Home ventilation in low resource settings: Learning to do more, with less
Abstract
Long-term ventilation (LTV) in children at home, especially invasive ventilation, is not widely available nor practised in low-resource settings (LRS). Barriers to providing LTV include underdeveloped pediatric critical care services, limited expertise in pediatric LTV, limited capacity to screen for sleep-disordered breathing (SDB) and high cost of LTV equipment and consumables. Additional challenges encountered in LRS may be unreliable electricity supply and difficult socioeconomic conditions. Where LTV at home has been successfully implemented, caregivers and families in LRS must often take full responsibility for their child's care as professional home-based nursing care is scarce. Selecting suitable children and families to offer LTV in LRS may therefore face difficult ethical decisions when families are disempowered or incapable of providing 24-h care at home. Early caregiver participation and hands-on training in tracheostomy care and LTV equipment is key to success, irrespective of the caregiver's level of education. The use of overnight oximetry, mobile phone technology, spirometry, and clinical evaluation are simple tools that can aid recognition and monitoring of children needing LTV. As children survive longer supported by LTV, engaging with adult services at an early stage is important to ensure suitable pathways for transition to adult care are in place. Building capacity and expertise in pediatric LTV in LRS requires targeted training of health professionals in related disciplines and advocacy to policymakers and funders that LTV in appropriately selected circumstances is worthwhile, life-changing, and cost-saving.
1 INTRODUCTION
With advancements in medical technology and life-saving interventions, there is a growing need worldwide for pediatric long-term ventilation (LTV) at home, including in low-middle-income countries (LMIC) with scarce resources. Although the global trend is more children being initiated on noninvasive ventilation (NIV) at a younger age for all indications, there is continued need for invasive LTV via tracheostomy in a smaller proportion of children in whom NIV is not possible or unsuccessful.1 More children are surviving critical illness and becoming dependent on medical technologies, which is shifting the burden of care from the hospital to the home and community. This transition requires considerable resources and expertise, which are scarce in low-resource settings (LRS). The estimated population prevalence rates of all-cause home LTV in 24 high-income countries (HIC) ranges between 1.2 and 47/100,000 people, with higher rates reported with increasing gross domestic product in countries.2 The minimal cost of supporting home LTV through equipment, services and maintenance was calculated in one study to be a conservative 3400–5928 €/patient/year, which is one of the major barriers to expanding home LTV and LRS.2 Nevertheless, the numerous advantages to patients, and families and limited hospital care resources compel care providers of children in LRS to find cost-effective solutions that enable LTV at home.3 Although guidelines and recommendations for pediatric LTV have been published, they are more suitable for HIC settings where there are resources to follow these guidelines.4, 5 In this review, we highlight the current status of pediatric LTV at home in LRS across the world with a focus on invasive LTV. Further, we discuss the challenges of implementing LTV in LRS and provide some alternative solutions for overcoming these barriers.
2 CURRENT STATUS OF LTV AT HOME IN LRS
The provision of LTV, invasive or noninvasive, is highly variable and inconsistent in LRS (Table 1). Although published reports may not represent the true picture, the type, and indications of home LTV in LRS depend on available resources, expertise, local practice preferences and availability of private healthcare insurance and providers. Apart from the initial expense of procuring and servicing LTV equipment and consumables, expertise and organized, dedicated pediatric multidisciplinary LTV care teams are scarce in most LMIC. The availability and access to pediatric critical care facilities and expertise is usually a prerequisite for implementing and supporting a home LTV program, especially for invasive LTV. In two recent scoping reviews, the severe shortage of pediatric critical care resources and lack of adequately trained heath care professionals, including nurses, has highlighted the significant need worldwide for more pediatric critical care in LMIC where the burden of disease of severe illness is significantly greater15, 16 The highly variable rate of invasive home LTV reported in LMIC (8%–100% of LTV cohorts) is likely to be strongly determined by availability of supporting pediatric critical care facilities in the same settings (Table 1).
