Diagnostic accuracy of pan-enteric capsule endoscopy and magnetic resonance enterocolonography in suspected Crohn's disease
Abstract
Background and Aims
Magnetic resonance enterocolonography (MREC) and pan-enteric capsule endoscopy (CE) offers visualization of the entire gastrointestinal tract in a single examination. We examined the diagnostic accuracy of MREC and CE in patients with suspected Crohn's disease (CD).
Method
In a prospective, blinded, multicenter study, we included patients with clinically suspected CD. Patients were examined with MREC, CE, and ileocolonoscopy (IC) within 2 weeks. The primary outcome was per patient sensitivity, specificity, and diagnostic accuracy for ileocolonic CD. IC served as reference standard.
Results
153 patients were included in the study and IC, MREC, and CE was performed in 152, 151, 133 patients, respectively. CD was diagnosed with IC in 59 (39%) patients (terminal ileum (TI) 22, colon 20, TI and colon 17). The sensitivity and specificity for diagnosing ileocolonic CD with MREC was 67.9% (CI 53.7–80.1) and 76.3% (CI 65.2–85.3) (TI 76.9% and 85.6%; colon 27% and 93%) compared to 87.5% (CI 73.2–95.8) and 87.8% (CI 78.2–94.3) with CE (TI 96.6% and 87.5%; colon 75.0% and 93.0%). The sensitivity of CE was superior to that of MREC (p = 0.02). The patient experienced discomfort was equal with CE and MREC and significantly less than with IC.
Conclusion
In patients with suspected CD, CE has a high sensitivity for diagnosing CD in the TI and colon, which is superior to that of MREC. The sensitivity of MREC for diagnosing CD in the colon is poor. CE could be a patient-friendly alternative to IC in selected patients with suspected CD.
Registered at ClinicalTrials.gov: NCT03134586.
Key summary
Summarize the established knowledge on this subject
-
Ileocolonoscopy is the recommended first line examination in clinically suspected Crohn's disease (CD); however, disease assessments require multiple tests due to the segmental inflammation throughout the gastrointestinal tract in CD.
-
Magnetic resonance imaging (MRI) and capsule endoscopy are established modalities for detection of small bowel CD.
-
Previous studies on the diagnostic accuracy of ileocolonic CD with MRI and capsule endoscopy is primarily on patients with established CD.
-
The diagnostic accuracy of MRI and capsule endoscopy for suspected ileocolonic CD is undetermined.
What are the significant and/or new findings of this study?
-
In suspected ileocolonic Crohn's disease, the sensitivity of capsule endoscopy is high and superior to MRI.
-
The sensitivity of MRI for diagnosing early Crohn's disease in the colon is poor.
-
The image quality did not affect the diagnostic accuracy of capsule endoscopy.
-
Capsule endoscopy could be an alternative to ileocolonoscopy in selected patients with suspected CD.
INTRODUCTION
Crohn's disease (CD) is an idiopathic chronic inflammatory bowel disease characterized by transmural inflammation with a segmental distribution. The disease may affect any part of the gastrointestinal tract, although most patients have CD located in the terminal ileum and/or colon.1 Hence, ileocolonoscopy (IC) is the first line diagnostic procedure in patients with suspected CD. Regardless of findings at IC an additional examination of the small bowel is recommended.2 IC is invasive and reaching the terminal ileum is not always possible.2, 3 Although significant adverse events such as bleeding and perforation are rare (<0.1%),4 up to one third of the patients experience minor adverse events, for example, abdominal pain and bloating.5
Recent technological advances in gastrointestinal imaging and endoscopy have greatly improved modalities for pan-enteric, non-invasive and patient-friendly diagnosis of CD. Magnetic resonance imaging (MRI), intestinal ultrasound, and capsule endoscopy (CE) are the main modalities currently used complementary to IC in the diagnostic work-up of CD. Both CE and MRI are well established modalities for evaluating the small intestine.6-8 Their diagnostic accuracy for detecting CD in the colon has not been investigated to the same extend; especially not in the initial work-up of CD. MREC has shown a moderate to high sensitivity for detecting CD in the colon and a good correlation with IC for assessing disease severity in patients with known CD.7, 9, 10 Similar, colonic evaluation with CE is safe with a substantial agreement between CE and IC11, 12 and a high diagnostic accuracy.13 Whether these modalities can replace IC in the future, as the initial diagnostic modality in selected patients with suspected CD is unknown.
