Increased Early Post-Discharge Mortality in Patients With Acute Pancreatitis
ABSTRACT
Background
Emerging evidence suggests that individuals who recover from acute pancreatitis may face a significant risk of mortality during the early post-discharge period. Despite these concerns, comprehensive population-based studies on this issue are lacking.
Objectives
To study in-hospital and post-discharge mortality in patients with acute pancreatitis and how it has changed over time.
Methods
In a Danish nationwide population-based cohort study, we included all adults discharged after an incident episode of acute pancreatitis between 2002 and 2017. For each patient, five individuals from the general population, matched by age and sex, were selected as controls. We used Cox regression analysis to assess all-cause mortality at 90 days, 1, 2, and 5 years post-discharge and to examine trends in in-hospital and post-discharge mortality over the study period. Models were adjusted for comorbidities, heavy smoking, alcohol abuse and sociodemographic factors.
Results
Of 28,759 adults with incident acute pancreatitis, 956 (3.3%) died in hospital. The 27,803 patients discharged from the hospital following an incident episode of acute pancreatitis were matched with 139,035 individuals (mean age 58.1 years, 51.1% men). The cumulative post-discharge mortality at 90 days was 5.0% for the acute pancreatitis cohort and 0.55% for controls. The mortality risk was significantly increased in acute pancreatitis patients at 90 days post-discharge (adjusted hazard ratio [aHR] 7.62; 95% CI 6.86–8.45); the risk attenuated over time but remained elevated for up to five years (aHR 1.85; 95% CI 1.79–1.92). In-hospital mortality decreased over the study period (aHR 0.65; 95% CI 0.53–0.81) from 2002–2005 to 2014–2017, while post-discharge mortality risk remained stable (aHR 0.85; 95% CI 0.72–1.01). Gastrointestinal and cardiovascular diseases accounted for 59.4% of 90-day post-discharge deaths.
Conclusions
In-hospital mortality for acute pancreatitis has improved in recent years. However, the risk of post-discharge mortality remains high, especially in the first 90 days after discharge.
Graphical Abstract
Summary
-
Summarise the established knowledge on this subject
- ◦
Severe acute pancreatitis has high mortality.
- ◦
Management advances have lowered in-hospital mortality, but post-discharge mortality remains a concern.
- ◦
Population-based data on both in-hospital and post-discharge mortality are limited.
- ◦
-
What are the significant and/or new findings of this study?
- ◦
In-hospital mortality for acute pancreatitis has decreased by 35% over the past 16 years and is now 3% in a population-based setting.
- ◦
Mortality during the first 90 days post-discharge is 5% in a population-based setting.
- ◦
Gastrointestinal and cardiovascular diseases contribute to a significant number of post-discharge deaths, which may be amenable to treatment.
- ◦
1 Introduction
Acute pancreatitis is the most common gastrointestinal inflammatory disease requiring acute hospitalisation [1]. Most patients with acute pancreatitis experience a mild self-limiting form that resolves in a few days. However, about 20% develop moderate to severe pancreatitis characterised by necrosis of pancreatic or peripancreatic tissue, organ failure, or both. These patients face a significant mortality rate of 20%–40% [2, 3]. The unfavourable prognosis has spurred substantial research to prevent disease progression and reduce in-hospital mortality. Hence, over recent decades, the management of acute pancreatitis has evolved, shifting from surgical interventions to a minimally invasive step-up approach [4]. This development has likely reduced in-hospital mortality and morbidity, but population-based data are lacking.
Despite advancements in the in-hospital management of acute pancreatitis, the post-discharge period has received less attention. However, accumulating evidence indicates that patients are at a high risk of developing metabolic complications after discharge [5-7]. In addition, a recent multicentre study from Hungary highlighted an increased risk of post-discharge death [8]. The heightened risk stems from various causes, including malignancies, cardiovascular diseases, and complications related to acute pancreatitis itself. These findings hold clinical significance, as early detection and management of complications could potentially mitigate non-malignant causes of death. Thus, the post-discharge period may present a critical window for improving mortality risk in acute pancreatitis and warrants further studies [8]. However, current knowledge on post-discharge mortality following acute pancreatitis remains limited, with a lack of population-based studies available.
