Efficacy of mirror therapy on lower limb motor recovery, balance and gait in subacute and chronic stroke: A systematic review
Abstract
Objective
Mirror therapy (MT) has been proposed to be an effective therapeutic regimen for lower limb stroke rehabilitation. This review is the first to evaluate the efficacy of MT in subacute and chronic stroke for lower-limb motor functions, balance and gait focusing on particular stage of stroke with specific outcome measures.
Methods
According to PRISMA guidelines, all relevant sources were searched from 2005 to 2020 using “PIOD” framework. Search methods included electronic database, hand and citation searching. Screening and quality assessment was performed by two individual reviewers. Data was extracted and synthesised from 10 studies. Thematic analysis was considered, random-effect models were used and pooled analysis was performed using forest plots.
Results
For motor recovery, MT showed statistically significant effects compared to control group using Fugl-Meyer Assessment and Brunnstorm stages as outcome measures (SMD 0.59; 95% CI 0.29 to 0.88; p < 0.0001; I2 = 0%). Statistical significant improvement was reported for balance in MT compared to control using Berg Balance Scale and Biodex in pooled analysis (SMD 0.47; 95% CI 0.04 to 0.90; p = 0.03; I2 = 0%). When compared with electric stimulation and action-observation training MT showed no signifiant improvement for balance (SMD −0.21; 95% CI −0.91 to 0.50; p = 0.56; I2 = 39%). For gait, MT showed statistical and clinical significant improvement compared to control group (SMD 1.13; 95% CI 0.27–2.00; p = 0.01; I2 = 84%) and when compared to action-observation training and electrical stimulation, presented statistical improvement using 10-m walk test and Motion Capture system (SMD −0.65; 95% CI −1.15 to −0.15; p = 0.01; I2 = 0%).
Conclusion
This review has shown that MT is effective in lower-limb motor recovery, balance and gait in subacute and chronic stroke in patients 18 years or above with no severe cognitive disorder, MMSE score ≥24 and FAC level ≥2. MT could be used for 30 min/day, 5 days/week for 4 weeks, as stand-alone for motor recovery and balance or as an adjunct with electric stimulation for gait for beneficial effects.
1 INTRODUCTION
Stroke is a neurological deficit caused by a vascular injury resulting in disruption of cerebral functions (Sacco et al., 2013; World Health Organization, 1978). Stroke is the second highest cause of morbidity and mortality in the UK, costing NHS £8.9 billion/year, 5% of total NHS costs (Feigin et al., 2003; Saka et al., 2009). Over 60% of stroke patients suffer from persistent disabilities impairing their quality of life (Sutbeyaz et al., 2007). Stroke reduces mobility and causes gait dysfunction in more than half of the survivors due to impaired motor functions and balance (Perry et al., 1995; World Health Organization, 2016). Restoration of mobility and recovery of motor functions are the major aims in rehabilitation (Stevens & Stoykov, 2003) which require therapeutic strategies such as, virtual reality, robotic-interactive therapy, body-supported treadmill training and neuromuscular stimulation (Lee & Lee, 2019). Most of these interventions have proved to be effective but not feasible for general use due to cost and maintenance (Mehrholz et al., 2018), arising the need for user-friendly and cost effective rehabilitation approach ensuring maximum patient participation (Louie et al., 2019).
Mirror therapy (MT) is a simple, low-cost and (Xu et al., 2017) and up-to-date evidence based approach for stroke rehabilitation (Pollock et al., 2014; Rothgangel et al., 2011). MT is a potentially beneficial therapeutic approach (Ramachandran & Altschuler, 2009) which instead of employing somatosensory input like other therapeutic interventions, is based on visual stimulation where patients perceive the mirrored image of their unimpaired limb as the impaired one (Stevens & Stoykov, 2003; Yavuzer et al., 2008), providing feedback substituting for the lost proprioception from the impaired limb (Selles et al., 2014; Thieme et al., 2013). Studies suggest that MT creates a visual feedback of well-functioning limbs, effectively initiating significant recruitment of contralateral primary motor cortex, bilateral somatosensory cortex and supplemental motor cortex aiding functional adaptations and motor recovery (Hung et al., 2015; Liepert et al., 2001; Luft et al., 2002; Muellbacher et al., 2001; Rossiter et al., 2015).