| Author, year | Country | N | Age of initiation | LTV initiated in ICU | Underlying disorders | PSG? | Proportion (%) NIV/invasive | Mortality |
|---|---|---|---|---|---|---|---|---|
| Basa, 20206 | Serbia | 105 | 6.2 y (0.3–18 years) 13 y (NIV; 18 months (invasive) |
NR | NMD 75%, respiratory 9%, CCHS 6%, OSA 7% | NR | 48/52 | 25% |
| Nathan, 20177 | Malaysia | 70 | 11 months (range 5–33 months 0 | NR | Respiratory 55%, NMD 10% | NR | 86/14 | 14% |
| Van der Poel, 20178 | South Africa | 55 | 3.5 y (0.4–17.6) | 65% | NMD 60%, CCHS 5%, other 35% | Yes, 11% | 16/39 | 38% |
| Yanaz, 20229 | Turkey | 416 | 10 months (invasive) 41 months (NIV) |
NR | NMD 35%: other neurological 26% | NR | 49/51 | NR |
| Leske, 202010 | Argentina | 244 | 9.4 y (range 3.4–14) | 9% | NMD 43%, genetic syndromes 23%; neural tube defects 9%; CCHS 4%, other 21% | Yes, 70% | 86/14 | 5% |
| Kinimi, 202011 | India | 57 | 6.4 y (range 3 months–17 y) | 17% | NMD 68%, | Yes, 65% | 12/88 | Nil |
| Hassani, 201912 | Iran | 67 | 5.2 y (range 2 months–15 y) | 100% | Congenital airway malformations 35%; severe laryngomalacia 28%. NMD 28% | None | 92/8 | Nil |
| Borges, 202013 | Brazil | 27 | 4.0 y (±3.9 y) | 100% | Cerebral palsy 37%, NMD 22%, genetic syndromes 18%, other 22% | No | 0/100 | 48% |
| Sriboonyong, 202314 | Thailand | 15 | Range 3 months–5.6 y | 100% | Severe tracheomalacia | No | 0/100 (CPAP via tracheostomy) | 20% |
- Abbreviations: CCHS, congenital central hypoventilation syndrome; ICU, intensive care unit; LTV, long-term ventilation; NIV, noninvasive ventilation; NMD, neuromuscular disorder; NR, not reported; PSG, polysomnography.
Children who will benefit from LTV are typically identified through several different clinical pathways: first, by failure to extubate or wean off prolonged mechanical ventilation in the intensive care setting following acute illness or postoperatively; second, surveillance for obstructive sleep apnea (OSA) and/or alveolar hypoventilation through elective polysomnography (PSG), polygraphy, or oxycapnography studies in at-risk groups such as children with neuromuscular disorders (NMD); and third, with clinical indications or complications in at-risk patients such as declining spirometry forced vital capacity (FVC) < 40% predicted in NMD, abnormal blood-gas analysis, pulmonary hypertension, recurrent pneumonia or atelectasis and day-time symptoms of sleep-disordered breathing (SDB) such as early morning headaches, poor sleep quality and day-time exhaustion.5, 17 Similar to pediatric critical care, access, and expertise to PSG or other basic SDB screening technologies is extremely limited or absent in many LMIC, even for adults where there is little consistent high-quality data on the epidemiology of SDB.18 As a consequence, the need for invasive LTV programs for children may arise following prolonged mechanical ventilation of children with underlying congenital disorders such as NMD or congenital abnormalities who present in crisis with unrecognized late complications of SDB such as chronic respiratory failure or pulmonary hypertension.8 In these situations, prolonged intensive care admissions place significant strain on already overstretched resources which provides a compelling argument and need to support the expansion of home LTV programs in LRS. The capacity and expertise to provide pediatric NIV in various forms (e.g., bubble continuous positive pressure and high flow oxygen therapy) in acute care is rapidly increasing and becoming more widespread in LRS. These technologies and expertise will hopefully have a knock-on effect in laying the foundation to support the expansion of LTV programs in LRS.19, 20
3 OVERCOMING OBSTACLES TO LONG-TERM VENTILATION IN LOW-RESOURCE SETTINGS
3.1 Recognizing children who need LTV and screening for sleep-disordered breathing
Recognizing children who need LTV in LRS where access to PSG is severely limited, requires a composite assessment of a patient's risk, clinical criteria, and alternative screening tests. Clinical and lung function surveillance can inform who would best benefit from the scarce resource of PSG and/or empiric LTV. The first step is to identify the child at risk; then undertake relevant clinical and screening tests to inform who requires confirmatory testing as summarized in Table 2.