We hypothesise that in-hospital mortality in patients with acute pancreatitis has improved and that patients are at an increased risk of death after discharge, with the highest risk occurring during the early post-discharge period. Utilising nationwide Danish health registries, we aim to investigate i) in-hospital and post-discharge mortality in a population-based setting, ii) time trends in in-hospital and post-discharge mortality, and iii) causes of death in the early (90-day) post-discharge period.
2 Materials and Methods
2.1 Study Design and Data Sources
This is a nationwide matched cohort study including all incident cases of acute pancreatitis in Denmark between 1 January 2002, and 31 December 2017. Figure S1 provides an overview of the study design.
All residents in Denmark are assigned a unique civil registration number, facilitating the linkage of personal data across nationwide health registers [9]. Information was gathered by combining data from the Civil Registration System, the Danish National Patient Registry, the Danish Cancer Registry, the Danish Cause of Death Registry, the National Prescription Registry, the Danish Education Registry, and the Income Statistics Registry.
The Civil Registration System, established in 1968, comprises data on sex, date of birth, dates of migration, and vital status of permanent residents in Denmark [9]. The Danish National Patient Registry, established in 1977, encompasses all hospital admissions, including outpatient and emergency visits since 1995, with diagnoses coded using the International Classification of Diseases version 10 (ICD-10) since 1994 [10]. The Danish Cancer Registry was established in 1943 and records all cancer diagnoses in Denmark [11]. The Danish Cause of Death Registry registers causes of death according to ICD-10 standards [12]. Since 2002, the Automated Classification of Medical Entities system has automatically identified underlying causes from physician-reported codes on death certificates. Established in 1995, the Danish National Prescription Registry captures data on prescribed medications dispensed at pharmacies, ensuring high accuracy due to legal documentation requirements [13]. The Danish Education Registry provides data on the educational attainment of all residents [14]. Finally, the Income Statistics Registry provides income data from 1970 onward [15].
2.2 Acute Pancreatitis Cohort
We identified a cohort of patients hospitalised with a diagnosis of acute pancreatitis (ICD-10: K85) between 1 January 2002, and 31 December 2017, from the Danish National Patient Registry. We excluded individuals with any previous diagnoses of acute pancreatitis (K85), pancreatic cancer (C24.1 or C25 (excluding C25.4)), chronic pancreatitis and pancreatic exocrine diseases (K86), and those who had undergone pancreatic resection or transplantation (KJLC00-KJLC50, KJLC96 or KJLE) from 1 January 1994, until the admission date (Supporting Information S1: Table S1). Additionally, patients below 18 years at the time of admission were excluded. This method follows a previously published algorithm [16]. For in-hospital mortality, the index date was the admission date; for post-discharge mortality, it was the discharge date. Figure 1 presents a flowchart.
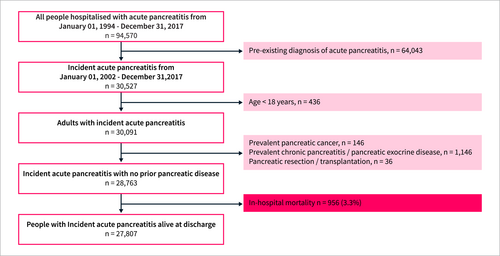
Flowchart of the acute pancreatitis study population.
2.3 Matched Comparison Cohort
Using the Civil Registration System, we identified individuals from the general population who matched each patient in the acute pancreatitis discharge cohort by sex and birth year and were alive on the patient's index date. We randomly selected five individuals per patient, sampling with replacement to allow multiple matches [17]. Comparison subjects had no history of pancreatitis, pancreatic cancer, other pancreatic exocrine diseases, or pancreatic surgery prior to being matched with acute pancreatitis patients (Supporting Information S1: Table S1) [16]. Individuals developing acute pancreatitis during follow-up were transferred to the acute pancreatitis cohort and censored from the comparison group.
