Effectiveness of a WHO self-help psychological intervention for preventing mental disorders among Syrian refugees in Turkey: a randomized controlled trial
Abstract
Refugees are at high risk of developing mental disorders. There is no evidence from randomized controlled trials (RCTs) that psychological interventions can prevent the onset of mental disorders in this group. We assessed the effectiveness of a self-help psychological intervention developed by the World Health Organization, called Self-Help Plus, in preventing the development of mental disorders among Syrian refugees experiencing psychological distress in Turkey. A two-arm, assessor-masked RCT was conducted in two Turkish areas. Eligible participants were adult Syrian refugees experiencing psychological distress (General Health Questionnaire ≥3), but without a diagnosis of mental disorder. They were randomly assigned either to the Self-Help Plus arm (consisting of Self-Help Plus combined with Enhanced Care as Usual, ECAU) or to ECAU only in a 1:1 ratio. Self-Help Plus was delivered in a group format by two facilitators over five sessions. The primary outcome measure was the presence of any mental disorder assessed by the Mini International Neuropsychiatric Interview at six-month follow-up. Secondary outcome measures were the presence of mental disorders at post-intervention, and psychological distress, symptoms of post-traumatic stress disorder and depression, personally identified psychological outcomes, functional impairment, subjective well-being, and quality of life at post-intervention and six-month follow-up. Between October 1, 2018 and November 30, 2019, 1,186 refugees were assessed for inclusion. Five hundred forty-four people were ineligible, and 642 participants were enrolled and randomly assigned to either Self-Help Plus (N=322) or ECAU (N=320). Self-Help Plus participants were significantly less likely to have any mental disorders at six-month follow-up compared to the ECAU group (21.69% vs. 40.73%; Cramer's V = 0.205, p<0.001, risk ratio: 0.533, 95% CI: 0.408-0.696). Analysis of secondary outcomes suggested that Self-Help Plus was not effective immediately post-intervention, but was associated with beneficial effects at six-month follow-up in terms of symptoms of depression, personally identified psychological outcomes, and quality of life. This is the first prevention RCT ever conducted among refugees experiencing psychological distress but without a mental disorder. Self-Help Plus was found to be an effective strategy for preventing the onset of mental disorders. Based on these findings, this low-intensity self-help psychological intervention could be scaled up as a public health strategy to prevent mental disorders in refugee populations exposed to ongoing adversities.
In 2020, the number of forcibly displaced people in the world, 80 million, was the highest since World War II1. Among them, 26 million fled their countries due to violence or persecution1. The largest group of refugees was from Syria, accounting for 6.6 million people. Around 3.6 million Syrian refugees are in Turkey, making Turkey the world's top refugee hosting country1.
Many Syrian refugees have been exposed to potentially traumatic experiences such as bombings, threats, captivity, torture, injury, and witnessing death or injury of loved ones2. Moreover, they are at risk of discrimination, economic problems, and social isolation. In 2020, the COVID-19 pandemic exacerbated Syrian refugees’ hardship in Turkey because of a sudden and severe deterioration in income generation opportunities and access to services and social supports3.
Owing to potentially traumatic events, major losses and other stressors before, during and after migration, refugees are at high risk of developing common mental disorders4. The World Health Organization (WHO) estimates that the rates of depression, post-traumatic stress disorder (PTSD) and any mental disorder among people exposed to conflict in the previous 10 years are 10.8%, 15.3% and 22.1% respectively5. Evidence suggests that Syrian refugees are at high risk of developing these disorders6.
A significant component of consensus-based humanitarian mental health policy and practice involves psychological interventions that aim to have preventive and health promotion effects2. However, evidence for such effects has been limited, and a recent Cochrane review did not identify any randomized studies assessing whether preventive psychological and social interventions can reduce the frequency of mental disorders in people affected by a humanitarian crisis7.
In recent years, the WHO has developed a series of brief transdiagnostic psychological interventions, including Problem Management Plus8 and Self-Help Plus9, which have been tested for treatment of mental health problems among people affected by adversity10-13. However, they have never been evaluated as indicated preventive interventions – i.e., they have not been tested among people who are distressed, but who do not meet the criteria for any mental disorder, to see whether they can prevent the onset of mental disorders.
