Management of neurological problems in children on home invasive mechanical ventilation
Abstract
Introduction
Home invasive mechanical ventilation (HIMV) has become a crucial long-term respiratory support for children with neurological disorders, but requires advanced technological skills and 24-h care. The increasing global population of children on HIMV is attributed to advancements in intensive care and improved survival rates.
Method
The manuscript will review the most common neurological problems encountered in children on HIMV.
Conclusion
The manuscript emphasizes the multidisciplinary nature of managing these patients, involving pediatric pulmonologists, pediatric neurologists, pediatric intensivists, nurses, therapists, dietitians, psychologists, and caregivers. The manuscript outlines the challenges posed by neurological disorders, such as spinal muscular atrophy, muscular dystrophy, cerebral palsy, spinal cord injuries, and neurodegenerative disorders, which may result in respiratory muscle weakness and impaired ventilation. The importance of individualized assessments, appropriate ventilator mode and equipment selection, training of caregivers, airway clearance techniques, nutritional support, regular follow-up visits, psychological and educational support, and addressing specific neurological issues such as involuntary movement disorders, prolonged seizures, sleep disorders, pain, sialorrhea, and immobilization-related complications are discussed. The treatment options for these specific challenges are outlined. This review highlights the complex nature of managing children with neurological disorders on HIMV and the importance of a collaborative approach among healthcare professionals and caregivers to optimize care and improve the quality of life for these children.
1 INTRODUCTION
Home invasive mechanical ventilation (HIMV) plays a crucial role in providing long-term respiratory support for children with neurological disorders affecting respiratory functions.1 It has significantly improved respiratory management, reduced infections, enhanced nutritional and physical status, increased survival rates, and shown various psychosocial benefits.2, 3
Long-term HIMV is a life-support ventilation method that is technically feasible for many children with neurological disorders but requires advanced technological skills and 24-h care.3, 4 Managing neurological problems in children on HIMV requires a multidisciplinary approach involving pediatric pulmonologists, pediatric neurologists, pediatric intensivists, therapists (respiratory, physical, occupational), speech-language pathologists, nurses, dietitians, psychologists, and caregivers.1, 5
The population of children receiving long-term HIMV has been observed to increase worldwide, attributed to advances in neonatal and pediatric intensive care units and improved survival rates of critically ill children.6-8 Family acceptance of HIMV is influenced by significant technical, sociocultural, emotional, and financial factors.2, 9
Neurological disorders can lead to respiratory muscle weakness, reduced lung capacity, and impaired ventilation, making spontaneous breathing difficult or impossible.10 HIMV can be used in the management of various neurological disorders, particularly spinal muscular atrophy, muscular dystrophy, cerebral palsy, brainstem disorders, spinal cord injuries, or progressive neurodegenerative disorders.10-12 Central nervous system (CNS) disorders can trigger respiratory failure through direct involvement of the bulbar respiratory center and a reduction of airway vagal tone, as well as diminished ventilatory response to hypoxia and hypercapnia, possibly caused by dysfunction of aortic and carotid sinus mechanoreceptor transmission or major pulmonary complications such as pneumonia, pulmonary edema, or traumatic pneumothorax.13 Moreover, neuromuscular disorders may lead to the weakness of the bulbar and/or respiratory muscles, causing decreased pressure and flow during inspiration and expiration. Inadequate bulbar and expiratory muscle functions may lead to retained secretions, which are frequently complicated by pneumonia and atelectasis.10, 11
In a recent study, Amin et al. demonstrated that higher mortality rates in children on home mechanical ventilation with both invasive and noninvasive modes were associated with lower income, comorbid neurological impairment, older age, and higher healthcare costs in the year before ventilation initiation.7 Despite this, the number of children with neurological disorders receiving long-term HIMV continues to rise. HIMV can be used for many childhood neurological disorders requiring respiratory support. The major neurological disorders that may require HIMV in children are summarized in Table 1.