2.4 Outcomes
The primary outcome was post-discharge all-cause mortality, obtained from the Civil Registration System. Patients discharged after an incident admission with acute pancreatitis were followed from the index date until death, emigration, or the end of follow-up (31 December 2018), whichever occurred first. Additionally, we investigated time trends in in-hospital mortality and 90 days post-discharge mortality. Furthermore, we explored cause-specific post-discharge mortality, including deaths from cardiovascular diseases, infectious diseases, gastrointestinal diseases, pancreatic cancer, other cancers, and other causes. The causes of death were obtained from the Danish Cause of Death Registry using ICD-10 codes (Supporting Information S1: Table S1) and have been described in prior studies [18].
2.5 Baseline Characteristics
Baseline characteristics were collected from six years prior to the index date until the index date (Figure S1). Data on age and sex were obtained from the Civil Registration System, while comorbidities and medications were sourced from the Danish National Patient Registry and the National Prescription Registry. We identified obesity, cholelithiasis, diabetes, nonfatal major cardiovascular events, and treatments involving antihypertensives, antithrombotics, and statins (Supporting Information S1: Table S1). Moreover, the Charlson Comorbidity Index (CCI) was derived from ICD-10 codes obtained from the Danish National Patient Registry and the National Cancer Registry (Supporting Information S1: Table S2) [19]. Smoking status was assessed using tobacco-related ICD-10 codes and prescriptions for tobacco dependency or obstructive pulmonary diseases for individuals over 40, following the methodology of previous studies [20]. Alcohol abuse was estimated using a diagnosis of or prescriptions for conditions associated with alcohol-related diseases or abuse [20]. Data from the Danish Education and Income Registries identified socioeconomic factors. Education was classified as high school or less versus beyond, while annual income was classified as low (under 30,000 USD), normal (30,000–75,000 USD), and high (over 75,000 USD).
2.6 Statistical Analysis
Baseline characteristics are reported as medians (interquartile range [IQR]), means (standard deviation [SD]), or counts (percentages). We analysed mortality risk at 90 days, one, two, and five years post-discharge. Survival probabilities at 90 days and five years post-discharge were estimated using the Kaplan–Meier method. We used Cox proportional hazard regression models to determine crude and adjusted hazard ratios (HR) with 95% confidence intervals (CI). For the multivariate analysis of all-cause mortality, adjustments were made for age, sex, CCI, heavy smoking, alcohol abuse, income, and education. In the analysis of time-period effects, we used 2002–2005 as the reference period, with models adjusted for the same covariates as in the primary analysis. Data on causes of death at 90 days post-discharge are presented in a graphical analysis, and time trends were analysed using a trend analysis for proportions. In a supplementary analysis, we calculated incidence rates for all-cause mortality at 90 days, one, two, and five years post-discharge. We compared incidence rates using Poisson regression models adjusted for the same covariates as in the main analysis (Supporting Information S1: Table S3). Finally, as a sensitivity analysis, we explored the impact of hospital stay duration on post-discharge mortality. The cohort was stratified into two groups: hospital stays ≤ 7 days and more than 7 days [21]. Mortality risk at 90 days, one, two, and five years post-discharge was analysed using Cox proportional hazards regression models, with adjustments consistent with those used in the primary analyses (Supporting Information S1: Table S4 and S5). A two-sided p-value of less than 0.05 was considered statistically significant. All data management and statistical analyses were conducted using SAS 9.4 (SAS Institute), Stata 17.0 (Stata Corp), and R 4.3.2 (R Development Core Team). Statistics Denmark provided anonymised data for this study under Project Identifier 708466. Access is restricted to authorised research institutions approved by the Danish Health Data Authority.
3 Results
3.1 In-Hospital Mortality
During the study period, 28,763 adult patients with no previous history of pancreatic diseases were hospitalised with an incident episode of acute pancreatitis, of whom 956 died during hospitalisation (in-hospital mortality: 3.3%, 95% CI [3.1% to 3.5%]) (Figure 1). Demographic and clinical characteristics of the admission cohort are detailed in Supporting Information S1: Table S6. The mean age was 58.6 years, and 50.9% were men.