| Identify child at risk | Clinical screening and tests | Confirmatory test |
|---|---|---|
| Obstructive sleep apnea:
|
Clinical:
|
|
| Alveolar hypoventilation: | Clinical:
|
|
| Neuromuscular disease
|
||
| Hypoxia awake/daytime.
|
- Abbreviations: EEG, electroencephalogram; OSA, obstructive sleep apnea; PSG, polysomnography.
Overnight oximetry is a very useful screening test for severe SDB, with a good positive predictive value.21-23 It is relatively widely available in LRS and should be advocated for as an important diagnostic tool. Respiratory criteria for sleep oxygenation have been recommended for initiation of LTV (minimum oxygen saturation SpO2 ≤ 90%, >2% recording time SpO2 ≤ 90%, 3% oxygen desaturation index >1.4 events/hour, apnea hypoxia index (AHI) > 10 event/hour).5 This is particularly helpful for children with variable upper airway obstruction as a cause of their respiratory failure. Other available screening tool useful in LRS is to get a home video of the symptoms when child asleep. This can be done as video or audio on a mobile phone.
For children at risk of hypoventilation carbon dioxide (CO2) should be monitored. If neither PSG, capnography nor transcutaneous CO2 monitoring are available, daytime arterial blood gas (done with appropriate care: age-appropriate explanation to child, topical anesthetic, skilled phlebotomist) is useful. For hypoventilation due to NMD lung function with spirometry, maximal inspiratory pressure (MIP), maximal expiratory pressure (MEP), and/or cough peak flow, should be monitored at least annually. Children with FVC < 50% or daytime CO2 ≥ 45 mmHg, symptoms of nocturnal hypoventilation, or recurrent respiratory infections, should have overnight oximetry.24 NIV during sleep is indicated for children with chronic respiratory failure (daytime pCO2 > 6.7 kPa/50 mmHg) with or without symptomatic nocturnal hypoventilation.
3.2 Empowering and preparing families/caregivers for LTV and patient-centered care approach
In contrast to most HIC supporting families with LTV at home through professional home-based nursing care is rarely possible in LRS, unless privately funded. Although unsupported by evidence, strong recommendations by the American Thoracic Society that an awake and attentive trained caregiver be in the home of a child requiring LTV at all times are equally valid in LRS.4 In addition to this, one of the most important prerequisites for considering invasive LTV at home in LRS settings is that the caregiver(s) and/or extended family must be able and willing to provide full-time care on a 24-h basis. Ironically, the lack of trained professionals for home care is one of the most common reasons cited in HIC for delays in discharging children from hospital to home. Delays ranging between 2 months (United States), 6 months (Canada), and up to 10 months (UK) have been directly attributed to a lack of home nursing care.25-27 In contrast, median time to home discharge in South Africa for invasively ventilated children, a setting without home-based nursing care, was 3 months (range 8–991 days).8 Equipping caregivers with the technical skills and confidence to provide full-time care of their technology-dependent child may add a significant burden to already stressful social and financial circumstances, but if appropriate selection criteria are applied for eligibility of LTV, it can be empowering to caregivers, regardless of socioeconomic circumstances or education.8
3.3 Selecting patients and families eligible for LTV at home in LRS
The indications and eligibility for LTV at home in LRS will vary considerably depending on local expertise and available resources. In broad terms, they can be categorized as patient-related, caregiver and home environment-related, and program-related (Box 1). In conditions where resources are very constrained, selecting children with more favorable outcomes and who have adequate home environments, over children with less favorable outcomes, inadequate or unsafe home environments will be inevitable. Difficult decisions need to be made by multidisciplinary clinical teams, which may lead to the withdrawal of life-supporting care and active palliation. Neuromuscular conditions presenting beyond infancy, either congenital or acquired, represent the largest group with the most favorable outcomes and should be prioritized for LTV in LRS. Unlike HIC, bronchopulmonary dysplasia in preterm infants is an uncommon indication for invasive LTV in LRS, where the morbidity and mortality in preterm infants is high due to limited access to neonatal intensive care.28
Box 1. Recommended minimum conditions to implement invasive LTV in low-resource settings
-
Quality of life with underlying condition or diagnosis can be substantially improved with LTV (e.g., congenital NMD), or underlying condition may improve over time (e.g. Guillain Barre’ syndrome).
