (e.g., respect, openness, responsiveness, kindness, support) Create routines, habits and programs that reinforce regular social connection within formal (workplace, education) and informal (neighborhoods, recreation and leisure) settings. Strengthen norms, incentives and opportunities to create a culture of service. Establish coalitions and networks to coordinate efforts and share best practices. |
| Infrastructure |
Design physical places and spaces to foster socializing (e.g., public, commercial, recreational, religious). Design should consider features of accessibility and inclusiveness across ages, abilities, and economic circumstances. Evaluate existing infrastructure to identify barriers to social connection. Redesign, reduce or eliminate features of infrastructure that are barriers. Create pro-social policies, and evaluate existing policies for barriers relevant to infrastructure (e.g., zoning laws, investing in public transportation, housing and desegregation). Reform policies to allow for the use of existing underutilized public spaces (e.g., schools during nights and weekends, churches on weekdays, commercial buildings during off hours) for community social events and gatherings. Develop programs, services and resources (e.g., recreation, volunteer programs, senior centers, community gardens) to support more connected communities. |
These recommendations align with those made by the National Academy of Sciences, Engineering, and Medicine15, 27, 92, expert consensus documents and reports, the US Surgeon General Advisory4, the WHO191, the US Centers for Disease Control and Prevention192, the American Heart Association28, and national organ-izations or groups of states (e.g., European Union, UK, Australia, Japan)193-195.
CONCLUSIONS
In recent decades, we have witnessed a progressive decline in the social connectedness of individuals and communities at the global level. At the same time, scientific evidence has been credibly demonstrating a significant causal effect of lack of social connection on leading physical and mental health indicators, such as cardiovascular disease, stroke, depression and dementia80. In some cases, these associations are bidirectional, cyclically reinforcing poorer social connection and worse health. The strongest evidence documents an independent directional influence of social connection indicators on risk for disease-related and all-cause mortality, adjusting for a robust set of demographic, lifestyle, biological, and health relevant factors15, 54, 55. Furthermore, evidence points to several plausible biological, behavioral and psychological mechanisms through which these associations of social connection with morbidity and mortality may occur. The WHO now recognizes social connection as a global public health priority1, 13.
Despite significant strengths, the body of research evidence is complex and uneven, generating several challenges. We need a common language to describe and measure the multiple indicators of social connection and its deficits. Despite the use of “loneliness” as a catch-all term, this construct is distinct from other related ones (e.g., social isolation). There is convergence of evidence of the health relevance across indicators of social connection, or lack thereof. Nonetheless, the relative effect sizes vary in their magnitude. Social isolation appears to be a stronger predictor of physical health outcomes, while loneliness is a stronger predictor of mental health outcomes58. Further, the influence of poor social connection across its multiple components appears to be much stronger than that of only one component42, 54. Explicit recognition of the separate contribution of the structure, function and quality components of social connection is needed in measurement, risk assessment, and health promotion.
Recent surges in the scientific study of social isolation and loneliness have replicated and expanded upon earlier findings, providing larger sample sizes, more rigorous methodologies, and greater confidence. However, studies have also shown that the public underestimates the relevance of social connection for health relative to what has been documented in the scientific literature93, 94. Since awareness is a critical step to behavior change96, education efforts should be prioritized as part of health promotion.
There has been a proliferation of interventions with promising results, most often improvements in loneliness. These interventions vary widely in their approaches, foci, modalities and features; yet no one approach appears superior to others151. There are also important limitations worth noting. Most interventions are individually focused, and attention to prevention or early intervention is limited148. Furthermore, most reviews and meta-analyses of the evidence only examine the effectiveness of interventions on changing social outcomes (e.g., loneliness), with fewer also evaluating the effectiveness on changing health outcomes. Overall, the proposed interventions lack the level of scientific rigor of the evidence that supports their need.
Existing trends in social disconnection and declining health are likely to persist if social factors continue to get relegated as peripheral to health, and interventions are only aimed at people most severely affected. In the presence of growing trends of distrust in institutions, including science, identifying and implementing effective solutions may be challenging. Furthermore, long-term implications from the COVID-19 pandemic and evolving digital technologies point to potential worsening of existing trends in social disconnection.
Looking to the future, the trajectory of social, mental and physical health declines is unknown, but may be accelerated. Global scale reductions in social contact and subsequent behavioral adaptations may reinforce sustaining social isolation or have delayed downstream effects. Among infants, young children and adolescents, the limited social exposure at critical developmental stages may result in longer-term health consequences into adulthood. Across ages, behavioral adaptations through tools and mechanisms meant to cope with isolation (e.g., remote work, streaming entertainment, telehealth, contactless delivery) may instead sustain reduced social contact. Further developments in digital technologies, such as AI, have the potential to both help and exacerbate the problem.
Despite challenges, there is sufficient scientific evidence to prompt action. Importantly, themes have emerged prompting recommendations for individuals, communities and countries. Prioritizing these recommendations will be critical for reversing trends of social isolation and loneliness, and advancing social connection to positively influence the health and well-being of individuals and society at large.