MT was used for the first time by Sütbeyaz et al., in 2007, for the rehabilitation of paretic lower-limbs, and presented statistically significant results (Sutbeyaz et al., 2007). First systematic review on MT for lower-limb rehabilitation included four studies with questionable methodology and weak statistical power to support the results (Hung et al., 2015). Good-quality Randomised Controlled Trials have been published on efficacy of MT on lower-limb with intention-to-treat analysis (Arya et al., 2019; Kawakami et al., 2015; Pandian et al., 2012), blinding and randomisation reducing the risk of bias (Stewart & Parmar, 1996). Statistical significant results were presented by six studies in lower-limb motor recovery with 95% confidence interval (p < 0.05; Arya et al., 2019; Lee & Lee, 2019; Salem & Huang, 2015; Sutbeyaz et al., 2007; Wang et al., 2018; Xu et al., 2017), whereas, there was no significant difference between groups one study (Mohan et al., 2013). Moreover, statistical significant results were recorded in five studies for gait (p < 0.05, CI = 95%; Arya et al., 2019; Ji & Kim, 2015; Lee & Lee, 2019; Mohan et al., 2013; Xu et al., 2017). For balance, significant results were represented by five studies (p < 0.05) in MT groups but non-significant results in between groups (p > 0.05) (Sutbeyaz et al., 2007; Lee & Lee, 2019; Wang et al., 2018; Mohan et al., 2013; Kim et al., 2016a; Lee et al., 2017). Recent reviews and meta-analysis (Broderick et al., 2018; Li et al., 2018; Louie et al., 2019) included studies focusing on lower-limb rehabilitation. However, the reviews have several methodological limitations such as including minimum number of papers with negative results increasing the chance of overstated efficacy of MT (Louie et al., 2019), heterogeneity in results and variability in intervention protocols in terms of not considering specific outcome assessments tools, qualitative analysis in some aspects or aiming for outcome other than gait, balance and motor recovery, effect of MT not distinguished from the supplemental intervention, dissimilarities at baseline, lack of focus on phase of stroke (Li et al., 2018) and lack of generalisation.
The aim of this systematic review was to address the efficacy of lower-limb MT for motor recovery by means of Fugl-Meyer Assessment scale (FMA) and Brunnstorm Stages, balance by Berg Balance Scale (BBS) and Biodex-Balance System and gait by using 10-m walk test (10MWT) and Motion Capture System (MCS), due to high content, criteria and construct validity, good inter and intra-rater reliability, high responsiveness, excellent correlation of the tools with each other and their frequent use in numerous high-quality studies (Bowden et al., 2010; Brandstater et al., 1983; Cachupe et al., 2001; Dawson et al., 2018; Drouin et al., 2004; Hsu et al., 2003; Muyor et al., 2017; Pfister et al., 2014) along with fulfilling ICF conceptual framework that is, body structure, activity and participation for stroke. For post-stroke sensorimotor rehabilitation FMA is used as the standardised protocol (Sullivan et al., 2011), whereas balance and gait are inter-related because the inability of the paretic lower-limb to maintain balance contributes to gait asymmetry (Hendrickson et al., 2014). Emphasis was on sub-acute stage that is, 3 weeks to 6 months (Kiran, 2012), focusing on the dosage of 15–30 min of MT for 4–6 weeks (Thieme, Morkisch, et al., 2018) along with baseline similarities to achieve the effect. Ethical approval for each included study was considered keeping in view that patients were not subjected to any kind of possible harm and benefits outweighed the risks.
2 METHODOLOGY
2.1 Search strategy
According to Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines, systematic search was carried out by two independent reviewers for studies published from 2005 to 2020 on Medical Literature Analysis and Retrieval System Online (MEDLINE), Cumulative Index of Nursing and Allied Health Literature (CINAHL), Cochrane Central Register of Controlled Trials (CENTRAL), PubMed and Physiotherapy Evidence Database (PEDro). Open Gray was searched for unpublished relevant articles. Medical Subject headings (MeSH) and keywords with Boolean Operators were used to search within the titles and abstracts (Appendix 1). Chartered Society of Physiotherapy (CSP), Department of Health (DOH) and National Institute for Health and Care Excellence (NICE) websites were searched for stroke rehabilitation guidelines. Studies referenced in the selected articles or authors in bibliographies were retrieved in citation-search. Frequently referenced journals in literature that is, Neural Repair Journal, British Medical Journal and Stroke were hand-searched. Potentially relevant articles were screened according to the inclusion and exclusion criteria and PIOD framework.