| Central nervous system disorders | Neuromuscular disorders |
|---|---|
| Cerebral palsy | Muscular dystrophies (DMD, BMD, CMD, Emery-Dreifuss MD, etc.) |
| Posthypoxic brain damage or posthypoxic leukoencephalopathy | Congenital myopathies |
| Sequelae of stroke | Congenital myotonic dystrophies |
| Sequelae of traumatic brain injury/spinal cord injury | Congenital myasthenic syndromes |
| Malformations of cerebral cortex development | Spinal muscular atrophy (Type 1,2) |
| Congenital central hypoventilation syndrome | Prolonged period of GBS or CIDP |
| Sequelae of viral or autoimmune encephalitis | Metabolic myopathies (Pompe disease, mitochondrial myopathies) |
| Neurogenetic disorders (Joubert syndrome, Prader–Willi syndrome, Down syndrome, etc.) | Hereditary sensory motor neuropathies |
| Neurodegenerative/neurometabolic disorders | Myasthenia gravis |
- Abbreviations: BMD, Becker muscular dystrophy; CIDP, chronic inflammatory demyelinating polyneuropathy; CMD, congenital muscular dystrophy; DMD, Duchenne muscular dystrophy; GBS, Guillain–Barré syndrome; HIMV, home invasive mechanical ventilation; MD, muscular dystrophy.
2 GENERAL MANAGEMENT
2.1 Initial assessment
The initial evaluation of children on HIMV is a critical step in ensuring effective and safe respiratory support for children with chronic respiratory failure. This evaluation typically involves a thorough assessment of the patient's neurological and respiratory status, medical history, and comorbidities.2, 14 Pediatric pulmonologists carefully review the patient's pulmonary function tests, blood gas analysis, and existing ventilator settings. In addition, the evaluation considers the patient's ability to tolerate invasive ventilation mode at home, assessing factors such as caregiver support, individualization of care plans, and the caregiver's understanding of the technology. This comprehensive evaluation tailors the HIMV to the child's specific needs, ensuring optimal respiratory care and improved quality of life. Moreover, creating a safe and clean home environment is vital for infection control measures in all children with or without HIMV.5, 15
2.2 Selection of ventilation mode and equipment and training
Mechanical ventilation modes can be categorized into invasive and noninvasive approaches. The choice between invasive and noninvasive ventilation depends on the severity of respiratory failure, specific medical conditions, and the patient's ability to tolerate different ventilation modes. Invasive ventilation modes include assist control (AC), pressure control (PC), synchronized intermittent mandatory ventilation, volume control (VC), pressure support (PS), and high-frequency oscillatory ventilation (HFOV).16, 17 The AC mode offers a preset tidal volume at a set rate. Children can trigger additional breaths. It is usually preferred in patients with severe respiratory failure, acute respiratory distress syndrome (ARDS), and neuromuscular disorders. The PC mode allows variable tidal volumes depending on lung compliance by maintaining a set pressure during inspiration. It is recommended for conditions requiring precise control over inspiratory pressure, such as neuromuscular disorders or ARDS. The SIMV mode combines forced breaths with the option for patients to breathe spontaneously between machine-assisted breaths. It is used under various conditions, particularly during the weaning process from mechanical ventilation. The VC mode maintains a constant volume, providing a set tidal volume with each breath. It is employed various conditions requiring control over tidal volumes, such as neuromuscular disorders or postoperative care. The PS mode assists spontaneous breathing by providing a preset pressure level during inspiration. It is often used during the weaning process, providing support during spontaneous breaths. The HFOV mode provides very fast and small tidal volume breaths at high frequency. It is applied in patients of severe respiratory failure and conditions with low lung compliance, such as those with ARDS or neuromuscular disorders.16-18 On the other hand, noninvasive ventilation modes include continuous positive airway pressure, bilevel positive airway pressure (BiPAP), and volume-assured pressure support. Noninvasive ventilation modes, especially BiPAP, can provide support for respiratory muscle weakness in conditions associated with neuromuscular disorders.16-19