3.2 Post-Discharge Mortality
The 27,807 patients discharged from the hospital alive comprised the acute pancreatitis discharge cohort, which was matched on age and sex to 139,035 comparison subjects from the general population (Figure 1). The mean (SD) follow-up time was 5.5 (7.3) years for the acute pancreatitis cohort and 6.3 (7.4) years for the comparison cohort.
Baseline characteristics are provided in Table 1. The mean age in both cohorts was 58.1 years, and 51.1% were men. Compared with the comparison cohort, patients with acute pancreatitis had a higher burden of comorbidities and were more likely to abuse alcohol and smoke.
| Acute pancreatitis | Comparison subjects | |
|---|---|---|
| Individuals, n | 27,807 | 139,035 |
| Calendar period of index date | ||
| 2002–2005, n (%) | 6100 (21.9) | 30,500 (21.9) |
| 2006–2009, n (%) | 5816 (20.9) | 29,080 (20.9) |
| 2010–2013, n (%) | 7306 (26.3) | 36,530 (26.3) |
| 2014–2017, n (%) | 8585 (30.9) | 42,925 (30.9) |
| Age, mean (SD) years | 58.1 (18.0) | 58.1 (18.0) |
| Age category (years), n (%) | ||
| 18–29 | 2004 (7.2) | 10,030 (7.2) |
| 30–39 | 3112 (11.2) | 15,522 (10.9) |
| 40–49 | 4367 (15.7) | 21,912 (15.7) |
| 50–59 | 5046 (18.1) | 25,176 (18.1) |
| 60–69 | 5312 (19.1) | 26,632 (19.2) |
| 70–79 | 4493 (16.2) | 22,380 (16.1) |
| ≥ 80 | 3473 (12.5) | 17,383 (12.5) |
| Female sex, n (%) | 13,605 (48.9) | 68,025 (48.9) |
| Comorbidities | ||
| Heavy smoking, n (%) | 6852 (24.6) | 21,179 (15.2) |
| Alcohol abuse, n (%) | 4386 (15.8) | 3511 (2.5) |
| Obesity, n (%) | 1953 (7.0) | 2557 (1.8) |
| Cholelithiasis, n (%) | 9726 (35.0) | 2149 (1.5) |
| Diabetes, n (%) | 3345 (12.0) | 9373 (6.7) |
| Nonfatal major cardiovascular events, n (%) | 1847 (6.6) | 5481 (3.9) |
| Charlson comorbidity index category, n (%) | ||
| 0 | 16,596 (59.7) | 110,738 (79.6) |
| 1–2 | 8257 (29.7) | 23,364 (16.8) |
| > 2 | 2954 (10.6) | 4933 (3.5) |
| Concomitant medication | ||
| Antihypertensives, n (%) | 13,976 (50.3) | 52,794 (38.0) |
| Antithrombotics, n (%) | 7812 (28.1) | 29,502 (21.2) |
| Statins, n (%) | 6335 (22.8) | 26,053 (18.7) |
| Socioeconomic factors | ||
| Highest completed education, n (%) | ||
| ≤ High-school graduate | 21,217 (76.3) | 96,667 (68.8) |
| > High-school graduate | 5182 (18.6) | 36,054 (25.9) |
| Unknown | 1408 (5.1) | 7314 (5.3) |
| Income group, n (%) | ||
| Low | 8251 (29.7) | 32,912 (23.7) |
| Normal | 16,106 (57.9) | 78,636 (56.6) |
| High | 3438 (12.4) | 26,835 (19.3) |
| Unknown | 12 (≤ 0.1) | 652 (0.5) |
During the five-year follow-up period, 5494 deaths occurred in the acute pancreatitis cohort, and 13,545 deaths occurred in the comparison cohort (Table 2). The cumulative risk of death for patients discharged after acute pancreatitis was 5.0% (95% CI: 4.8%–5.3%) at 90 days and 19.8% (95% CI: 19.3%–20.2%) at 5 years (Figure 2). Patients with acute pancreatitis had an increased risk of death compared with the comparison subjects within the first 90 days post-discharge (adjusted HR [aHR] 7.62; 95% CI 6.86–8.45); the risk attenuated over time but remained elevated after 5 years (aHR 1.85; 95% CI 1.79–1.92) (Table 2).