The aim of this study was to compare the diagnostic accuracy, feasibility, and patient experienced discomfort with pan-enteric CE and MREC for the initial diagnosis of ileocolonic CD compared to the current standard (IC).
METHODS
Study design and participants
This was a prospective, blinded, multicenter study of the diagnostic accuracy, image quality, and patient experienced discomfort with CE and MREC in patients with suspected CD. The study was conducted in accordance with the STARD 2015 reporting guideline for diagnostic accuracy studies.14
Patients were recruited from three centers in the Region of Southern Denmark managing adult patients with inflammatory bowel diseases. Eligible subjects were ≥16 years of age with a clinical suspicion of CD defined as diarrhea and/or abdominal pain for more than 1 month (or repeated episodes of diarrhea and/or abdominal pain) associated with negative serologic markers for celiac disease, negative stool culture (or polymerase chain reaction) for pathogenic bacteria, a fecal calprotectin >50 mg/kg and at least one additional finding suggesting CD: elevated inflammatory markers, anemia, fever, weight loss, perianal abscess/fistula, a family history of inflammatory bowel disease, or a prior flexible sigmoidoscopy suggestive of CD. Use of NSAID's, renal failure, known gastrointestinal disorder, drug abuse, pregnancy, acute bowel obstruction, implanted magnetic foreign bodies or an IC performed within 3 months prior to inclusion were exclusion criteria (detailed criteria listed in Supporting Information S1 and S2). Patients were enrolled from June 2016 to July 2020. All patients had standardized clinical work-up including medical history, physical examination, bowel ultrasonography, blood samples, IC with biopsies, CE, and MREC within a 2-week period. Patients who failed to undergo IC were excluded from the study.
All examinations were performed by specialists, blinded to the results of the other imaging modalities and findings were reported in a standardized fashion - including whether or not CD was evident.
Diagnostic criteria
IC served as the reference standard for diagnosing CD in the terminal ileum and colon. Clinical information was available to the assessor of the reference standard. CD was defined endoscopically (IC & CE) by the presence of more than three ulcerations (aphthous lesions or ulcers), irregular ulcers/fissures, or stenosis caused by fibrosis or inflammation.6, 15 Stenosis was defined as a luminal narrowing passable (low grade) or impassable (high grade) by the endoscope. For diagnosing CD with MREC, the following findings were evaluated: mucosal ulcerations, bowel wall thickening (≥3 mm), bowel wall hyper-enhancement, diffusion restriction, bowel stenosis, creeping fat, dilated vasa recta, and the presence of an abscess or fistula in conjunction to a diseased bowel segment.16 The diagnosis was based on an overall evaluation of lesions consistent with CD.
MREC
MREC was performed after overnight fasting with a 1.5 T Philips Intera MRI unit (Eindhoven, Netherlands) with Syn-body coil. A total of 1 L of Mannitol 7.5% solution was ingested 1.5 h before the examination. Hyoscine butylbromide 20 mg was administered intravenously in order to reduce artifacts from bowel peristalsis. 15 ml gadoterate meglumine (0.5 mmol/ml) (Dotarem®, Guerbet, Raleigh, North Carolina, USA) was administered intravenously for post contrast assessment. Images were recorded with cor T2, B-FFE, T1, SPIR, axial T1w and diffusion weighted sequences.