-
Quality of palliative and comfort care can be substantially improved with incurable end-of life conditions (e.g., brain tumor).
-
Ventilation is required ≥ 12 h per day, and NIV is contraindicated, failed or not secure (e.g., infants with CCHS or congenital NMD).
-
At least one reliable, trainable caregiver who is able to provide full-time care at home. Subsequent training of other household members or lay carers is strongly recommended.
-
Cohesive family support network to support primary caregiver emotionally and financially.
-
Basic sanitation, running water and ablution facilities in the household.
-
A reliable electricity supply with an additional external power source to recharge external batteries.
-
Access to reliable telephone or mobile phone for emergencies and communication with healthcare providers.
-
A multidisciplinary team with expertise in tracheostomy care and LTV. Nurse-led LTV programs are preferred but not essential.
-
Access and availability of pediatric intensive care facilities.
-
Reliable supply and maintenance services of suitable pediatric LTV ventilation equipment and consumables, including humidifiers, provided either free to families who can't afford it or procured through health insurance schemes where available.
-
Technical support and backup services for maintenance of equipment and consumables.
Legend: CCHS, Congenital Central Hypoventilation Syndrome; LTV, long-term ventilation; NMD, neuromuscular disease.
Compared with NIV, invasive LTV in the home setting is more expensive in terms of equipment and consumables (i.e., ventilators, humidifiers, and circuits), requires accompanying tracheostomy care and suction devices, and additional caregiver training in emergency measures. Social determinants are often important barriers to invasive LTV. Factors such as uninterrupted electricity supply and whether the caregiver(s) are able to provide full-time 24-h care at home are important factors when considering the feasibility of invasive LTV in LRS. Caregivers who are employed may be forced to resign from their positions which adds significant financial burden on families, more so in LRS where they may be the main breadwinners in the household and social assistance programs are less supportive.
3.4 Solution-focused approach and preparing caregivers for LTV at home
Once the indication and need for invasive LTV is identified in child, a stepwise process that begins to engage and prepare caregivers and their extended family is required to establish feasibility and potential barriers for invasive LTV within the family's unique circumstances and resources. Understanding the caregiver and family's insight of their child's condition and medical needs is important, especially in LRS, where levels of basic literacy, education, and medical knowledge may vary widely. Allowing the caregiver and family to express their personal experience and journey with their sick child facilitates open, honest discussion about the future care of their child and the impact it will have on their family. Including the family at the outset of the LTV journey empowers them to face their difficult new reality, and in turn, identify skills, strengths, personal and familial qualities, and beliefs, that will guide the family in finding what capacity they have to cope with LTV at home. With appropriate preparation and guidance in committed families, it is unusual that LTV at home cannot be accomplished, even with very basic home conditions (Figure 1).8 “De-medicalizing” the lives of children and families requires more than technical training. Caregivers need to gain the confidence to take on the challenge of LTV, and mobilize their own family and community resources with the assurance of ongoing support of a multidisciplinary LTV team.