| Acute pancreatitis (n = 27,803) | Comparison subjects (n = 139,035) | Crude | Adjusteda | |||||
|---|---|---|---|---|---|---|---|---|
| Post-discharge | Events, n (%) | Person-years | Events, n (%) | Person-years | HR (95% CI) | p | HR (95% CI) | p |
| 90 days | 1395 (5.02) | 6618 | 767 (0.55) | 34,145 | 9.33 (8.55–10.19) | < 0.001 | 7.62 (6.86–8.45) | < 0.001 |
| 1 year | 2472 (8.89) | 26,051 | 3226 (2.32) | 137,098 | 4.01 (3.81–4.23) | < 0.001 | 3.39 (3.19–3.60) | < 0.001 |
| 2 years | 3467 (12.47) | 49,767 | 6234 (4.48) | 264,822 | 2.94 (2.83–3.07) | < 0.001 | 2.47 (2.36–2.60) | < 0.001 |
| 5 years | 5494 (19.76) | 104,967 | 13,545 (9.74) | 568,434 | 2.19 (2.12–2.26) | < 0.001 | 1.85 (1.79–1.92) | < 0.001 |
- a Adjusted for age, sex, Charlson comorbidity index, heavy smoking, alcohol abuse, income, and education.
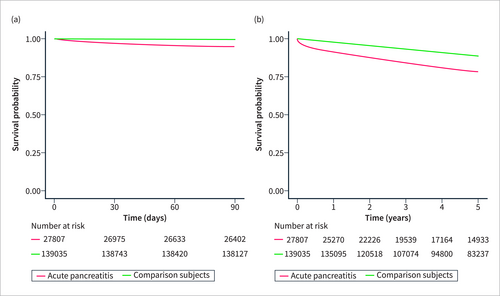
Kaplan–Meier survival curves for patients with acute pancreatitis and comparison subjects. (a) 90-day post-discharge survival probability. (b) 5-year post-discharge survival probability.
The primary analyses showed that the difference in post-discharge mortality risks between acute pancreatitis patients and comparison subjects decreased over time, potentially challenging the Cox model's proportionality assumption. However, the supplementary analysis of all-cause mortality incidence rates yielded results consistent with the primary analysis (Supporting Information S1: Table S3).
In sensitivity analyses stratified by the duration of hospitalisation, the 90-day post-discharge mortality risk remained significantly higher compared with the comparison cohort. Patients with longer hospital stays ( > 7 days) had slightly higher adjusted hazard ratios (aHR 8.56; 95% CI: 7.12–10.30) than those with shorter stays ( ≤ 7 days) (aHR 6.96; 95% CI: 6.15–7.88). The differences in risk between the subgroups were minimal, suggesting that the duration of hospital stay had limited influence on post-discharge mortality. Consistent with the primary analyses, the risk attenuated over time for both subgroups but remained elevated at five years post-discharge (Supporting Information S1: Tables S4 and S5).
3.3 Time Trends in Mortality
In Supporting Information S1: Table S6, baseline characteristics stratified by calendar period are reported for acute pancreatitis patients at admission. Comparing the first period (2002–2005) to the last period (2014–2017), patients became slightly older, had more comorbidities, and were more likely to smoke. In-hospital mortality risk significantly decreased over the study period, remaining stable from 2002 to 2009 and gradually declining for those diagnosed thereafter. Using 2002–2005 as a reference, the aHR for in-hospital death was 0.74 (95% CI 0.60–0.92) for patients diagnosed in 2010–2013 and 0.65 (95% CI 0.53–0.81) for patients diagnosed in 2014–2017 (Table 3).