When selecting ventilation equipment for children on HIMV, several factors should be considered to ensure both safety and effective respiratory support. The choice of specific equipment may vary based on the child's age, weight, and underlying medical condition.16, 17 It is crucial to ensure that the selected ventilator offers the necessary ventilation modes to meet the child's respiratory needs. Consideration should be given to the size and weight of the ventilator, as well as its portability. A preference should be given to a compact and lightweight device that facilitates easy transport. In addition, the ventilator should feature appropriate alarms and safety mechanisms, encompassing alerts for low and high pressure, low tidal volume, disconnection, and battery status. Safety mechanisms should be in place to prevent excessive pressures that could harm the child's airways. Given that HIMV often requires humidification to prevent airway drying, it is advisable to choose a ventilator that integrates well with humidification systems suitable for children. Furthermore, a ventilator with monitoring capabilities, which provides real-time data on the patient's ventilation parameters, may be preferable. These data can be invaluable for healthcare professionals, allowing for comprehensive review and assessment.17, 20
Selecting the appropriate mechanical ventilation mode is crucial for optimizing outcomes. HIMV settings must be tailored to the child's needs and underlying neurological disorders. Healthcare professionals are responsible for training caregivers on how to use the ventilator effectively and safely. This training includes troubleshooting common issues and understanding the signs of respiratory distress or equipment malfunction. Caregivers should also be educated about potential complications and when to seek medical assistance. Preparing a well-defined emergency plan is crucial. Caregivers should know when and how to seek immediate medical attention.8, 11, 21 In a recent prospective cohort study, Wynings et al. identified risk factors for tracheostomy accidental decannulations in 67 pediatric inpatients. This study revealed that the most common cause of tracheostomy accidental decannulation was due to patient movements (32%).22 Therefore, we suggest that accidental or patient-induced decannulation may be more prevalent in children with neurological diseases, particularly those with hyperkinetic movement disorders such as choreoathetosis and dystonia. This unfortunate event may lead to severe hypoxic-ischemic encephalopathy and a poor prognosis. It is crucial to alert caregivers about this potential unexpected situation and to provide them with education on basic resuscitation techniques.
2.3 Airway clearance techniques
Children with neurological disorders, especially those with severely affected neuromuscular diseases with bulbar muscle weakness, may encounter challenges in effectively clearing secretions from their airways, leading to an increased risk of respiratory infections. Airway clearance techniques, such as chest physiotherapy, cough assist devices, and suctioning, are essential for preventing respiratory infections in children on HIMV. Chest physiotherapy is a set of techniques designed to improve respiratory function by promoting airway clearance. It is often individualized based on the patient's specific needs, underlying medical condition, and ability to perform techniques. Airway clearance techniques can be subdivided into proximal (cough augmentation) or peripheral (secretion mobilization) methods.23 Chest physiotherapy techniques for airway clearance include manual approaches such as postural drainage, chest percussion, and vibration. In addition, devices play an important role with options such as high-frequency chest wall oscillation (HFCWO) devices, positive expiratory pressure (PEP) devices, and intrapulmonary percussive ventilation (IPV). Inclusion of breathing exercises, such as deep breathing exercises and directed cough techniques, can also contribute to effective airway clearance.24, 25
HFCWO devices use external forces, such as air pulses or mechanical vibrations, to loosen and mobilize mucus. PEP devices generate resistance during exhalation, thereby promoting the maintenance of positive pressure in the airways. This method helps to keep the airways open and facilitates effective mucus clearance. IPV delivers a series of small, rapid air bursts to the lungs during both inhalation and exhalation, enhancing airway clearance. These various techniques and devices contribute to a comprehensive chest physiotherapy approach aimed at optimizing respiratory function.26
2.4 Nutritional support
Many neurological disorders may affect a child's ability to swallow, leading to weight loss and malnutrition. Children on long-term HIMV typically require assistance with feeding. Ensuring proper nutrition and hydration is critical for maintaining overall health and supporting respiratory functions. In a prospective cohort study, Martinez et al. evaluated the nutritional and metabolic status of 20 children with or without neuromuscular disorders receiving long-term home mechanical ventilation and found that most children had malnutrition, altered metabolic status, and suboptimal macronutrient intake.27 CNS disorders characterized by excessive involuntary movements, such as dystonia and severe choreoathetosis, can lead to an increased need for caloric intake. Regular assessment of malnutrition in children on HIMV is important to reduce preventable complications.