2.2 Priori review
Changes were made in the selection criteria in terms of phase of stroke that is, from sub-acute to sub-acute and chronic (3 weeks to > 6 months) (Kiran, 2012), from efficacy of MT to efficacy of MT and its comparison with other interventions and from inclusion of all outcome measures that is, motor recovery, balance and gait to inclusion of at least one of the outcomes in each paper as very few of papers were available for conducting a systematic review by following the previous criteria.
2.3 Inclusion and exclusion criteria
The revised selection criteria was addressed using “PIOD” framework that is, Population, Intervention, Outcome and Design (Sackett & Wennberg, 1997), utilised as follows (Table 1):
| Inclusion criteria |
| Population |
| Patients (18 years or above) with subacute or chronic stroke, that is 3 weeks–12 months with lower-limb impairement |
| Intervention |
| Studies focusing on Mirror Therapy or MT along with other interventions |
| Outcomes |
| Studies focusing on atleast either one of the outcome measure for motor recovery (FMA or Brunnstorm Stages), balance (BBS or Balance System—Biodex) or gait (10MWT or Motion Capture System) |
| Design |
| Randomised Controlled Trials in English Language |
| Exclusion criteria |
| Population |
| Patients with lower-limb impairment caused by other neurological diseases or inability to comply with study protocol |
| Intervention |
| Studies focusing on interventions other than Mirror Therapy |
| Outcomes |
| Studies focusing on other outcomes measures |
| Design |
| Study designs other than Randomised Controlled Trials and in different languages |
2.4 Data extraction and quality assessment
As per the Cochrane and CRD guidelines, the data was extracted from included studies by Cochrane Data Extraction Form (Chandler et al., 2013; Appendix 2) according to the demographics that is, age, gender, phase of stroke and baseline similarities; frequency and dosage of MT and outcome measures that is, motor recovery, balance and gait (Higgins & Green, 2011). The scales used were Brunnstorm stages or FMA for motor recovery, BBS or Biodex for balance and 10MWT or MCS for gait.
Quality assessment was evaluated by two individual reviewers by using Critical Appraisal Skills Program checklist for RCTs (Critical Appraisal Skills Programme, 2018) to eliminate the bias and add weight to the quality of the review as it suits the method, measures the internal and external validity, ensures relevance of study to practice and its widespread use in various good-quality studies (Armijo-Olivo et al., 2012). The types of risks evaluated for quality assessment are selection bias that is, randomisation and allocation concealment; performance bias that is, blinding; attrition bias that is, incomplete outcome data; reporting bias that is, selective reporting of outcome and other potential bias (Higgins et al., 2011; Appendix 3).
2.5 Data analysis
For assessing the inter-rater reliability between the two reviewers for selection and critical appraisals of studies Inter-coder Kappa statistical test was performed (McHugh, 2012). All RCTs comparing the effect of MT for motor recovery, balance and gait on experimental and control groups were analyzed for the treatment effect. According to Cochrane Handbook for Systematic Reviews (Higgins & Green, 2011) for heterogeneity between trials I2 and Chi2 statistic tests were used and a low p value for Chi2 test provided evidence of heterogeneity. Thematic analysis was considered by identifying, analysing and interpreting meaningful patterns and random-effect model was applied due to methodological differences among studies (p < 0.05 or I2>50%). Fixed-effect model was used where homogeneity existed between the trials and the variation in results was due to random error. Mean Difference (MD) and Standardised Mean Difference (SMD) were used to specify the effect of MT and pooled analysis was performed using forest plots that is, odds ratios (ORs) and 95% confidence intervals. For conducting sensitivity analysis, each study was deleted individually with overall risk of bias to assess the quality and consistency of the results. It determined the extent to which the results were affected by change in methods, variables and dosage of treatment.