| Period | No. at risk | Events | Person-years | Crude | Adjusteda | ||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | ||||
| In hospital mortality | |||||||
| 2002–2005 | 6388 | 288 | 176 | 1.00 | 1.00 | ||
| 2006–2009 | 6054 | 238 | 150 | 0.97 (0.81–1.15) | 0.698 | 0.95 (0.77–1.17) | 0.654 |
| 2010–2013 | 7526 | 220 | 193 | 0.77 (0.64–0.92) | 0.005 | 0.74 (0.60–0.92) | 0.005 |
| 2014–2017 | 8795 | 210 | 172 | 0.72 (0.60–0.86) | < 0.001 | 0.65 (0.53–0.81) | < 0.001 |
| 90 days post-discharge mortality | |||||||
| 2002–2005 | 6100 | 299 | 1451 | 1.00 | 1.00 | ||
| 2006–2009 | 5816 | 280 | 1383 | 0.98 (0.83–1.16) | 0.831 | 1.06 (0.84–1.22) | 0.900 |
| 2010–2013 | 7306 | 366 | 1740 | 1.02 (0.88–1.19) | 0.793 | 0.94 (0.79–1.12) | 0.474 |
| 2014–2017 | 8585 | 450 | 2042 | 1.07 (0.92–1.24) | 0.375 | 0.85 (0.72–1.01) | 0.058 |
- a Adjusted for age, sex, Charlson comorbidity index, heavy smoking, alcohol abuse, income, and education.
In Supporting Information S1: Table S7, baseline characteristics stratified by calendar period are reported for acute pancreatitis patients at discharge, showing similar patterns of change over the study period as the admission cohort. The 90-day post-discharge mortality risk did not significantly change over time. Using 2002–2005 as a reference, the aHR for 90-day post-discharge mortality was 0.94 (95% CI 0.79–1.12) in 2010–2013 and 0.85 (95% CI 0.72–1.01) in 2014–2017 (Table 3).
3.4 Causes of Deaths
Among the 1395 deaths observed within 90 days from acute pancreatitis discharge, 647 (46%) died from gastrointestinal diseases, 62 (4.4%) from infectious diseases, 182 (13%) from cardiovascular diseases, 55 (3.9%) from pancreatic cancer, 197 (14%) from non-pancreatic cancers and 252 (18%) from other causes (Figure 3a and Supporting Information S1: Table S8).
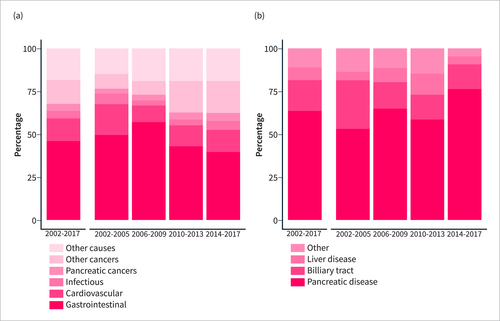
Causes of death within 90 days post-discharge for acute pancreatitis patients, presenting overall trends and stratification by calendar periods. (a) Overall causes of death. (b) Gastrointestinal causes of death.
During the study period, the most remarkable change in causes of death was a decreasing proportion of patients dying from gastrointestinal diseases (p = 0.021) and an increased proportion of patients with non-pancreatic cancers (p < 0.001). No significant differences were observed in time trends for the other causes of death (Figure 3a). Focussing on gastrointestinal diseases, pancreatic disease emerged as the leading cause of death, followed by conditions affecting the biliary tract, liver diseases, and other gastrointestinal causes (Figure 3b and Supporting Information S1: Table S9).
4 Discussion
We present population-based estimates of in-hospital and post-discharge mortality risks for patients hospitalised with incident acute pancreatitis. The in-hospital mortality rate was 3.3%, while the early (90-day) post-discharge mortality rate was 5%. After adjusting for relevant confounders, patients discharged after acute pancreatitis had an almost eightfold higher risk of death during the 90-day post-discharge period compared with a matched cohort from the general population. Over the study period (2002–2017), the in-hospital mortality risk declined by 35%. However, there was no significant change in the 90-day post-discharge mortality risk. Analysis of post-discharge deaths showed that nearly 60% of deaths were due to gastrointestinal or cardiovascular diseases, which may potentially be prevented with timely diagnosis and management.