In the present study, we examined the effectiveness of Self-Help Plus as an indicated intervention to prevent the onset of mental disorders among distressed Syrian refugees in Turkey.
METHODS
Study design
The study was an assessor-masked, parallel-group randomized controlled trial (RCT). The trial protocol was published and registered at clinicaltrials.gov (NCT03587896)14. The study was approved by the WHO Ethics Review Committee and the Ethics Committees of Istanbul Sehir University and Koc University. Written informed consent was provided by all participants.
Participant recruitment occurred from October 1, 2018 to November 30, 2019 in Istanbul and Mardin, Turkey. Six-month follow-up assessments ended in June 2020.
Local non-governmental organizations (NGOs) implementing projects for refugees in Turkey were approached to identify potentially eligible participants. These NGOs provide integrated reception services that include food, housing; legal, educational, health care and social guidance and support; and programs to promote socioeconomic inclusion and integration. Participants were consecutively invited to participate by members of the research team, in agreement with local service staff, who facilitated contacts.
All research team members were Arabic-speaking. They were trained in conducting the interviews, administering the rating scales, and performing follow-up assessments, so that they were able to assist the persons in a culturally appropriate manner. Research team members followed a code of conduct, complying with the principles of neutrality, impartiality, confidentiality, demeanor, and avoiding activities that might lead to a conflict of interests. All research-related training activities were coordinated by the WHO Collaborating Centre of the University of Verona, Italy.
Randomization and masking
Participants were randomly assigned either to the Self-Help Plus arm (consisting of Self-Help Plus combined with Enhanced Care as Usual, ECAU) or to ECAU only, in a 1:1 ratio. Randomization was centralized and coordinated by the Verona WHO Collaborating Centre.
The randomization schedule was generated by Castor Electronic Data Capture (EDC) software15, employing variable block randomization. Research team members involved in recruitment were able to access the web-based software to randomize each newly enrolled participant, but were not able to access the randomization list, and were not aware of the block size. Castor EDC software allowed random allocation only after the main information on the enrolled participant was entered, upon verification of the inclusion criteria. After random allocation, the software produced a unique identification number for each participant.
Both assessors evaluating outcomes and the statistician performing analyses were masked to participant allocation status. Outcome assessors were not involved in any activities that might reveal random allocation of study participants. A formal assessment of the success of masking was not conducted, as there is no methodological consensus on whether such tests are appropriate, reliable and truly informative16.
Inclusion and exclusion criteria
Participants were included if they met the following criteria: a) aged 18 years or older; b) able to speak and understand Arabic; c) being under temporary protection according to Law on Foreigners and International Protection; d) experiencing psychological distress, as shown by a score of 3 or more on the 12-item General Health Questionnaire (GHQ-12)17, 18; e) having completed oral and written informed consent to enter the study.
Exclusion criteria were: a) presence of any mental disorder according to the Mini International Neuropsychiatric Interview (MINI)19, 20; b) evidence of acute medical conditions contraindicating study participation; c) evidence of imminent suicide risk, or suicide risk scored as “moderate or high” on the MINI; d) signs of impaired decision-making capacity emerging from responses during the clinical interview. Refugees who were excluded because of a diagnosis of a mental disorder and/or imminent suicide risk were referred for treatment to a health professional.
Experimental and control intervention
The Self-Help Plus intervention consists of a pre-recorded audio course, delivered by trained facilitators in a group setting and complemented with an illustrated self-help book adapted for the target cultural group. The intervention is based on acceptance and commitment therapy, a form of cognitive behavioural therapy. It is delivered across five 2-hour sessions. The audio material imparts key information about stress management and guides participants through individual exercises and small group discussions. The self-help book reviews all essential content and concepts.
In this study, a version of the intervention previously adapted for Syrian populations was used. The adaptation followed a WHO protocol and involved adapting the audio recordings to a colloquial form of Arabic widely understood in Syria, and culturally adapting the illustrations.
As Self-Help Plus is a pre-recorded intervention, fidelity checking primarily involved ensuring that all of the recordings were played and all activities (e.g., discussions, exercises) were completed. Fidelity forms were completed after each session by facilitators. Additionally, 20% of all sessions were checked using the same forms by external trained supervisors.