3 RESULTS
3.1 Study identification
A total of 182 studies were retrieved from electronic databases and citations search. Following the selection criteria 10 RCTs published between 2007 and 2019 were included in this review (Figures 1 and 2).
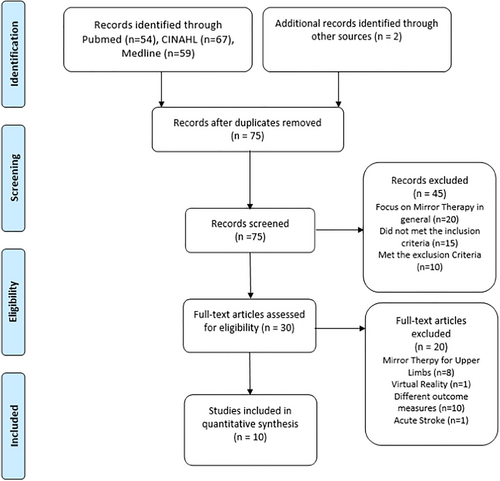
PRISMA flowchart for selection of studies.
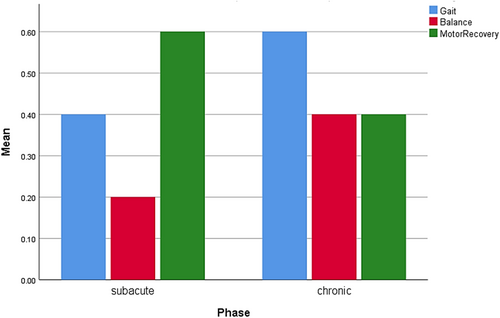
Bar chart of studies characteristic.
3.2 Study characteristics
Forty three participants were included across all 10 studies with sample sizes ranging from 30 (Ji et al., 2014; Lee & Lee, 2019; Salem & Huang, 2015) to 69 (Xu et al., 2017). Five studies focused on subacute stage of stroke (Ji & Kim, 2015; Kim et al., 2016b; Sutbeyaz et al., 2007; Wang et al., 2018; Xu et al., 2017) and five studies focused on chronic stroke (Arya et al., 2019; Ji et al., 2014; Lee & Lee, 2019; Salem & Huang, 2015; Lee et al., 2017). Six studies focused on effect of MT (Arya et al., 2019; Ji & Kim, 2015; Kim et al., 2016b; Salem & Huang, 2015; Sutbeyaz et al., 2007; Wang et al., 2018), whereas 4 studies included supplemental intervention that is, electric stimulation and action-observation training (Ji et al., 2014; Lee & Lee, 2019; Xu et al., 2017; Lee, Kim, Lee). All studies focused on the dosage of 15–35 min of MT for 3–5 days/week for 4–6 weeks (Thieme, Mehrholz, et al., 2018).
3.3 Quality assessment
Inter-coder Kappa statistic test was performed for inter-rater reliability for screening and risk of bias assessment (Carletta, 1996; Viera & Garrett, 2005) presenting the value of 0.86 (Table 2).
| Value | Asymptotic standard errora | Approximate T b | Approximate significance | |
|---|---|---|---|---|
| Measurement of agreement | ||||
| Kappa | 0.867 | 0.122 | 5.229 | 0.000 |
| Number of valid cases | 10 | |||
- a Not assuming the null hypothesis.
- b Using the asymptotic standard error assuming the null hypothesis.
3.4 Efficacy of mirror therapy
3.4.1 Motor recovery
Five out of 10 included studies measured motor recovery in lower-limb (Figure 3). All 5 studies measured motor recovery by Brunnstorm stages (Arya et al., 2019; Salem & Huang, 2015; Sutbeyaz et al., 2007; Wang et al., 2018; Xu et al., 2017), whereas 1 trial used FMA and Brunnstorm stages (Arya et al., 2019). A random-effects model was chosen and there was no significant heterogeneity (I2 = 0%). Pooled analysis showed a significant effect of MT compared to control group (SMD 0.59; 95% CI 0.29 to 0.88; p < 0.0001) (Figure 4).