The small intestine was divided into thirds (proximal, middle and distal third), and the colon was divided into six segments: cecum, ascending, transverse, descending, sigmoid colon, and rectum. Disease severity was assessed with MaRIA score.10, 17
Pan-enteric CE
CE was performed with the PillCam™ Colon-2 capsule (n = 43) and once commercially available the PillCam™ Crohn's capsule (n = 90) (Medtronic, Dublin, Ireland) after overnight fasting and bowel preparation with 2 + 2 liters of Polyethylene glycol plus ascorbate (Moviprep®, Norgine, Amsterdam, Netherlands) and Sodium Phosphate booster as previously described by European Society of Gastrointestinal Endoscopy.18 Images were reviewed with PillCam™ software v9. The small intestine was divided into thirds by the software. The colon was divided into five segments: Cecum, ascending colon, transverse colon, descending/sigmoid colon and rectum. The right and left flexures were used as landmarks for this subdivision. A complete small bowel evaluation was defined by capsule passage to the colon. Capsule expelled from the rectum defined a complete colon examination. The ileocolonic disease severity was assessed with the Simple Endoscopic Score for Crohn's Disease (SES-CD)19 and disease severity in the small intestine was assessed with the Lewis score.20
Ileocolonoscopy
IC was performed according to standard clinical practice after bowel preparation with sodium picosulfate (Picoprep®, Ferring Pharmaceuticals, Saint-Prex, Switzerland), and type of sedation was recorded (midazolam/fentanyl or propofol). If IC was performed the day after CE, the patients remained on a clear liquid diet and received no further bowel preparation. Complete IC was documented by intubation of the terminal ileum. The length of terminal ileum intubation was estimated and the reason for unsuccessful intubation was recorded. The ileocolonic disease severity was assessed with SES-CD.19
Data management and collection
Study data were collected and managed using REDCap electronic data capture tools hosted at OPEN—Region of Southern Denmark.21 All authors had access to the study data, reviewed and approved the final manuscript. The trial protocol and data underlying this article will be shared on reasonable request to the corresponding author.
Statistical analyses
Based on previous studies by our group using similar inclusion criteria,6 the prevalence of CD was estimated to be 40%–50%. With a prevalence of 50% and a targeted sensitivity of 90%, 70 patients with CD and 70 without CD was needed to achieve a lower limit of the 95% confidence interval (CI) of at least 0.75.22 We aimed to include 150 patients.
Continuous data were summarized using descriptive statistics. The sensitivity, specificity and diagnostic accuracy of CE and MREC for diagnosing CD in the terminal ileum and colon was calculated on 2 × 2 tables. Diagnostic accuracies were compared by area under receiver operator characteristic curve (AUC) and differences in sensitivity and specificity were tested with McNemar's test.23 Due to a small number of discordant pairs, we used the mid-p McNemar's test to obtain the two-sided mid-p-value.24 Sensitivity and specificity analyses for CE and MREC were performed on (1) the total number of patients examined with CE or MREC compared to IC including examinations with segments not fully visualized with CE or IC, and (2) subjects who were examined with all three modalities, had segments fully visualized and no protocol deviation (per protocol analysis). The latter for a direct comparison of CE and MREC compared to IC and test of significance. To assess if misclassification between CD and ulcerative colitis (UC) affects the diagnostic accuracy, a combined variable of both diagnoses was created. CD detected in the small bowel proximal to the terminal ileum was reported as diagnostic yield, and differences were tested for statistical significance in a clustered logistic regression model. Only PillCam™ Crohn's capsules were included in diagnostic yield, due to more reliable small bowel assessment. A non-parametric test was used to compare differences in patient experienced discomfort with CE, MREC and IC with different types of sedation (Wilcoxon matched-pairs signed-ranks test or Kruskal–Wallis test). Statistical analyses were performed using Stata (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC).
Ethical considerations, approvals and registration
The study was conducted in accordance with the principles of the Helsinki declaration and was approved by the local ethics committee of Southern Denmark (S-20150189) and the Danish Data Protection Agency (16/10457). All patients gave informed consent before participation (oral and written). Before inclusion of adolescents between 15 and 17 years of age, both parents and the patient gave informed consent. The study was registered at ClinicalTrials.gov (NCT03134586).
RESULTS
A total of 153 patients were enrolled in the study, and 152 were examined in accordance with the protocol (Figure 1). The study population included 43 males and 109 females with a median age of 27 years (range 16–72). Patient characteristics are shown in Table 1. IC, MREC and CE was performed in 152, 151, 133 patients, respectively. A complete IC and CE was achieved in 130 (85.5%) and 109 (82.0%) patients.