ECAU was provided to participants in both groups, and consisted of routinely delivered social support and/or care. Additionally, participants in the control arm received baseline and follow-up assessments according to the study schedule, information about freely available health and social services, and links to community networks providing support to refugees.
An independent Ethics Advisory Board, consisting of international experts giving advice on any relevant ethical issues, supervised the study.
Measures
The primary outcome was the presence of current mental disorders at six-month follow-up, ascertained by the MINI19, 20. The MINI was also administered at baseline before randomization, and at post-intervention. All other assessment instruments measured secondary outcomes at post-intervention and at six-month follow-up.
Psychological distress was measured using the GHQ-12 questionnaire17, 18, in which items are rated on a four-point Likert scale, giving a maximum total score of 36. PTSD symptoms were assessed by the PTSD Checklist for DSM-5 (PCL-5)21, 22, a 20-item questionnaire giving a maximum total score of 80. Depression symptoms were measured by the Patient Health Questionnaire, nine-item version (PHQ-9)23-25, which gives a maximum total score of 27. Personally identified psychological outcomes were examined using the Psychological Outcome Profiles (PSYCHLOPS)26, 27, which asks participants to describe two problems from their own perspective and rate their severity on a six-point scale (maximum score: 18).
Functional impairment and subjective well-being were assessed by the WHO Disability Assessment Schedule 2.0 (WHODAS 2.0)28, and the WHO-5 Well-Being Index (WHO-5)29, 30, respectively. The WHO-5 contains five questions using a six-point scale (maximum score: 25). For evaluating general health, we administered the European Quality of Life 5-Dimensions 3-Level (EQ-5D-3L) questionnaire, a brief self-report measure consisting of five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression)31-33.
Traumatic/adverse life events and environmental stressors were explored using the Harvard Trauma Questionnaire (HTQ)-Part A34, 35 and the 17-item Checklist for Post-Migration Living Difficulties (PMLD)36. HTQ-Part A asks for lifetime traumatic life events. The PMLD asks respondents to rate their experience of the problems during the last 12 months on a five-point scale (from “not a problem” to “a very serious problem”).
Assessments were conducted as face-to-face interviews or remotely by telephone or secure online audio/video communication (for reasons of feasibility, including physical distancing requirements related to the COVID-19 pandemic). Adverse events reported spontaneously by the participants or observed by the research staff were recorded, reviewed by the Ethics Advisory Board in regular meetings, and reported to the WHO Ethics Review Committee.
Statistical analysis
We expected a frequency of mental disorders of 25% at six months in this population group14. We hypothesized that Self-Help Plus would show a clinically significant advantage by producing a between-groups absolute difference of 10%14. With these figures, to achieve at least 80% power for a 0.05 level of significance in a chi-square test, a sample size of 500 participants (250 per group) was needed. Assuming that a proportion of refugees might be lost at study endpoint (due to the specific characteristics of this population), a final sample size of 600 participants (300 per group) was planned.
Descriptive statistics were calculated on sociodemographic, pre-migration, migration and post-migration variables at baseline. Balance between treatment groups was checked calculating standardized mean differences (SMDs). SMD values of 0.1 and –0.1 were used as thresholds for imbalance37.
We followed an intent-to-treat approach for analysis of primary and secondary outcomes. The intent-to-treat population consisted of all randomized participants who completed baseline assessment, irrespective of the number of Self-Help Plus sessions received. To check the robustness of results, the primary outcome was also analyzed using a per-protocol approach, including only participants who completed at least three Self-Help Plus sessions.
The primary outcome was compared between the two groups using Cramer's V, together with a risk ratio (RR) and its 95% confidence interval (95% CI). A multivariate secondary analysis was performed through a Poisson regression model, with a robust error variance, to estimate RRs directly, and to explore the potential confounding effect of prognostic factors controlling for variables showing imbalance at baseline.
For each secondary outcome, a mixed analysis of covariance (ANCOVA) controlling for baseline scores, with robust standard errors and distinct variances for post-intervention and six-month follow-up, was performed. In addition to mixed models, a last observation carried forward (LOCF) approach was also used to account for missing observations at six months. Standardized coefficients were estimated with the Stata “stdBeta” command.