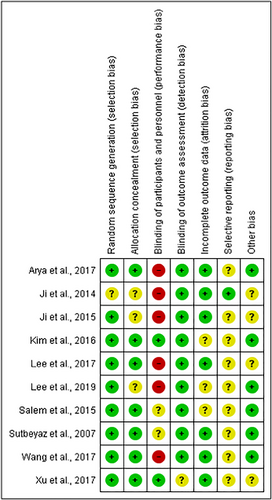
Risk of bias summary for selected studies.
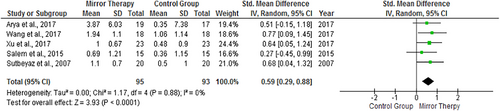
Forrest plot of effect of mirror therapy on motor recovery.
3.4.2 Balance
Three of the included studies measured balance that is, overall stability in functional balance tasks. Two studies used Biodex as an outcome measure (Lee et al., 2017; Kim et al., 2016b) and one study used BBS (Lee & Lee, 2019) for overall balance as dynamic balance moderately reflects functional balance (Hinman, 2000; Parsa et al., 2019). Pooled analysis of the three studies reported significant improvement in overall balance in MT group compared to control group (SMD 0.47; 95% CI 0.04 to 0.90; p = 0.03; I2 = 0%) (Figure 5).
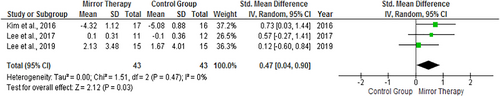
Forrest plot of effect of mirror therapy on balance.
The subgroup analysis of the two studies comparing MT with supplemental intervention that is, electric stimulation and action-observation training (Lee & Lee, 2019; Lee et al., 2017) showed heterogeneity (I2 = 39) with no significant improvements in favour of MT compared to intervention group (SMD -0.21; 95% CI -0.91 to 0.50; p = 0.56) (Figure 7).
3.4.3 Gait
Five out of 10 included studies measured gait that is, walking independence and functional ambulation (Arya et al., 2019; Ji et al., 2014; Ji & Kim, 2015; Salem & Huang, 2015; Xu et al., 2017). Three studies used 10 MWT as an outcome measure (Arya et al., 2019; Salem & Huang, 2015; Xu et al., 2017), whereas two studies used MCS (Ji et al., 2014; Ji & Kim, 2015). Random-effects model was used with evidence of significant heterogeneity (I2 = 84%). Pooled analysis showed significant effect of MT on gait compared to control group (SMD 1.13; 95% CI 0.27–2.00; p = 0.01) (Figure 6).
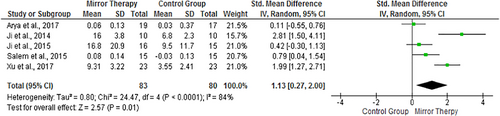
Forrest plot of effect of mirror therapy on gait.
One study compared MT with Action-Observation Training (Lee, Kim, Lee) and another study compared MT with electrical stimulation (Lee & Lee, 2019). The subgroup analysis of the two studies showed significant improvements for MT group (SMD −0.65; 95% CI −1.15 to −0.15; p = 0.01) with no heterogeneity (Figure 7).
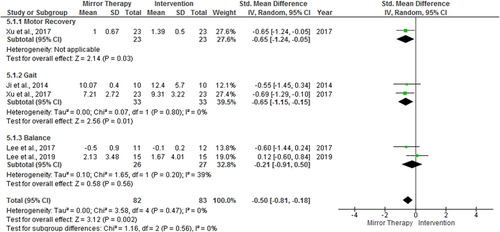
Forrest plot of comparison of effect of mirror therapy and other interventions.
3.4.4 Phase of stroke
Subgroup analysis explored the effect of phase of stroke. Five out 10 studies focusing on subacute stroke showed significant improvements for lower-limb MT for motor recovery, balance and gait (SMD 0.94; 95% CI 0.44 to 1.44, p = 0.0002; I2 = 62%). The other 5 studies with focus on chronic stroke also indicated significant improvements for MT in lower-limb for motor recovery, balance and gait (SMD 0.78; 95% CI 0.17 to 1.39; I2 = 65%) (Figure 8).
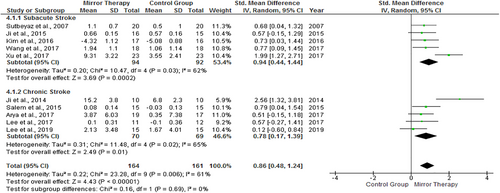
Forrest plot of subgroup analysis on the basis of phase of stroke.