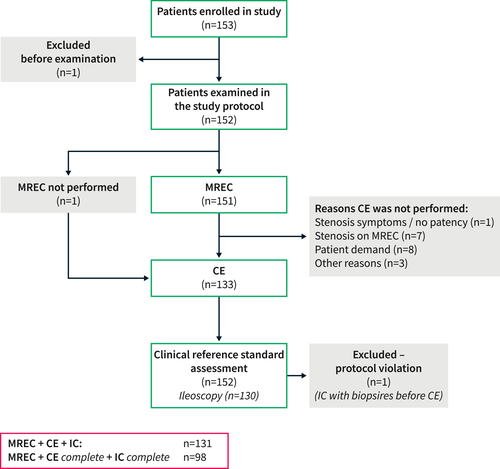
Flow chart showing the number of patients entering the study and completing examinations in accordance with the study protocol
| Gender (n) | Male | 43 | (28%) |
| Female | 109 | (72%) | |
| Age (years) | Median | 27 | |
| Range | 16–72 | ||
| Genetic predisposition (n) | None | 106 | (70%) |
| Crohn's disease | 31 | (20%) | |
| Ulcerative colitis | 15 | (10%) | |
| BMI (kg/m2) | Median | 24.2 | |
| Range | 17.1–57.2 | ||
| Smoking status (n) | Current | 42 | (28%) |
| Former | 23 | (15%) | |
| Never | 87 | (57%) | |
| Duration of symptoms (months) | Median | 6 | |
| Range | 1.0–60 | ||
| Symptoms (n) | Abdominal pain | 148 | (97%) |
| Diarrhea | 75 | (49%) | |
| Weight loss >3 kg | 57 | (38%) | |
| No. of bowel movements | Median | 3 | |
| Range | 1–17 | ||
| C-reactive protein (mg/L) | Median | 12 | |
| Range | 0.2–122 | ||
| Fecal calprotectin (mg/g) | Median | 516 | |
| Range | 51–6000 | ||
| CDAI (responders n = 98) | Median | 167.5 | |
| Range | 20–387 | ||
| Bowel resection before inclusion (n) | 0 | ||
| Non-steroidal anti-inflammatory drugs use (n) | 0 |
Findings
IC diagnosed CD in 59 patients (39%). The Montreal classification is shown in Table 2. In comparison, CE detected CD in 51 (38.4%) patients (terminal ileum 22, colon 7, small bowel and colon 22), and MREC detected CD in 66 (43.7%) patients (small bowel 48, colon 14, small bowel and colon 4).
| n | % | |
|---|---|---|
| A1: ≤16 years | 1 | 2% |
| A2: 17–40 years | 47 | 80% |
| A3: >40 years | 11 | 18% |
| L1: Ileal | 22 | 37% |
| L2: Colonic | 20 | 34% |
| L3: Ileocolonic | 17 | 29% |
| B1: Luminal | 54 | 91% |
| B2: Stricturing | 4 | 7% |
| B3: Penetrating | 1 | 2% |
Diagnostic accuracy for ileocolonic CD
For MREC, the overall sensitivity and specificity for diagnosing CD in the terminal ileum or colon was 67.9% (CI 53.7–80.1) and 76.3% (CI 65.2–85.3)—terminal ileum 76.9% and 85.6%; colon 27% and 93%. For CE this was 87.5% (CI 73.2–95.8) and 87.8% (CI 78.2–94.3)—terminal ileum 96.6% and 87.5%; colon 75.0% and 93.0%. See Table 3 for full details.
| All patients | |||||||||
| n | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | ROC (95% CI) | FP (n) | FN (n) | ||
| Terminal ileum + colon | MREC | 129 | 67.9 (53.7–80.1) | 76.3 (65.2–85.3) | 66.7 (52.5–78.9) | 77.3 (66.2–86.2) | 0.72 (0.64–0.80) | 18 | 17 |
| CE | 114 | 87.5 (73.2–95.8) | 87.8 (78.2–94.3) | 79.5 (64.7–90.2) | 92.9 (84.1–97.6) | 0.88 (0.82–0.95) | 9 | 5 | |
| Terminal ileum | MREC | 129 | 76.9 (60.7–88.9) | 85.6 (76.6–92.1) | 69.8 (53.9–82.8) | 89.5 (81.1–95.1) | 0.81 (0.74–0.89) | 13 | 9 |
| CE | 117 | 96.6 (82.2–99.9) | 87.5 (78.7–93.6) | 71.8 (55.1–85.0) | 98.7 (92.8–100) | 0.92 (0.87–0.97) | 11 | 1 | |
| Colon | MREC | 151 | 27.0 (13.8–44.1) | 93.0 (86.8–96.9) | 55.6 (30.8–78.5) | 79.9 (71.9–86.2) | 0.60 (0.52–0.68) | 8 | 27 |
| CE | 128 | 75.0 (50.9–91.3) | 93.0 (86.1–97.1) | 71.4 (47.8–88.7) | 93.6 (85.7–97.9) | 0.84 (0.76–0.93) | 7 | 7 | |
| Per Protocol | |||||||||
| n | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | ROC (95% CI) | FP (n) | FN (n) | ||