For each questionnaire, in case of missing items, we used the corrected item mean substitution method (i.e., the item mean across participants weighted by the subject's mean of completed items)38, using information from subjects belonging to the same treatment arm for the same follow-up time, through the Stata “hotvalue” command. The substitution was only performed if resulting in admissible values, and only for observations having less than 50% of missing items. As a sensitivity analysis, we re-ran our models without any data imputation.
The hypothesis that the experimental intervention had no effect on GHQ-12, PCL-5, PHQ-9, PSYCHLOPS, WHODAS 2.0, WHO-5 and EQ-5D-3L scores was tested by performing seemingly unrelated regression (SUR)39, in its modification to allow for unbalanced data through the Stata “suregub” command. SUR was performed for each time point, controlling for baseline values.
Possible interactions between treatment and specific variables (gender, age, years of education, length of stay in the hosting country) were evaluated. In particular, in the case of continuous outcomes, SUR for unbalanced data on all outcomes was performed, with their value at baseline, treatment status, all potential moderators, and their interactions with treatment status as predictors. A global test on all interaction terms was implemented and, in case of significance, the same test was performed for each scale. Finally, for scales meeting the statistical significance threshold, single regressions were conducted.
As for binary outcomes, to avoid the issue of poor performance of the model in case of solutions near the boundary40, Poisson regression models were performed with robust standard errors, setting as regressors the variable “intervention allocation”, each variable separately, and their interaction with treatment. The Bonferroni correction was used to take into account multiple testing.
Multivariate analyses were performed for each secondary outcome to take confounding factors into account, again including the baseline value as a covariate. Finally, lost-to-follow-up was compared between the two groups using a chi-square or a Fisher exact test, as appropriate. All analyses were performed using Stata/SE, Release 15.141.
RESULTS
After screening 1,186 potentially eligible participants, 544 were excluded. A total of 123 were excluded because their level of distress was below the established cut-off, 282 because of a positive MINI, and 139 for other reasons (e.g., mental health was not a priority for them or they were not available to receive the intervention) (see Figure 1). This left 642 individuals who met the inclusion criteria, consented to be randomized, and were randomly allocated to either Self-Help Plus (N=322) or ECAU (N=320).
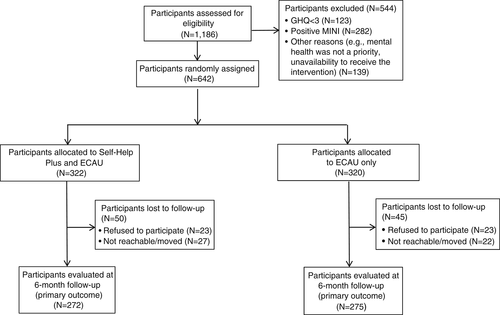
At six-month follow-up (primary outcome), we could not assess 95 individuals (14.8%). They were lost to follow-up because they refused to participate (N=46) or because they were not reachable and/or moved to other locations (N=49). The distribution of participants lost to follow-up was similar between the study groups (15.53% vs. 14.06%, Cramer's V = 0.021, p=0.601; RR=1.104, 95% CI: 0.761-1.602).
The main sociodemographic characteristics of the included participants are shown in Table 1. Their mean age was 31.5±9.0 years; 62.9% of them were women. For 61.8% of them, primary school was the highest level of education, while 14.5% received academic education. Almost all participants came from Syria (628 of 642, 97.8%). The remaining 14 participants came from Iraq (N=11), Yemen (N=1), or occupied Palestinian territory (N=1). One additional participant did not consent to reveal this information. The mean age at departure was 27.1±10.1 years. A minority of participants (5.2%) experienced detention during their transition to Turkey.