4 DISCUSSION
The aim of this systematic review was to evaluate the efficacy of MT in lower-limb rehabilitation. The primary findings indicated that MT had significant improvement in motor recovery, balance and gait for patients in subacute and chronic stage of stroke. For motor recovery Brunnstorm stages and FMA were used as outcome measures and the pooled analysis showed statistical significant effects for MT compared to control group with SMD = 0.59 and p < 0.0001 (Figure 4) (Arya et al., 2019; Salem & Huang, 2015; Sutbeyaz et al., 2007; Wang et al., 2018; Xu et al., 2017) where SEM = 0.38 (Hsieh et al., 2009) and MCID = 1.9 for FMA and MCID = 6 for Brunnstorm stages (Huang et al., 2016; Pandian et al., 2016; Shelton et al., 2001). Subgroup analysis for motor recovery was not conducted as only one study compared MT to electric stimulation (Xu et al., 2017). Two other reviews also examined MT for lower-limb motor recovery and showed significant improvement at post-intervention assessment in MT group but they did not focus on any specific outcome assessment tool (Broderick et al., 2018; Louie et al., 2019). According to the results, MT could be used as stand-alone treatment for motor recovery with a dosage of 30 min, 5 days/week for 4 weeks.
For gait that is, walking independence and functional ambulation 10 MWT and MCS were used as outcome measures where SEM = 0.04 and MCID = 0.47 for 10 MWT (Perera et al., 2006). The pooled analysis presented statistically and clinically significant results for MT as change in baseline to final score is greater than MCID with SMD = 1.13 and p = 0.01 with heterogeneity that is, variations in intervention protocols among the studies (I2 = 84%) (Figure 6) (Arya et al., 2019; Ji et al., 2014; Ji & Kim, 2015; Salem & Huang, 2015; Xu et al., 2017). Subgroup analysis comparing MT with supplemental interventions that is, electric stimulation and action-observation training showed significant effects for gait with no heterogeneity (Figure 7; Ji et al., 2014; Xu et al., 2017). It has also been reported previously that MT combined with electric stimulation has greater beneficial effects in gait than MT (Li et al., 2018; Louie et al., 2019; Xu et al., 2017). According to the results for gait, MT could be used for 30 min, 5 days/week for 4 weeks as stand-alone or for more favourable effects as an adjunct with electric stimulation.
For balance, BBS and Biodex were used as outcome measures and pooled analysis presented statistical significant improvement in balance in MT group as compared to control group with SMD = 0.47 and p = 0.03 (Figure 5). BBS and Biodex were used together for balance as moderate correlation exist between the two outcomes for overall functional stability in balance tasks (Cachupe et al., 2001; Dawson et al., 2018; Parsa et al., 2019). For BBS, SEM = 1.49 and MCID = 2.7 (Flansbjer et al., 2012; Hiengkaew et al., 2012) and for Biodex, MCID = 2.2 (Cachupe et al., 2001; Hinman, 2000). The subgroup analysis comparing MT with supplemental interventions that is, electric stimulation and action-observation training explored heterogeneity in dosage and frequency of intervention (I2 = 39) and no significant improvements were noted in favour of MT compared to intervention group (Figure 7). The present findings are supported by a review where the results presented significant effect for balance for MT alone but did not find significant effect when compared with electric stimulation (Louie et al., 2019). According to the results for balance, MT could be used for 30 min, 5 days/week for 4 weeks as stand-alone for positive effects.
Results could be generalised with caution for MT in subacute and chronic stroke for motor recovery, balance and gait as samples were representative and quantile (Q-Q) plots presented normal distribution and it should be applicable to wider stroke populations, if met study criteria.