4.1 In Hospital Mortality
The in-hospital mortality risk of 3.3% observed in our study is consistent with findings from previous studies [8, 22-24]. The Hungarian Pancreatic Study Group found a mortality of 3.5% in a large multicentre study, while a global prospective study across 90 centres reported a similar 30-day mortality of approximately 3% [8, 23]. A multicentre study in Spain showed a slightly higher in-hospital mortality of 4%, whereas a retrospective study from the United States reported a lower mortality of 1% [22, 24]. Our study, along with the previous studies, highlights a relatively consistent in-hospital mortality in acute pancreatitis across diverse cohorts and study designs.
4.2 Post-Discharge Mortality
The post-discharge mortality risk observed in our study is moderately higher compared to that reported from a multicentre study conducted by the Hungarian Pancreatic Study Group [8]. The cumulative incidence of death in our study was 5.0% at 90 days and 8.9% at 1 year; in the Hungarian study, the corresponding numbers were 3.0% and 5.5% [8]. The higher mortality observed in our study may be explained by the differing time periods and settings between studies. Hence, our study included a longer and earlier observation period (2002–2017) compared to the Hungarian study (2012–2021). Given significant advancements in managing acute pancreatitis over decades, the higher mortality rate in our study may reflect a time-period effect [4]. This is supported by the decline in in-hospital and (albeit insignificantly) post-discharge mortality observed in our study. Further, patient selection may explain some of the differences in mortality risks. The population-based setting with essentially complete follow-up in our study differs from the design of the Hungarian study, which was based on a multicentre database with a potential risk of selection bias. Consistent with our findings, other studies also show a moderately increased risk of death for patients discharged after acute pancreatitis, both during short- and long-term follow-up [25, 26].
4.3 Time Trends in Mortality
An interesting observation from our study was the significant decrease in in-hospital mortality over the study period. Mortality declined by 35% between the first and last periods, with this reduction becoming evident from 2010 onwards. This trend coincides with the implementation of the minimally invasive step-up approach for managing severe acute pancreatitis [4, 27]. The decline in post-discharge mortality was less pronounced (approximately 15% and nonsignificant). The reasons behind this difference between in-hospital and post-discharge mortality cannot be determined conclusively from our study. While significant attention and improvements have been made in the in-hospital management of acute pancreatitis, the post-discharge period may have received comparatively less focus, leading to this observed gap in mortality reduction.
4.4 Causes of Death in the Early Post-Discharge Period
Analysis of death causes in the early (90-day) post-discharge period revealed that gastrointestinal and cardiovascular diseases accounted for almost 60% of the observed deaths. The Hungarian study reported comparable findings. However, the estimates cannot be directly compared due to differing practices in ascribing causes of death (register-based in our study vs. autopsy-based in the Hungarian study) [8].
The notably increased risk of gastrointestinal-related death post-discharge is likely associated with late complications of acute pancreatitis, such as infected necrotic collections and bleeding from nearby vessels. It is interesting to note that the risk of death from gastrointestinal diseases decreased during the study period, which may be related to improvements in in-hospital management of severe acute pancreatitis, which may also have affected post-discharge outcomes [27]. Despite this decline, the high risk of death from gastrointestinal diseases throughout the study period underscores the urgent need for strategies to detect complications early and intervene promptly to lessen the burden of post-discharge mortality.