3.5 Tracheostomy care
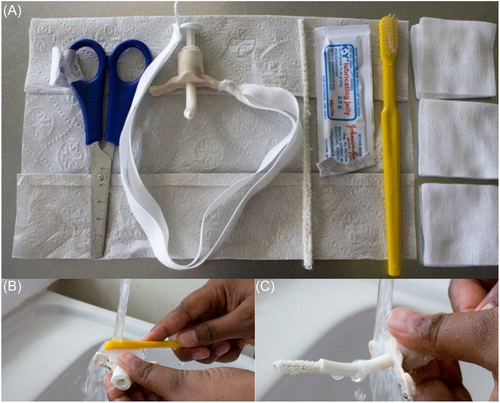
Tracheostomy care practice and protocols vary widely across the world. A recent multicenter survey of the International Pediatric Otolaryngology Group (IPOG) in North America and Europe reported responses from members in four areas: in-patient teaching, homecare, evaluation, and management of tracheitis, and surveillance endoscopies.29 The conclusion of this survey was that practices and opinions varied widely despite published guidelines. Factors that often influence practices are health insurance requirements and family resources. For example, the recommended frequency of tracheostomy changes reported in the IPOG survey was highly variable: 25% recommend changes twice per month, 25% recommend changes at least every 1–2 months; 8% recommend weekly changes, while others based frequency on type of tracheostomy or proximity to the hospital.29 Examples of innovative and successful tracheostomy care practices do exist in LRS and provide evidence that a tracheostomy should not present a barrier to LTV at home in LRS. A long-standing tracheostomy home care program in South Africa adopted unique practices which include training caregivers to do daily tracheostomy tube changes and re-use two tracheostomy tubes on a rotational basis; simple cleaning techniques with soap, pipe-cleaners, and toothbrush; and simple taping techniques to prevent dislodgement (Figure 2). Daily tracheostomy tube changes equip caregivers with confidence and competency to change the tracheostomy tube in all situations and have the added advantage of preventing sudden life-threatening tracheostomy occlusion or tracheitis that can result from the accumulation of biofilm material in the tracheostomy lumen.30 A study from this South African center of 157 (16% receiving LTV) children discharged home with tracheostomies between 2008 and 2012 reported low mortality (1.2%) and increased risk or unplanned admissions within 1 year in families with a history of substance abuse and household cigarette smoke exposure.31 An example of an innovative manual for caregivers on information and training on tracheostomy and LTV can be downloaded at this website (chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/http://breatheasyprogramme.org/uploads/6ba5c67c361fb06ba9c67c3f/1442588335920/Home-Care-Book-final-email.pdf).
3.6 Home LTV equipment and consumables
The technology requirements for LTV will depend on patient-specific needs, the underlying diagnosis and time required per day on the ventilator.2 Modern home ventilators for either NIV or invasive LTV range from simple, less expensive bi-level pressure-cycled devices to more expensive sophisticated multi-modal pressure and volume-cycled ventilators designed for longer or continuous LTV. Consumables include single-limb circuits with expiration outlets, appropriate patient interface connections, and humidifiers with accompanying automated temperature regulation systems. Humidification of the airway is essential with invasive LTV as it prevents dehydration of the airway mucosa and secretions, which may cause life-threatening complications such as obstruction and infections. Heated humification systems have better outcomes compared to heat and moisture exchangers but are more expensive, require electricity, and are more complex to operate.32
Modern home ventilators have a lifespan of 5–7 years if maintained well but the ongoing expenses of consumables such as air filters, circuits, and humidification must be factored into the overall costs. Although not recommended by the manufacturers, using less expensive bi-level devices for invasive LTV is feasible in some circumstances, such as delivery of CPAP in children with severe tracheomalacia or LTV in young children with severe muscle weakness disorders where chest wall compliance is very high.14 However, bi-level devices generally do not have built-in batteries and, therefore, will not operate if there is an interrupted or unreliable power supply. Ensuring uninterrupted power supply in LRS is one of the more difficult challenges and barriers in providing LTV at home in LRS. The inclusion of manual resuscitator bags is mandatory in most LRS due to the high risk of unpredictable interruption of power supply. Similarly, providing manual suction devices is equally important. Modern re-chargeable external backup batteries can provide up to 8-h of power during electricity outages but add significantly to the overall costs. The COVID-19 pandemic sparked renewed interest in designing low-cost (USD 700) basic home ventilators in countries like India.33 Although data and experience are lacking, children needing LTV in LRS could stand to benefit in the future from similar advances in technology.