2.5 Follow-up visits
Regular monitoring of the child's respiratory status, nutrition, growth, and development is crucial. Follow-up visits with the general pediatrician, pediatric pulmonologist, and pediatric neurologist are critical to evaluate the effectiveness of ventilation, manage potential complications, and specify the care plan. Regular communication and collaboration between healthcare professionals and caregivers are essential to provide the best possible care for children on HIMV.2, 28, 29 Moreover, the use of telemedicine in children on home invasive or noninvasive mechanical ventilation may be a feasible tool to avoid face-to-face visits during the pandemic.30
Weaning off home mechanical ventilation is possible in children with certain subtypes of neuromuscular disorders, such as congenital myopathies and myasthenia. In addition, advancements in gene or gene-based therapies have shown promising results, allowing a small number of patients with spinal muscular atrophy to be weaned off home mechanical ventilation in recent years.31 Improvement of the underlying neuromuscular condition and increased muscle strength through proper nutrition can facilitate this situation.11, 32
2.6 Psychological and educational support
Managing a child with neurological disorders on HIMV can be emotionally challenging for both the child and caregivers. In a recent study evaluating patients on long-term mechanical ventilation with four phases of care: intensive care unit, respiratory care center, respiratory care ward, and respiratory home care, family caregivers of patients receiving respiratory home care reported the highest level of stress.33 Providing psychological support and counseling to both patients and caregivers are critical components of the overall care plan. Particular attention should be given to preventing caregiver burnout, and measures should be taken.34-36 Moreover, Mattson et al. emphasized the importance of regular measurement and assessment of quality of life in children and adolescents on home mechanical ventilation to provide person-centered care.37 Note that educational support is particularly critical for children on HIMV with and without significant intellectual impairment. Children on HIMV should be encouraged to attend school and integrate into their communities as much as possible.
3 MAIN NEUROLOGICAL PROBLEMS AND SPECIAL MANAGEMENT
From a pediatric neurology perspective, managing neurologically ill children on HIMV presents multiple challenges. Figure 1 summarizes the main neurological issues and special treatments commonly observed in pediatric neurology practice for children on HIMV. Among patients with CNS disorders, movement disorders are a significant problem, especially in children with conditions such as hypoxic-ischemic encephalopathy and neurodegenerative disorders. Involuntary movements, including dystonia and choreoathetosis, may increase the risk of accidental decannulation.22 Furthermore, children with these movements often experience gastrointestinal absorption and motility disorders, which limit caloric intake despite their increased energy consumption, leading to failure to thrive and malnutrition. Treating these children with involuntary movements requires the critical use of antidystonic therapies. Pharmacological agents, including baclofen, benzodiazepines, gabapentin, clonazepam, and trihexyphenidyl, are favored for treating dystonia. In patients resistant to pharmacotherapy, alternatives such as botulinum toxin injections and deep brain stimulation may be considered preferred interventions. The treatment of choreoathetosis in children depends on the underlying cause, including genetic, metabolic, or neurological disorders, and autoimmune conditions. These treatments include pharmacological interventions, including dopamine-depleting agents such as haloperidol or pimozide, dopamine-receptor blocking agents such as risperidone and olanzapine, benzodiazepines such as clonazepam, antiseizure medications such as valproic acid and carbamazepine, and tetrabenazine.38-41
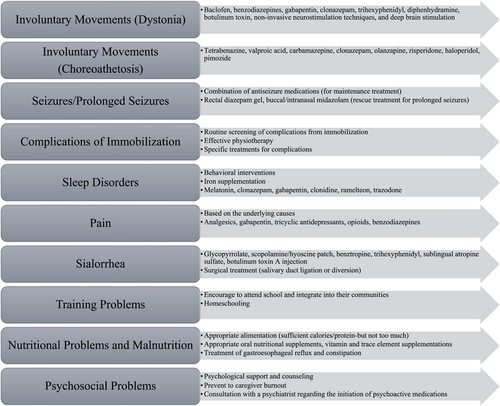