Detailed subgroup analysis of all included studies for phase of stroke showed improvement in motor recovery, balance and gait for both subacute and chronic stage with no heterogeneity that is, no variability of population, outcome measures and phase of stroke; indicating a positive effect of MT on patients aging 18 years or above with no severe cognitive disorder with score of ≥24 on mini-mental state examination and level ≥2 on functional ambulation classification. Regression analysis of included studies was performed for the first time in this review for MT in subacute and chronic stroke and displayed equal variance representing homoscedasticity (Figures 9-11) (Montgomery et al., 2012; Seber & Lee, 2012). Inter-coder Kappa statistic test was performed for risk of bias assessment presenting the value of 0.86 indicating substantial agreement between two reviewers (Table 2) (Park & Kim, 2015; Viera & Garrett, 2005) whereas no other review provided information about the inter-rater reliability.
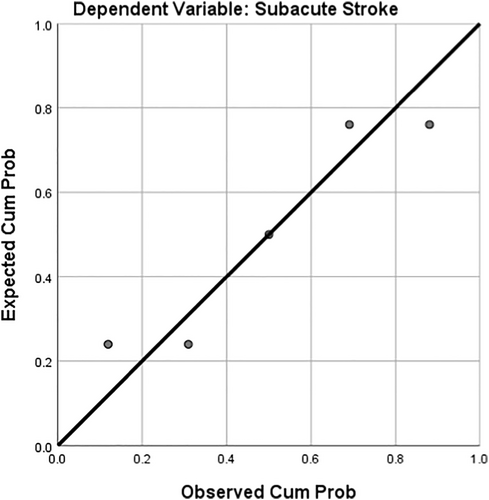
Normal Q-Q plot for subacute stroke.
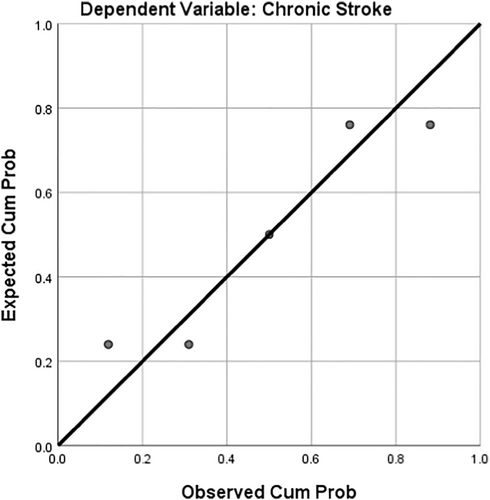
Normal Q-Q plot for chronic stroke.
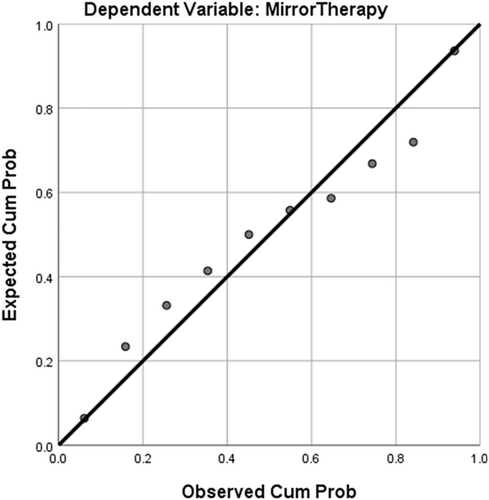
Normal Q-Q plot for mirror therapy.
The studies included in this review focused on the modified dosage protocol by Sutbeyaz et al. (2007), for MT that is, 15–30 min/day, 3–5 days/week for 4–6 weeks for optimal results. The studies using MT for 30 min/day, 5 days/week for 4 weeks presented larger effect in both subacute and chronic phase for motor recovery, balance and gait (Arya et al., 2019; Kim et al., 2016a; Lee & Lee, 2019; Salem & Huang, 2015; Sutbeyaz et al., 2007; Xu et al., 2017) than the studies using MT for 15 min/day, 3 days/week for 6 weeks (Lee et al., 2017; Ji et al., 2014). 30 min of MT for 5 days/week for 4 weeks is the recommended dosage according to this review and the guidelines and might be a potential prospect for future research and clinical implication as it revealed significant statistical and clinical effects for motor recovery, balance and gait.