| Terminal ileum + colon | MREC | 98 | 66.7 (48.2–82.0) | 73.8 (61.5–84.0) | 56.4 (39.6–72.2) | 81.4 (69.1–90.3) | 0.70 (0.61–0.80) | 17 | 11 |
| CE | 98 | 90.9 (75.7–98.1) | 86.2 (75.3–93.5) | 76.9 (60.7–88.9) | 94.9 (85.9–98.9) | 0.89 (0.82–0.95) | 9 | 3 | |
| p-value | 0.02 | 0.08 | 0.002 | ||||||
| Terminal ileum | MREC | 113 | 75.9 (56.5–89.7) | 84.5 (75.0–91.5) | 62.9 (44.9–78.5) | 91.0 (82.4–96.3) | 0.80 (0.71–0.89) | 13 | 7 |
| CE | 113 | 96.6 (82.2–99.9) | 86.9 (77.8–93.3) | 71.8 (55.1–85.0) | 98.6 (92.7–100) | 0.92 (0.87–0.97) | 11 | 1 | |
| p-value | 0.04 | 0.82 | 0.029 | ||||||
| Colon | MREC | 98 | 10.0 (1.23–31.7) | 92.3 (84.0–97.1) | 25.0 (3.19–65.1) | 80.0 (70.2–87.7) | 0.51 (0.44–0.59) | 6 | 18 |
| CE | 98 | 75.0 (50.9–91.3) | 92.3 (84.0–97.1) | 71.4 (47.8–88.7) | 93.5 (85.5–97.9) | 0.84 (0.74–0.94) | 6 | 5 | |
| p-value | <0.001 | 0.77 | <0.001 | ||||||
- Note: Sensitivities and specificities are stated in percentages, with the corresponding 95% CI intervals in parentheses. The positive predictive value (PPV), negative predictive value (NPV), area under receiver operator curve (ROC), and numbers of false positive (FP) and false negative (FN) are displayed. The difference in diagnostic sensitivity and specificity was tested for statistical significance and p-values are reported. Per protocol analysis: Patients examined with all three modalities, segments fully visualized and no protocol deviation.
In the per protocol analysis, the sensitivity of CE was superior to that of MREC; especially for colonic disease (p < 0.001). There was no significant difference in specificity (p > 0.08). The AUC of CE was superior to that of MREC for both the terminal ileum and colon.
Proximal small bowel
In the proximal third of the small bowel MREC and CE detected CD in 2 of 151 (1.5%) and 11 of 90 patients (12%), respectively. In the middle third, MREC and CE found CD in 3 of 151 (2%) and 13 of 90 patients (14%). The combined diagnostic yield proximal to the terminal ileum was 4 (3%) and 14 (15.6%) with MREC and CE, respectively (p < 0.01). In 3 cases of complete IC, the terminal ileum was reported normal, but CE detected CD in the proximal small bowel (MREC detected 1 of the cases).
Disease activity
The median SES-CD was 9.0 (range 1–21) with IC compared to 9.5 (range 2–28) with CE, and there was a strong correlation between modalities (Spearman's rho 0.82, p < 0.001). For the small bowel, CE found a mean Lewis score of 1784 (range 225–6060). MREC found a mean MaRIA score for the terminal ileum and overall of 13.7 (range 2.8–28.35) and 15.8 (range 2.8–47.4), respectively. There was a weak correlation between the global MaRIA score and SES-CD with IC (Spearman's rho 0.2, p = 0.2).
Patient experienced discomfort
A total of 106 patients (69.7%) completed the questionnaire. There was no difference between MREC and CE in terms of physical and psychological discomfort (Table 4). Compared to IC, both MREC and CE was associated with less physical and psychological discomfort (p < 0.001). However, when IC was performed with propofol sedation, the discomfort was similar to that of MREC and CE.