| SH+ | ECAU | Difference (standard error) | SMD | |
|---|---|---|---|---|
| Age (years, mean±SD) | 31.22±8.89 | 31.73±9.16 | –0.508 (0.712) | –0.040 |
| Gender (% females) | 63.98 | 61.88 | 0.021 (0.038) | 0.031 |
| Education (years, mean±SD) | 8.94±3.72 | 9.12±3.73 | –0.173 (0.300) | –0.033 |
| Type of education (%) | ||||
| Illiterate | 5.28 | 2.50 | 0.028 (0.015) | 0.102 |
| Primary school | 62.73 | 60.94 | 0.018 (0.038) | 0.026 |
| High school | 16.46 | 20.00 | –0.035 (0.030) | –0.065 |
| University | 14.60 | 14.38 | 0.002 (0.028) | 0.004 |
| Not reported | 0.93 | 2.19 | –0.013 (0.010) | –0.072 |
| N. relatives (mean±SD) | 5.04±3.71 | 4.87±2.27 | 0.168 (0.250) | 0.039 |
| N. children (mean±SD) | 2.73±1.89 | 2.73±1.92 | 0.002 (0.157) | 0.001 |
| Age at departure (years, mean±SD) | 26.91±11.13 | 27.20±8.96 | –0.295 (0.804) | –0.021 |
| Detention during transition (%) | 5.00 | 5.38 | –0.004 (0.018) | –0.012 |
| Months of detention (mean±SD) | 10.89±23.00 | 8.27±19.33 | 2.620 (9.051) | 0.087 |
| Total HTQ score (mean±SD) | 4.35±4.00 | 4.12±3.56 | 0.229 (0.299) | 0.043 |
- SMD – standardized mean difference, HTQ – Harvard Trauma Questionnaire
Assessment of 20% of Self-Help Plus sessions showed that all the components of the intervention were delivered in line with the manual. No adverse events related to the study participation were reported. In addition to Self-Help Plus sessions or ECAU, participants received minimal health care during the study period, which did not differ between the two groups (see supplementary information).
Differences between study conditions on primary and secondary outcome measures are reported in Table 2. Analysis of the primary outcome revealed that Self-Help Plus arm participants were significantly less likely to meet criteria for a mental disorder at six-month follow-up (59/272, 21.69%) compared to ECAU participants (112/275, 40.73%) (Cramer's V = 0.205, p<0.001, RR=0.533, 95% CI: 0.408-0.696). The mental disorders at follow-up were major depressive disorder (51/272 participants in the Self-Help Plus group and 94/275 participants in the ECAU group), PTSD (16/272 vs. 35/275), anxiety disorders (10/272 vs. 20/275), obsessive-compulsive disorder (three participants in the Self-Help Plus group) and bipolar disorder with psychotic features (one participant in the ECAU group). By contrast, at post-intervention, the frequency of any mental disorders was similar in the two groups (p=0.784) (see Table 2).
| Frequency of mental disorders | SH+ | ECAU | Cramer's V | p | RR (95% CI) |
|---|---|---|---|---|---|
| Baseline | 0/322 (0%) | 0/320 (0%) | |||
| Post-intervention | 30/237 (12.66%) | 36/267 (13.48%) | 0.012 | 0.784 | 0.939 (0.598-1.475) |
| 6 months (primary outcome) | 59/272 (21.69%) | 112/275 (40.73%) | 0.205 | <0.001 | 0.533 (0.408-0.696) |
| Secondary outcomes | Coefficient | p | Standardized coefficient (SE) | ||
| GHQ-12 score (0-36), mean±SD | |||||
| Baseline (N=642) | 17.363±4.519 | 16.776±4.299 | |||
| Post-intervention (N=503) | 12.657±4.947 | 13.491±5.101 | –0.974 | 0.028 | –0.096 (0.044) |
| Six months LOCF (N=574) | 13.269±4.825 | 13.768±4.548 | –0.578 | 0.139 | –0.062 (0.042) |
| PCL-5 score (0-80), mean±SD | |||||
| Baseline (N=640) | 20.724±14.904 | 20.138±14.278 | |||
| Post-intervention (N=504) | 16.824±12.831 | 14.814±14.597 | 1.754 | 0.134 | 0.063 (0.042) |
| Six months LOCF (N=574) | 13.991±11.454 | 15.085±12.855 | –1.278 | 0.195 | –0.052 (0.040) |
| PHQ-9 score (0-27), mean±SD | |||||
| Baseline (N=642) | 6.449±4.696 | 6.299±4.725 | |||
| Post-intervention (N=503) | 5.241±4.905 | 5.324±5.124 | –0.196 | 0.648 | –0.020 (0.043) |
| Six months LOCF (N=574) | 4.928±5.048 | 6.694±5.455 | –1.842 | <0.001 | –0.173 (0.040) |
| WHO-5 (0-100), mean±SD | |||||