3.7 Transitioning safely from hospital to home
It is essential that, before LTV being initiated, the family undergo an in-depth interview detailing the family composition and broader support. This helps the healthcare worker to learn about the child's family and community and what the family understands about what the doctors have told them regarding their child's condition. This process is key to the eventual safe transition home. Caregiver counseling is ongoing and an important part of the preparation and training. The primary carer should be with their child in the hospital while the LTV is successfully established so they can be adequately trained, learning about the equipment, the multidisciplinary care, and troubleshooting. This ensures too that there is time to identify the various community networks that will replicate the hospital care team once they are home. The caregiver training must include training in emergency care and response; it is essential that discharge planning includes printed emergency numbers and action plans to keep easily at hand. To adequately plan for safe discharge, a home visit is recommended. This will assist the family through the logistics of how home ventilation will work. For example, a guaranteed power supply is essential and may require batteries and/or a generator, certain necessary home modifications may be identified for action. Transition planning must include considerations of transport, carer support, multidisciplinary community care support, schooling, and communication with local health facilities. A checklist inclusive of equipment (considering specific household needs like electrical outlets and extension cords, portability, humidification, oximeter, and alarm settings), training needs, essential carer competencies, and discharge planning steps should be completed before discharge; an example is included in supplementary material. This ensures that no important steps are missed and that all communication has been clear. Completing a detailed patient-specific care plan (text and pictures) that includes an explanation of the child's condition, details of the ventilation support, how to manage complications, and clear emergency plans should be completed and be given in paper and electronic form to the primary carer. It can, in addition, be shared with the community care teams and school. Follow-up appointments are important for monitoring family adherence and patients' quality of life. Community follow-up may be needed if there are complicated intercurrent issues or missed appointments. Careful and consistent case management of a child on LTV managed at home is essential for safety and success. Any homecare ventilation program must identify who in the team is responsible for coordinating care; and updating and communicating multidisciplinary plans between the healthcare team, family, and community networks.
3.8 Social determinants impacting quality of life
Without professional help in the home setting, families in LRS must often make difficult lifestyle and financial decisions and adjustments to their lives to care for their children on LTV. There is good evidence from both HIC and LMIC settings that Health-related Quality of Life is reduced in caregivers and children on LTV.3, 34-36 In addition, increased mental health and sleep disturbances are reported in caregivers with children on LTV.37-39 The high demands related to the care of children on LTV children therefore pose a significant risk factor for triggering poor mental health outcomes in caregivers and their families. Careful evaluation and screening for potential stressors in the family and social environment is necessary as part of the decision-making to establish the feasibility of LTV, especially if there are pre-existing mental health or substance abuse disorders 3.9 Training care providers and building professional capacity for home LTV programs.
Apart from the expense of LTV equipment and consumables, a lack of professional expertise and experience is a major obstacle to advancing pediatric LTV at home in LRS. Specialized pediatric nursing and Advanced Nurse Practitioners (ANP) are more established professions in HIC but are frequently poorly implemented or unsupported by regulation in LMIC.40 Evidence for higher patient satisfaction, improved chronic disease outcomes, and cost-effectiveness with ANP compared to medical practitioner-led care exist in primary, secondary, and specialist care settings involving both adult and pediatric populations.41 In the absence of ANP or specialized LTV nursing career pathways, multi-disciplinary teams caring for children needing LTV can build expertise and capacity through short courses or training modules such as this example in South Africa: (https://health.uct.ac.za/childrensnursingunit/teaching/short-courses/nursing-children-tracheostomy).