| VAS | p-value | |||||
|---|---|---|---|---|---|---|
| Mean (95% CI) | Median | Range | MREC | CE | ||
| Physical discomfort | MREC | 3.6 (3.0–4.2) | 2.75 | 0–10 | N/A | 0.72 |
| CE | 3.4 (2.8–4.0) | 3 | 0–10 | 0.72 | N/A | |
| IC | 4.8 (4.1–5.4) | 5 | 0–10 | 0.00 | 0.00 | |
| Midazolam, fentanyl | 5.2 (4.5–5.8) | 5 | 0–10 | 0.00 | 0.00 | |
| Propofol | 3.6 (2.2–5.0) | 2 | 0–10 | 0.74 | 0.81 | |
| Psychological discomfort | MREC | 2.0 (1.5–2.5) | 1 | 0–10 | N/A | 0.72 |
| CE | 2.1 (1.6–2.6) | 1 | 0–10 | 0.72 | N/A | |
| IC | 3.1 (2.5–3.6) | 2 | 0–10 | 0.00 | 0.01 | |
| Midazolam, fentanyl | 3.2 (2.5–3.8) | 2 | 0–10 | 0.00 | 0.00 | |
| Propofol | 2.6 (1.6 3.7) | 2 | 0–10 | 0.02 | 0.66 | |
- Note: Patients marked visual analog scales for physical and psychological discomfort after each examination. All scales were 10 cm long; 0 cm equaled no discomfort and 10 cm the worst imaginable discomfort. IC is divided into 2 subgroups depending on type of sedation used. The difference between CE, MREC and IC was tested for statistical significance and p-values are reported.
Safety
Four (2.6%) cases of serious adverse events were recorded, and none of these had any lasting consequences for the patients. A 27 years old male with colonic cancer in the transverse colon had capsule retention. The patient did not experience symptoms of retention and subsequently underwent surgery. Three patients were admitted to hospital after IC, MREC and CE, respectively, due to discomfort and abdominal pain. The patients had no signs of bowel perforation or capsule retention. All patients were discharged after 6–8 h of observation.
Additional results
Additional findings and data on image quality are available in Supporting Information S1 and S2.
DISCUSSION
This prospective, blinded, multicenter study is, to the best of our knowledge, the largest study comparing the diagnostic accuracy of MREC and pan-enteric CE in the initial diagnosis of ileocolonic CD. CE was superior to MREC for diagnosing CD in the terminal ileum and colon, and the diagnostic yield was higher for detection of CD in the proximal small bowel. In this population, MREC performed poorly for the colon. Patients' subjective experience of discomfort during MREC and CE was similar and significantly better compared to IC with midazolam/fentanyl sedation but not with propofol.
Visualizing the transmural component of CD (e.g. bowel wall thickening and post contrast enhancement) is a key finding with cross sectional imaging. In the majority of patients, CD often progress from luminal inflammation at the time of diagnosis to complicated disease involving the entire gut wall.25 Therefore, comparing diagnostic studies is limited by spectrum bias, and transferring results from patients with known or complicated CD to patients with suspected or early CD may not be valid. This may explain why MREC performed poorly for the initial diagnosis of colonic CD against an endoscopic reference standard compared to previous studies of patients with known CD.7, 10, 26 This was also shown in the METRIC trial, where the sensitivity of MREC for detection of colonic CD in patients with newly diagnosed CD was inferior to that of patients with known CD—47% and 84%, respectively.7 Another issue could be the chosen diagnostic threshold or difficulty distinguishing between non-specific inflammation, UC, and mild colonic CD. However, we did not find misclassification of the various types of inflammation to have a major impact on the diagnostic accuracy (Supporting Information S1 and S2). In line with the METRIC trial, our results indicate that MREC is not an optimal modality for diagnosing CD in a very early stage due to the low sensitivity for CD located in the colon. MREC is more suited for advanced CD with pronounced transmural inflammation and a higher frequency of disease complications (stenosis or penetrating lesions).
Achieving a complete examination is a common challenge with CE and IC. In this study, capsule excretion per rectum was achieved in 82% of patients, which is comparable to similar studies with suspected or known CD.11, 27 This should, however, be compared to the failure rate of IC (i.e. not intubating the terminal ileum), which was about 14% in our study and comparable to previous studies.6, 28 It should, however, be emphasized, that diagnoses can be made with incomplete examinations if signs of disease are detected.