In this review the dosage used for MT agrees with the dosage stated in the NICE guidelines (recommendation 6.4.2) that is, offer 45 min of relevant stroke-rehabilitation therapy for 5 days/week where functional goals could be achieved. If unable to participate for 45 min, ensure therapy for 5 days/week for a shorter time for active participation (National Institute for Health and Care Excellence, 2019). As per SIGN guidelines (recommendation 4.2.1), when the aim of treatment is to improve gait, motor functions and balance, repetitive task-training with visual feedback should be followed, which ideally describe the methods of MT provided in the studies included in this review (Scottish Intercollegiate Guidelines Network, 2010). MT aids in lower-limb rehabilitation in stroke, supporting the KNGF guidelines (F.2.2) which recommend MT for the paretic limb additional to the regular stroke treatment for beneficial effects (Veerbeek et al., 2014).
The positive findings of this review have significant clinical implications. MT is a safe low-cost therapeutic regimen for stroke which can be performed for 30 min/day, 5 days/week for 4 weeks for statistical and clinical significant results, in sitting or standing with mirror (40 × 70 cm) positioned between the limbs, with non-paretic limb facing the reflective surface providing mirror visual feedback to stimulate mirror neurons system and decrease motor impairment (Dohle et al., 2020; Thieme, Morkisch, et al., 2018). PRISMA guidelines were followed in this review (Liberati et al., 2009), error and bias was controlled by using Cochrane risk assessment tool and inter-coder kappa test was performed for inter-rater reliability (Higgins et al., 2011). This review is the first with prime focus on particular outcome assessment tools for motor recovery, balance and gait where MT proved to be effective in subacute and chronic stroke as stand-alone rehabilitation approach for motor recovery and balance and for more beneficial effects MT could be used as an adjunct with electric stimulation for gait. Recommended outcome measures that presented significant effects in this review are FMA with MCID = 1.9 and SEM = 0.38 (Hsieh et al., 2009) for motor recovery, 10 MWT with MCID = 0.47 and SEM = 0.04 (Perera et al., 2006) for gait and BBS with MCID = 2.7 and SEM = 1.49 (Flansbjer et al., 2012) for balance and could be used by the clinicians for evaluation and assessment.
This systematic review has some limitations. The included studies had small sample sizes and variations of adjuncts were used with MT that is, electric stimulation and action-observation training but as only a few studies deliver these methods and some of the studies being underpowered, combining the results for generalisation to general stroke population becomes challenging. Not all studies measured motor recovery, balance and gait within the specific domains relevant to this review leading to limited number of studies included in pooled analysis. Upcoming research should investigate long-term effect of MT that is, 6 months follow-up, as it was not considered in this review due to limited evidence (Sutbeyaz et al., 2007). Future research should also investigate MT in combination with other modalities that is, electric stimulation and action-observation training to analyse the efficacy. Due to methodological complications that is, small sample sizes and lack of proper reporting, there is need for further high-level evidence on MT with large sample sizes through power calculations, to perceive the minimum number needed for each outcome measure that is, motor recovery, balance and gait, to achieve the expected effect in both subacute and chronic stage of stroke, with follow-up assessments and consideration of intention-to-treat analysis to overcome Type-II Error, and for generalisation of results to general stroke population.
5 CONCLUSION
In conclusion, this review has shown that MT is significantly effective in rehabilitation of lower-limb motor recovery, balance and gait in subacute and chronic phase of stroke in patients 18 years or above with no severe cognitive disorder with score of ≥24 on mini-mental state examination and level ≥2 on functional ambulation classification. MT could be used for 30 min/day, 5 days/week for 4 weeks in subacute and chronic stroke for effective results in motor recovery and balance and in combination with electric stimulation for gait but further research should address the issue of optimal frequency and dosage of MT. According to this review samples were representative and normally distributed and results could be generalised with caution for subacute and chronic stroke for motor recovery, balance and gait. MT could be used as stand-alone treatment for motor recovery and balance or as an adjunct with electric stimulation for gait for favourable effects. FMA, 10 MWT and BBS presented significant effects for motor recovery, balance and gait and are the recommended outcome measures in this review future studies and clinical practice. As only 10 studies were identified in this review, there is need for further high-level evidence on MT with large sample sizes through power calculations to perceive the minimum number needed motor recovery, balance and gait to achieve the expected effect in both subacute and chronic stage of stroke, with follow-up assessments and consideration of intention-to-treat analysis for generalisation of results to general stroke population.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study