4 TRANSITION TO ADULT CARE: ENGAGING ADULT SERVICES
With early diagnosis and supportive interventions, an increasing number of children with NMD are surviving into adolescence and adulthood.42 This has led to a growing need to engage with adult services to facilitate the transition of care for this particularly vulnerable group of patients. Ideally, a successful transition program should address the medical, psychosocial, emotional, and educational needs of the individual.43
Planning for transition should begin in early adolescence, with the choice of adult services dependent on the underlying condition and the availability and locality of services.42 This is often a barrier in LRS where home LTV programs for adults may not be established.2 Further, the financial burden to families of health services in caring for technologically dependent adults is an important consideration when planning for transition and ensuring appropriate care, including access to welfare support if needed.2, 44 Key steps in ensuring a successful transition from pediatric to adult services include establishing standardized management protocols to facilitate the process and prevent adverse outcomes.45
Early planning and staged transition with all specialists, healthcare, and community providers, together with the family and adolescent collaborating, is a useful strategy to follow.43 Identified facilitators of successful transition include early discussions and active planning, which may need to begin up to 2 years before the planned transition; joint pediatric-to-adult home ventilation clinics; written information on adult services and training the adolescent in communication skills in order for the individual to communicate and advocate for their health needs, without a caregiver necessarily present.43 Barriers to successful transition may include lack of referral to other medical specialists, beyond the home ventilation program team; developmental delay or disability of the adolescent, and lack of information on adult community funding structures and access to this.43 Importantly, discussions on ethical decisions such as the need for ongoing or escalating ventilatory support and end-of-life decisions should also be addressed in the transition process.42
5 ETHICAL ASPECTS OF PEDIATRIC LONG-TERM HOME VENTILATION IN LOW-RESOURCE SETTINGS
Long term ventilation at home in LRS is fraught with difficult ethical challenges. While there is considerable evidence that LTV optimizes use of healthcare resources is a cost-effective and provides mental and emotional benefits and independence for patients and their families, there are often significant barriers and ethical considerations that need overcoming before embarking on this course of treatment.42 Equity of access to treatment is a global issue and is dependent on local resources. While the burden of home care may be significant, local experience has shown that it is feasible even in significantly constrained socioeconomic settings.8
Decision-making around LTV is usually on a case-by-case basis, and utilizing a standardized framework may assist in the challenging decision making around the process.46 Depending on the underlying medical conditions necessitating LTV, the goal is either to “bridge” the patient to recovery or definitive treatment whereby LTV is no longer required; or “destination” therapy whereby there are no further recovery or definitive treatment options, and LTV is a permanent therapy.46 Important considerations in the decision-making process include the patient and family wishes, and this may provide challenges in terms of overlapping interests of the patient and the parents, especially if the child is unable to voice their thoughts. The impact on the family and siblings and the burden of care must be considered in the planning process.42, 46
Public health needs and priorities, access to LTV services, and the principle of distributive justice are important considerations. The potential access to novel therapies including disease-modifying gene-therapy for SMA-type 1, further complicates the decision-making process46 While these therapies are less accessible in LRS due to high cost, the future potential to access of these will become increasingly important in ethical decisions.
Palliative care, defined by the World Health Organization as improving the quality of life of patients with life-threatening illnesses and their families, is important for patients receiving LTV, even if the end of life is not imminent. In children receiving LTV for complex medical conditions, the main goals of palliative care are achieving the best quality of life through alleviating physical and psychosocial distress, understanding the needs of children and their families, and providing adequate end-of-life care.47 A multi-disciplinary team, family-centered approach, with open communication is vital in achieving this.47
6 CONCLUSION
Although access to pediatric LTV at home is not widely available in LMIC, lessons learned from existing programs in LRS provide useful evidence and guidance on how to implement LTV programs when resources are constrained. The main obstacles to achieving broader access to LTV in children are limited or absent pediatric critical care facilities, the inability to screen at-risk children for SDB, and the high cost of mechanical home ventilators and consumables. When resources are scarce, selecting appropriate children and families to offer LTV may encounter difficult ethical decisions. In LRS, where no LTV programs exist, children continue to suffer with premature morbidity and mortality relating to their underlying conditions. Advocating to policymakers, health facility managers, and healthcare funders that LTV in children is worthwhile to improve their quality of life and save costs by keeping children out of hospital is important.
AUTHOR CONTRIBUTIONS
Jane Booth: Writing—review & editing (supporting). Diane M. Gray: Writing—original draft (supporting); writing—review & editing (supporting). Aneesa Vanker: Writing—original draft (supporting); writing—review & editing (supporting).
CONFLICTS OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.