Another limitation with CE is the technical inability to wash away or aspirate the contents of the colon, and extensive bowel preparation for a good visualization of the mucosa is required. In this study, the bowel cleansing was rated good or excellent in 75% of patients (Supporting Information S1 and S2), which is comparable to other studies.13, 29 Surprisingly, no difference was found in the overall diagnostic performance of CE when stratifying for the bowel cleansing and the overall negative predictive value of a complete CE was 95%. A reason for this could be the presence of multiple or extensive ulcerations in patients with CD detected irrespective of the image quality. This is an important observation and in line with a limited number of studies examining the feasibility of low-volume bowel cleansing regimens.30
Future diagnostic algorithms should strive for minimally invasive and patient-friendly modalities. We found MREC and CE to be equivalent and better tolerated than IC in relation to both psychological and physical discomfort. However, using propofol sedation reduced the discomfort of IC to the same level as MREC and CE. Nevertheless, patients still experience discomfort and optimizing bowel cleansing and contrast regimens can further improve the patient experience.
The ability to detect various types of pathology is important if CE or MREC is used in patients with suspected CD. In this study, almost 10% of patients had UC, and cases of malignancy were detected with MREC and CE, although both modalities misclassified one case as CD (Supporting Information S1 and S2). This is a reminder that atypical presentations should trigger a targeted IC with biopsies, especially in the elderly patients.
Future perspective
Implementing pan-enteric CE as a first-line modality in patients with suspected CD, could reduce the need for IC; changing IC from a first line procedure to a targeted procedure for obtaining biopsies, or if CE is incomplete or contraindicated. Since pan-enteric CE visualizes the entire small bowel, this offers a potential single-examination strategy yielding the total disease distribution—in this study CE found CD proximal to the terminal ileum in 14 of 51 cases with CD on CE. This strategy might be feasible in young patients, who have a low risk of neoplasia. The potential is a rapid and less invasive diagnostic work-up, which is better tolerated and possibly cost-effective.31 Future research should develop new diagnostic algorithms using minimally invasive technology, examine the feasibility of CE as a first-line diagnostic procedure, reduce the time used for CE analysis (e.g. with artificial intelligence), implementing pan-enteric scores,32 and optimize bowel preparation, which will add further potential to this modality. MREC should be reserved for more advanced stages of CD to harvest the full potential of this modality.
Strengths and limitations
We included a clinically relevant population of patients with suspected CD eliminating reader expectation and spectrum bias. An accepted reference standard was applied, and readers were blinded to the results of other examinations. Hence, our results are valid for the first diagnostic work-up of suspected ileocolonic CD. Diagnostic accuracies may not apply to the proximal small bowel. CE and MRI are, however, well established and recommended in the current guidelines for diagnosing small bowel CD.2
An endoscopic reference standard might favor CE over MREC since both IC and CE evaluate the mucosa, whereas MREC primarily evaluate inflammation in the bowel wall. Nevertheless, current guidelines recommend IC as the first line examination,2 and the earliest lesions of CD are believed to arise in the intestinal mucosa.1 With this in mind, we consider IC an appropriate reference standard for the initial diagnosis of ileocolonic CD. We applied a widely accepted but not validated diagnostic criterion for the diagnosis of CD with CE.15 Choosing another diagnostic threshold might have impacted the results. We used 2 types of capsules for CE, and they differs in terms of software and small bowel segmentation. However, this does not affect the ileocolonic evaluation. Findings in the upper and middle third of the small bowel is only presented for the PillCam™ Crohn's capsule.
Experienced gastroenterologists at each participating center performed IC and CE. Variations between multiple observers were not accounted for in this study. A single dedicated abdominal MRI specialist with more than 20 years' experience participated in the study. It is unknown whether the administration of rectal contrast or consensus decision between two or more radiologists would have altered the diagnostic accuracy of MREC. Studies of the inter-observer variation for diagnosing colonic CD with MREC should clarify the latter. A recent study showed a fair agreement in newly diagnosed patients.33
Instead of patency capsule, we primarily used MREC for securing bowel patency. The number of patients examined with CE could be slightly higher, however, if patients with stenosis at MREC had a patency capsule.34
Conclusion
Pan-enteric CE has a high accuracy for diagnosing CD in the small bowel and colon, which is superior to that of MREC. The sensitivity of MREC for diagnosing CD in the colon is poor. Both examinations are better tolerated than IC with conscious sedation. CE could be an alternative to IC as first line modality in selected patients with suspected CD. Future studies on implementation in clinical practice are warranted.
ACKNOWLEDGMENTS
This work was supported by Public grants from the Region of Southern Denmark and Research council Lillebaelt Hospital. Further support was granted from the Danish Colitis and Crohn's association (CCF) to cover travel expenses of the participants.
CONFLICT OF INTEREST
The Authors declare that there is no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