| Baseline (N=642) | 42.458±24.418 | 43.591±23.766 | |||
| Post-intervention (N=504) | 50.903±24.599 | 48.494±23.520 | 2.743 | 0.196 | 0.057 (0.044) |
| Six months LOCF (N=574) | 52.143±21.709 | 49.320±22.670 | 3.154 | 0.085 | 0.071 (0.041) |
| WHODAS 2.0 (12-60), mean±SD | |||||
| Baseline (N=638) | 18.418±7.282 | 17.924±7.089 | |||
| Post-intervention (N=501) | 15.380±4.705 | 15.561±6.477 | –0.205 | 0.665 | –0.018 (0.041) |
| Six months LOCF (N=570) | 14.804±4.787 | 14.269±4.261 | 0.488 | 0.190 | 0.054 (0.041) |
| PSYCHLOPS score (0-20), mean±SD | |||||
| Baseline (N=488) | 9.422±5.592 | 8.911±5.269 | |||
| Post-intervention (N=388) | 6.230±5.727 | 6.890±5.640 | –1.071 | 0.104 | –0.091 (0.056) |
| Six months LOCF (N=543) | 4.852±5.375 | 6.168±6.499 | –1.215 | 0.036 | –0.100 (0.047) |
| PMLD score (0-68), mean±SD | |||||
| Baseline (not measured) | - | - | - | - | - |
| Post-intervention (N=501) | 16.569±11.022 | 18.864±12.689 | |||
| Six months (N=524) | 13.422±10.451 | 12.322±11.536 | 1.824 | 0.075 | 0.080 (0.045) |
| EQ-5D-3L score, mean±SD | |||||
| Baseline (N=627) | 0.718±0.275 | 0.720±0.282 | |||
| Post-intervention (not measured) | - | - | - | - | - |
| Six months (N=513) | 0.857±0.218 | 0.799±0.250 | 0.067 | 0.001 | 0.147 (0.044) |
- SH+ – Self-Help Plus, ECAU – Enhanced Care As Usual, RR – risk ratio, SE – standard error, LOCF – last observation carried forward, GHQ-12 – General Health Questionnaire, 12-item version, PCL-5 – PTSD Checklist for DSM-5, PHQ-9 – Patient Health Questionnaire, 9-item version, WHO-5 – WHO-5 Well-Being Index, WHODAS 2.0 – WHO Disability Assessment Schedule 2.0, PSYCHLOPS – Psychological Outcome Profiles, PMLD – Checklist for Post-Migration Living Difficulties, EQ-5D-3L – European Quality of Life 5-Dimensions 3-Level
Compared with ECAU, Self-Help Plus was also associated with improvements at six-months for the secondary outcomes of depression symptoms (p<0.001), personally identified psychological outcomes (p=0.036), and quality of life (p=0.001). Psychological distress as measured with the GHQ-12 showed a significant improvement in favor of the Self-Help Plus group at post-intervention only (p=0.028) (Table 2). These results were confirmed by global statistical significance of the intervention on all secondary outcomes by performing SUR (p=0.005 at post-intervention, p<0.001 at 6 months).
The intent-to-treat analysis results were confirmed by the per-protocol analysis. Self-Help Plus arm participants were significantly less likely to meet criteria for a mental disorder at six-month follow-up (47/218, 21.56%) compared to ECAU participants (112/275, 40.73%) (Cramer's V = 0.204, p<0.001, RR=0.529, 95% CI: 0.396-0.708) (see supplementary information for other results).
Results of secondary analyses of continuous outcomes conducted without any imputations of missing values were comparable to those of our main analyses. Secondary analyses accounting for baseline imbalance between groups did not identify relevant differences with respect to our main analyses on either primary or secondary outcomes (see supplementary information).
We investigated possible heterogeneity of the effect of treatment on outcomes by testing for interactions between intervention allocation and potential moderators. None of the interactions reached the statistical significance threshold for binary outcomes after applying the Bonferroni correction. By performing SUR on post-intervention secondary outcomes, a global test on all interactions of the variable “intervention allocation”, with center and the potential moderators on all regressions, was not significant (p=0.292). Similarly, none of the interactions for continuous outcomes reached the significance threshold at 6 months (p>0.05 in all cases).