Another significant issue in children on HIMV is seizures, which pose a major challenge in children with hypoxic-ischemic encephalopathy, malformations of cerebral cortex development, and progressive neurodegenerative disorders. In the acute treatment of prolonged seizures or seizure clusters, the use of rescue antiseizure medications, such as rectal diazepam gel or buccal/intranasal midazolam, may help prevent progression to status epilepticus.42 Many children require a combination of multiple antiseizure medications, leading to increased sedation or sialorrhea, which can be critical problems for children on HIMV. Addressing sialorrhea may involve the use of treatments such as glycopyrrolate, scopolamine/hyoscine patch, benztropine, trihexyphenidyl, sublingual atropine sulfate, or botulinum toxin A injection.43, 44 Maintaining good oral hygiene is crucial for the management of sialorrhea. A regular dental check-up can identify any issues associated with excessive drooling, such as dental caries and malocclusion. In pharmacoresistant patients, surgical procedures, such as salivary duct ligation, may be considered to decrease saliva flow.45 Moreover, the use of certain antiseizure medications, including phenytoin, valproate, carbamazepine, and oxcarbazepine, might also have a deleterious effect on osteopenia in immobilized children and requires careful evaluation and treatment to avoid bone fractures.46, 47
Children on HIMV with neuromuscular disorders face significant challenges because of immobilization resulting from hypotonia and muscle weakness. Immobilization often leads to decreased muscle strength and atrophy, contractures, osteopenia, bone fractures, and an increased risk of venous thromboembolism, particularly in severe patients of early onset weakness, such as spinal muscular atrophy type 1.48, 49 Prolonged immobilization can lead to decreased cardiac output, orthostatic hypotension, impaired respiratory functions, pressure ulcers, alterations in glucose metabolism and insulin sensitivity, risk of urinary tract infections and urolithiasis, and immunosuppression.50 In addition, children with Duchenne muscular dystrophy using steroids are at a high risk of osteopenia and bone fractures.51 Regular physiotherapy to prevent complications from immobilization and routine screening for these complications are crucial in their management. Moreover, cardiomyopathy is a major concern in muscular dystrophies and mitochondrial diseases because it further limits patient mobility.52 The decision to consider advanced therapies, such as implanting a ventricular assist device in patients with Duchenne muscular dystrophy, involves collaboration among pediatric neurologists, pediatric cardiologists, and pediatric intensivists.53 This decision is challenging because of many limitations, including scoliosis, malignant hyperthermia, circulation problems such as deep venous thrombosis, and the risk of advanced contractures.52, 53
Sleep disorders are prevalent among children on HIMV, especially those with CNS disorders.54 While there is a substantial body of data on sleep hygiene in children on home noninvasive mechanical ventilation, limited information is available for children on HIMV. Sleep disturbances resulting from spasticity, pain, gastroesophageal reflux, seizures, and involuntary movements can significantly reduce the quality of life in children with neurological disorders on HIMV. It is crucial to address the underlying causes. Treatment for sleep disorders may involve various approaches, including behavioral interventions such as establishing a consistent bedtime routine, creating a comfortable sleep environment, and limiting stimulating activities before bedtime, and pharmacological interventions such as iron supplementation, melatonin, benzodiazepines, clonidine, gabapentin, ramelteon, and trazodone.55, 56
Managing pain caused by neuropathic pain, dysautonomia, visceral hyperalgesia, hip subluxation, joint deformities, contractures, muscle spasms, osteoporosis, gastroesophageal reflux, and constipation is another complex issue for children on HIMV.57 Pain can significantly reduce the quality of life for these patients and induce stress for both patients and their caregivers. Treatment for pain is based on the underlying causes and may involve the use of analgesics, gabapentin, tricyclic antidepressants, opioids, or benzodiazepines.57
4 CONCLUSION
The management of neurological problems in children on HIMV requires a coordinated and holistic approach. It is essential to remember that each child's situation is unique, and care management should be tailored to their specific needs. Regular communication and collaboration among healthcare providers and caregivers are crucial for achieving the best outcomes for these children.
AUTHOR CONTRIBUTIONS
Yavuz Sayar: Conceptualization; writing—original draft; formal analysis; validation; methodology; writing—review editing. Miraç Yıldırım: Conceptualization; investigation; writing—original draft; formal analysis; writing—review editing; validation. Serap Teber: Conceptualization; supervision; writing—review editing.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. Data available on request because of privacy/ethical restrictions.