The increased risk of cardiovascular death identified in our study is another important and potentially clinically actionable finding. Several factors may contribute to this observation. First, severe inflammatory or infectious diseases, such as influenza or gout, can raise the risk of ischaemic cardiovascular events shortly after symptom onset [28, 29]. Systemic inflammation is linked to the destabilisation of atherosclerotic plaques, which could explain these associations and may also contribute to the heightened short-term cardiovascular risk observed in acute pancreatitis patients in our study. Second, patients admitted with acute pancreatitis often receive substantial intravenous fluid therapy as part of their standard treatment [30]. This can lead to congestive heart failure in predisposed individuals, potentially increasing post-discharge cardiovascular mortality. Third, refeeding syndrome in malnourished acute pancreatitis patients and excessive fluid resuscitation can cause electrolyte disturbances, which might trigger fatal cardiac arrhythmias [31].
Pancreatic and non-pancreatic malignancies also contributed to early post-discharge mortality, with a slight increase observed throughout the study period. This aligns with broader trends in Western countries, where cancer has become one of the leading causes of death, alongside a rising incidence of pancreatic cancer [32, 33]. However, the clinical relevance of these findings is limited as the short time from acute pancreatitis to death suggests that these cancers were advanced.
4.5 Clinical Implications
Our study highlights the substantial burden of post-discharge mortality in patients with acute pancreatitis, particularly due to gastrointestinal and cardiovascular causes. Given the high mortality rate, especially in the early post-discharge period, targeted interventions are needed. While our study provides valuable insights into mortality risk on a population-based level, further research is necessary before clinical changes can be implemented. Prospective studies with detailed patient characteristics are essential to identify high-risk individuals and explore the specific causes of death, especially in the early post-discharge phase. Additionally, understanding the mechanisms linking acute pancreatitis to gastrointestinal and cardiovascular death will help guide prevention strategies, as these causes may be amenable to early intervention. The identification of high-risk patients could lead to the development of a discharge screening tool and targeted follow-up protocols, including enhanced monitoring and early interventions.
5 Strengths and Limitations
Several factors highlight the strengths of this study. First, the large and nationwide population-based setting. Second, Danish medical registries ensure comprehensive long-term follow-up. Third, registries are prospectively maintained for administrative purposes, providing a large study population and precise outcome estimates.
However, there are limitations. First, epidemiological studies are susceptible to the risk of misclassification. However, ICD-10 codes for acute pancreatitis have a validated positive predictive value of 97.3%, demonstrating a strong alignment with diagnoses confirmed by the revised Atlanta criteria [34]. Second, because of the strict definitions of cause-specific mortality, we were not able to determine the cause of death for a significant proportion of patients. Third, residual confounding may persist despite adjustments. Expanding the matching process to include comorbidities and other mortality-related factors could have addressed this issue but was not feasible in this study. However, the attenuating in-hospital mortality risk over time indicates that the observed associations with acute pancreatitis are likely not solely due to confounding. Fourth, our findings warrant replications in other populations where the cause of death in the post-discharge period may differ from those observed in our and the previously mentioned study from Hungary [8]. Fifth, a limitation of our study is the lack of data beyond 2018, which restricts our ability to assess the most current trends in post-discharge mortality. Lastly, details on acute pancreatitis severity, comorbidities, and patient factors were limited, hindering an in-depth investigation into post-discharge mortality risk factors. However, we used the duration of admission as a proxy for acute pancreatitis severity [21] and found that post-discharge mortality remained significantly increased regardless of the duration of admission. This suggests that factors other than pancreatitis severity influence the observed mortality risk.
6 Conclusions
Despite a decrease in in-hospital mortality over 16 years, the risk of mortality following discharge from acute pancreatitis is significantly elevated post-discharge, particularly within the first 90 days. A substantial proportion of deaths are attributed to gastrointestinal and cardiovascular diseases, which may be amenable to treatment. These findings highlight the need for further research and development of strategies to enhance post-discharge follow-up and management for individuals at high risk of death following acute pancreatitis.
Author Contributions
S.S.O. designed the study. L.D. performed data management and statistical analysis. S.S.O. and L.D. interpreted the data and wrote the article. C.C.K., M.E.C., and A.M.D. reviewed and edited the manuscript. L.D. and S.S.O. are guarantors responsible for data integrity and accuracy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
Statistics Denmark provided anonymised data for this study. Access is restricted to authorised research institutions approved by the Danish Health Data Authority.