DISCUSSION
To the best of our knowledge, this is the first prevention RCT conducted among refugees experiencing psychological distress but without a mental disorder7. We found that the likelihood of having a mental disorder at six-month follow-up was approximately half for Self-Help Plus vs. ECAU participants, and that such risk reduction appeared to be consistent across the most common diagnoses, i.e. depression, PTSD and anxiety disorders. Consistent with this, Self-Help Plus participants also showed improvements in depression symptoms, personally identified psychological outcomes, and quality of life at six-month follow-up. We did not detect significant differences between the Self-Help Plus and control groups on any outcome measure immediately post-intervention, with the exception of psychological distress.
Four out of ten participants in the control group developed a mental disorder. This very high frequency may be explained by events occurring during the study. First, before completion of six-month assessments, in October-November 2019, Operation Peace Spring was launched in northern Syria at the border with Mardin, a Turkish area where most study participants lived. The aim was to create a safe zone where Syrian refugees could be resettled42. However, this event caused fears of deportation, and this stressor may have increased the risk for mental disorders. Second, many six-month follow-up assessments were completed during the first lockdown period to control COVID-19 pandemic in 2020, which led to the cutting off of core services and income generating activities for refugees, causing severe economic hardships and adversity43.
Though there is limited information on the psychological effects of COVID-19 pandemic among refugees in Turkey, a prospective study with displaced populations in Iraq indicated a substantial increase in their depression, anxiety and PTSD during the pandemic44. Refugees settled in countries where existing services have not been well-established are even more vulnerable to financial and psychosocial problems when new crises arise. Within this context, the Self-Help Plus intervention may have been particularly beneficial in tackling severe and ongoing stress and adversities.
The positive impact of Self-Help Plus at six-month follow-up is in line with previous studies indicating an incubation effect in acceptance and commitment therapy trials45, 46. However, an RCT among asylum seekers and refugees resettled in Western European countries, conducted following a similar protocol on a smaller sample of participants, did not report this pattern of findings, possibly because it did not reach the target sample size47. In addition, participants in the Western European trial might have faced different stressors as compared with the present sample, which was exposed to severe and persistent stress throughout the follow-up period.
The results of the present study consolidate recent research evidence showing that prevention programs can be effective in reducing mental health problems. For example, a recent meta-analysis of 50 prevention trials indicated that psychological interventions can reduce the incidence of depressive episodes by 19%48.
This study has some limitations. First, as for most RCTs of psychological interventions, a double-blind design was not feasible. However, outcome assessors were masked, and they were not involved in any trial phase that might reveal random allocation. In addition, both participants and assessors were instructed not to mention any interventions received during the study. Second, we had to switch from face-to-face to remote (online or telephone) assessments due to the COVID-19 pandemic during follow-up. It is unclear if this change, which equally applied to both study arms, might have affected the participants’ responses. Even though several studies documented that a careful and culturally appropriate use of available instruments is feasible and allows a standardization of the screening process and a systematic recognition of psychological distress and psychiatric diagnoses6, formal studies on online or telephone use of these tools in refugee groups are lacking. Third, at baseline we did not assess the history of any previous mental disorder. Consequently, mental disorders at follow-up could include both new cases and recurrences of previous mental disorders.
Considering the size of the effect observed in the present study, and that Self-Help Plus can be provided by briefly trained peer non-specialist facilitators in large groups of up to 30 participants at a time, we suggest that it could be offered to forced migrants to support and improve their functioning, and to decrease the pressure on mental health services. Moreover, the use of an illustrated guide and audio recording for delivery decreases the need for extensive training and supervision of facilitators, while increasing intervention fidelity.
In the light of these advantages, Self-Help Plus could be scaled up as a public health strategy to prevent mental disorders in refugee populations exposed to ongoing adversities. Since the intervention does not address the determinants of the refugees' mental health problems, it should be applied in tandem with strong advocacy for protection of those who face adversity, and for services that address their social, physical and broad mental health needs.
ACKNOWLEDGEMENTS
This work was supported by the European Commission (grant agreement no. 779255). The authors are grateful to peer facilitators and co-facilitators who delivered the Self-Help Plus intervention, and to all the assessors who administered baseline and follow-up interviews. The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the WHO. M. van Ommeren and C. Barbui are joint senior authors of the paper. Supplementary information on the study is available at http://doi.org/10.23728/b2share.8ac4f28d2415413e89de7847c05471fc.




